You’re standing in the kitchen, maybe reaching for a pan or draining pasta, and suddenly there’s that searing, white-hot flash of pain. Your brain screams "hot!" before your nerves even process the damage. In those first few seconds, you’re frantically wondering if you need an ER or just a cold cloth and some aloe. Looking at pictures of 1st 2nd and 3rd degree burns online often feels like a gamble because, honestly, real-life injuries aren't always as "textbook" as the medical diagrams make them out to be.
Most people assume they can tell the difference immediately. They think a little redness is fine and a blister is the end of the world. But skin is a complex organ, the largest one you've got, and how it reacts to thermal energy depends on a dozen different variables like contact time and the source of the heat.
The Subtle Warning Signs in First-Degree Burns
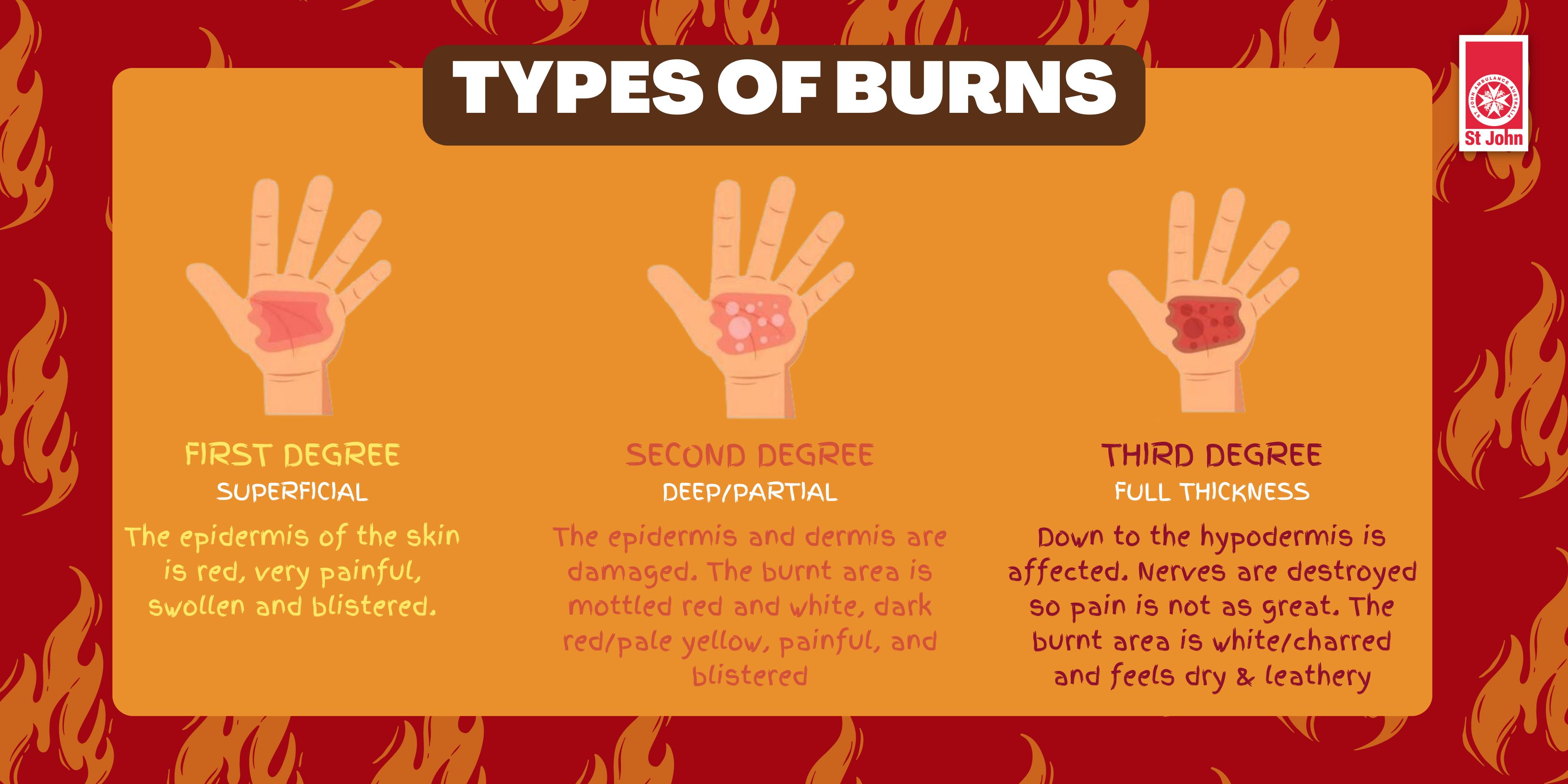
A first-degree burn is essentially the "entry-level" of skin trauma, but don't let the name fool you into thinking it's always minor. Technically, this is a superficial burn. It only affects the epidermis, which is that thin, protective outer layer of your skin.
When you look at pictures of 1st 2nd and 3rd degree burns, the first-degree examples usually just look like a bad sunburn. The skin is red. It’s dry. It’s painful to the touch. One of the clearest ways to identify this is the "blanching" effect. If you press your finger onto the red area and it turns white for a second before rushing back to red, you're likely looking at a first-degree injury.
There aren't any blisters here. That’s the big differentiator. If you see a bubble, you’ve moved up a level.
Usually, these heal in about 3 to 6 days. The skin might peel—a process called desquamation—as the damaged cells slough off to make room for the fresh stuff underneath. It’s annoying and it stings, but it rarely leaves a scar. However, if a first-degree burn covers a massive portion of your body, like your entire back or both legs, it can actually cause systemic issues like dehydration or a low-grade fever.
