You wake up, swing your legs over the side of the bed, and the moment your feet hit the floor, it feels like you've stepped directly onto a bed of jagged glass. That sharp, stabbing pain in your heel is the hallmark of plantar fasciitis. For veterans, this isn't just a "foot ache." It's often the result of years spent in heavy combat boots, carrying 80-pound rucksacks, or running miles on unforgiving asphalt. Getting va disability for plantar fasciitis is something many veterans overlook because they think it's just "part of the job." It isn't.
Pain matters.
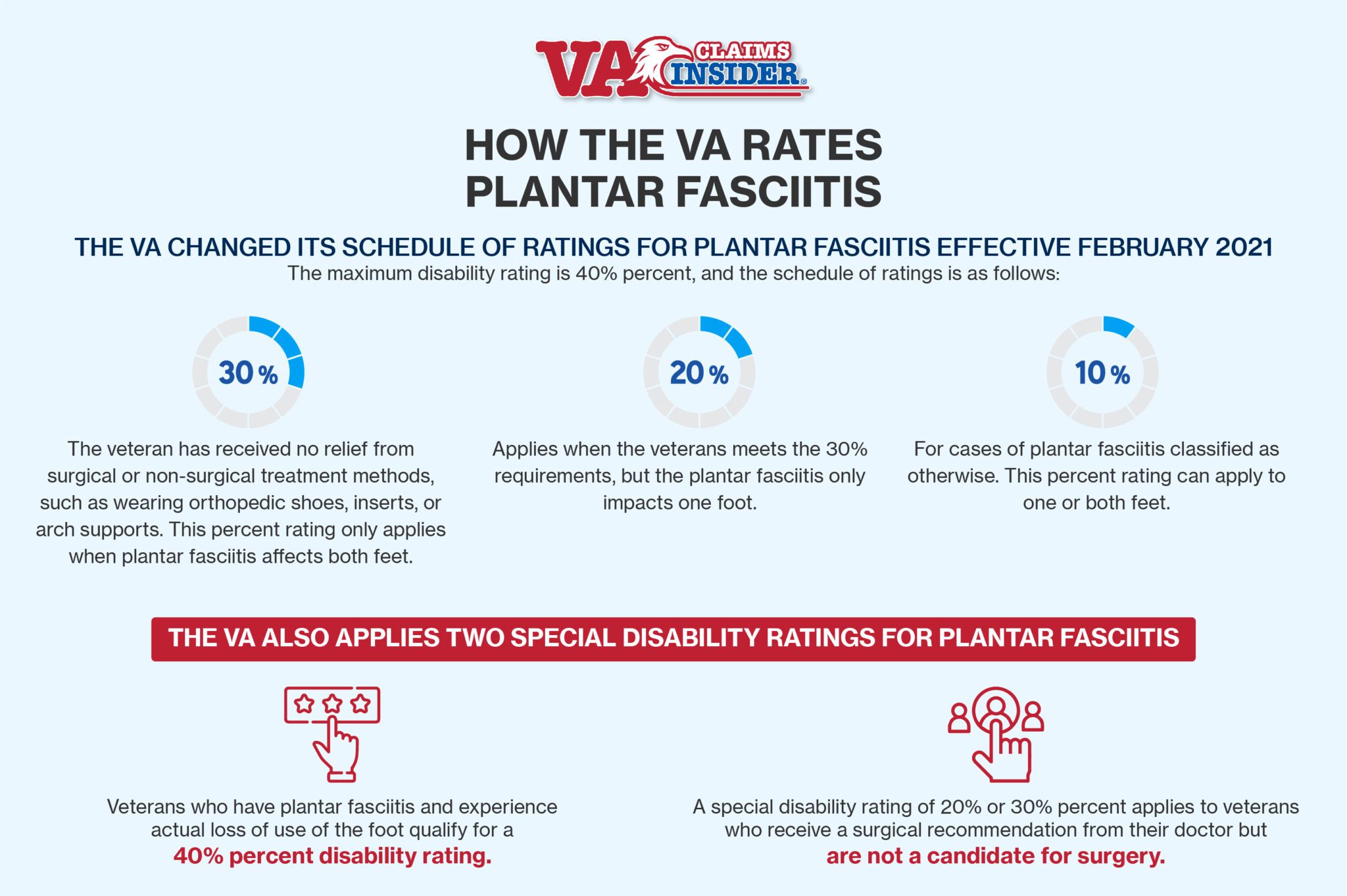
The VA recently overhauled how they evaluate foot conditions, which changed the game for everyone filing a claim. If you haven't looked at the 38 CFR § 4.71a schedule of ratings lately, you're probably looking at outdated info. They used to lump everything together, but now there's more nuance. Or at least, there's supposed to be.