Moving Into the Danger Zone: Second-Degree Burns
This is where things get messy. A second-degree burn, or a partial-thickness burn, goes past the surface and starts chewing into the dermis. This is the layer that holds your sweat glands and hair follicles.
When you browse pictures of 1st 2nd and 3rd degree burns, the second-degree ones are the most distinct because of the blisters. These blisters are the body's way of creating a "biological bandage." Inside that bubble is serum, a fluid that leaks out of damaged capillaries to protect the raw dermis underneath.
Why Texture Matters More Than Color
In a "superficial" second-degree burn, the skin looks moist and weepy. It’s incredibly painful because the nerves are exposed and firing like crazy. But there is a "deep" version of the second-degree burn that is much more dangerous.
In deep partial-thickness burns, the skin might actually look white or waxy. It might not even hurt as much as the superficial ones because the heat has started to stun or damage the nerve endings. This is a trap. People see a white, non-painful patch and think they're fine, when in reality, the damage has gone deeper than the screaming red areas.
👉 See also: That Nagging Aching Feeling in Chest: When to Worry and What’s Likely Just Gas
According to the American Burn Association, any second-degree burn larger than three inches in diameter, or anything located on the face, hands, feet, or genitals, needs professional medical eyes on it immediately. Infection is the big enemy here. Once that blister pops—and it usually does—you have an open highway for bacteria to enter your bloodstream.
The Deceptive Silence of Third-Degree Burns
Here is the most counterintuitive thing about severe injuries: third-degree burns often don't hurt at the center.
When you examine pictures of 1st 2nd and 3rd degree burns, the third-degree (full-thickness) category looks terrifyingly "dead." The skin might be charred black (eschar), or it might look like a piece of stiff, white leather. It can even look brown or tan.
Because the burn has traveled through the epidermis and the dermis into the subcutaneous fat layer, it has effectively incinerated the pain receptors. You’ll feel intense pain around the edges of the wound where the burn is "only" second-degree, but the center is often numb. This is a medical emergency of the highest order.
👉 See also: What to Eat When You Have a Stomach Ache: The Foods That Actually Help
The Physical Changes
- Leathery Texture: The skin loses all elasticity.
- No Blanching: If you press on a third-degree burn, it doesn't turn white. The blood vessels are gone.
- Swelling: Known as edema, this can be so severe that it cuts off circulation to a limb (which might require a procedure called an escharotomy to release the pressure).
You won't see blisters on a third-degree burn because the tissue is too damaged to even hold fluid in that way. It’s just... gone. Healing this requires skin grafts because the local "repair shops" in your skin (the hair follicles and glands that help regrow tissue) have been destroyed.
Beyond the Basics: The Rarely Discussed Fourth Degree
While most people stop at three, medical professionals often categorize even deeper injuries as fourth-degree burns. These go through the skin and fat and into the muscle or bone.
In pictures of 1st 2nd and 3rd degree burns, you won't typically see these because they are often the result of high-voltage electrical shocks or prolonged exposure to intense flames. The area looks charred and "skeletonized." At this point, the risk isn't just a scar; it’s the loss of the limb or organ failure as the body tries to process the toxic byproducts of destroyed tissue.
How to Actually Use This Information
Knowing the difference is about more than just curiosity. It's about triage.
If you or someone else is burned, the very first step—before you even look at a picture—is to stop the burning process. Cool water, not ice. Ice can actually cause "frostbite" on top of a burn, further damaging the tissue by restricting blood flow when the skin needs it most.
Quick Triage Checklist
- Is it just red? Keep it clean, use aloe or a light moisturizer, and keep it out of the sun.
- Are there blisters? Do NOT pop them. Popping a blister is like opening the door for an infection. Cover it loosely with sterile gauze.
- Is the skin white, black, or numb? Call 911 or go to the ER. Don't stop to put ointment on it. Ointment can actually trap the heat inside the tissue and make the burn worse while you're driving to the hospital.
One detail experts like those at the Mayo Clinic emphasize is the "rule of nines." Doctors use this to calculate how much of the body is affected. For an average person, the entire arm is about 9%, the head is 9%, and the torso is 36%. If you’re looking at your injury and it covers a significant "percentage" of your body, even if it looks like a first-degree burn, you need to see a doctor because of the risk of shock.
Real-World Healing and Scarring
The aftermath of looking at pictures of 1st 2nd and 3rd degree burns is the reality of the recovery. First-degree burns vanish. Second-degree burns can leave "hyper-pigmentation" (dark spots) or "hypo-pigmentation" (light spots) that might last for years. Third-degree burns will always scar, often with "contractures" where the new skin is so tight it limits your movement.
Modern medicine has come a long way, though. We now have synthetic skin, silver-impregnated bandages that kill bacteria on contact, and advanced pressure garments that help minimize scarring.
What to do right now if you've been burned
- Remove jewelry immediately. Fingers and wrists swell fast. If you don't get that ring off now, a doctor might have to cut it off later.
- Skip the home remedies. No butter. No toothpaste. No lard. These are old wives' tales that actually introduce bacteria and trap heat.
- Hydrate. Your skin helps regulate your body's fluids. When it's damaged, you lose water through evaporation much faster than normal.
- Check your Tetanus shot. Burns are dirty injuries. If it's been more than 5 years since your last shot and you have a second or third-degree burn, you likely need a booster.
The visual difference between these injuries is your roadmap for action. Pay attention to the texture and the pain level, not just the color. If the wound looks dry and leathery or if you see underlying structures like fat or muscle, skip the Google search and head straight to a trauma center. Your skin is your primary defense against the world; once that's compromised, speed is the only thing that preserves function and minimizes the long-term impact on your life.