The Reality of the 2026 Rating Schedule
Let's be real: the VA doesn't make this easy. You can't just walk in, say "my feet hurt," and expect a check. You need a nexus. You need a diagnosis. Most importantly, you need to show how it messes with your life.
Under the current diagnostic code 5269, the ratings for va disability for plantar fasciitis generally fall into three buckets: 10%, 20%, and 30%. If you have it in one foot and it’s manageable with those cheap store-bought inserts, you’re looking at 10%. If it’s in both feet (bilateral) and it’s "unresponsive to treatment," that’s usually where the 30% kicks in. But there's a catch. To hit that 30% mark, the VA typically wants to see that you've tried everything—physical therapy, custom orthotics, maybe even those painful steroid injections—and you're still limping.
They look for "loss of use." Can you stand for an eight-hour shift? Probably not if your fascia is screaming. Do you have to sit down every twenty minutes? That's the kind of detail that wins claims.
Why Your "Service Connection" Is Often Rejected
Most veterans get denied because they can't bridge the gap between their time in service and their current pain. You might have left the Army in 2008 and didn't file until 2024. The VA rater is going to look at that 16-year gap and assume you just got old or wore bad shoes.
You need the paper trail.
If you didn't go to medical while you were active duty because you didn't want to be labeled a "sick bay commando," you've got a mountain to climb. But it's not impossible. This is where buddy letters come in. Your old squad leader remembers you limping after that 12-mile march. Your spouse sees you clutching the dresser every morning just to stand up. These personal statements fill the gaps that the official medical record missed.
Honestly, the "nexus letter" is your best friend here. A doctor—preferably a podiatrist who knows the VA system—needs to write down the magic words: "at least as likely as not." This means there is a 50% or greater chance your military service caused or aggravated your condition. Without those words, your claim for va disability for plantar fasciitis is basically dead on arrival.
Secondary Conditions: The Multiplier Effect
Plantar fasciitis rarely travels alone. When your feet hurt, you change how you walk. You start "favoring" one side. You shift your weight. Suddenly, your knees start popping. Your hips feel out of alignment. Your lower back starts spasming.
This is called "secondary service connection."
If you already have a rating for a knee injury, and that knee injury caused you to walk funny, which then caused plantar fasciitis, that’s a claim. Or, conversely, if your service-connected plantar fasciitis causes degenerative disc disease in your spine because your gait is completely trashed, you can claim the back pain as secondary to the feet.
It's a domino effect.
The C&P Exam: Don't "Tough It Out"
The Compensation and Pension (C&P) exam is where most claims go to die. Veterans are conditioned to be tough. When the doctor asks, "How are you doing today?" the instinctual response is "I'm fine, sir."
Stop that.
If you say you're fine, the examiner writes "Veteran reports no issues." Boom. Denied.
You need to describe your worst day, not your best one. If you’re having a "good day" during the exam but yesterday you couldn't walk to the mailbox, tell them about yesterday. Mention the "flare-ups." The VA is legally required to consider how the condition affects you during a flare-up, not just the ten minutes you're sitting on the exam table.
Explain the functional loss. Talk about how you can't play with your kids in the yard. Talk about how you had to quit your job as a warehouse foreman because you couldn't stay on your feet. That is what "disability" actually means in the eyes of the law. It’s not just about a medical code; it’s about your inability to function in a "substantially gainful" way.
🔗 Read more: Captain Tom Bunn: Why the Most Famous Fear of Flying Author Actually Works
Evidence That Actually Moves the Needle
If you want to win, you need more than just a doctor's note. You need a "Caluza Triangle." This is the gold standard for VA claims.
- Current Diagnosis: You need a recent medical record showing you actually have plantar fasciitis. No diagnosis, no claim.
- In-Service Event: Documentation of an injury, a specific ruck march, or even just long-term "wear and tear" documented in your service treatment records.
- Medical Nexus: The link between the first two points.
I've seen veterans submit photos of their flattened arches or old physical profiles from their service records. Every bit helps. If you have prescriptions for high-dose Ibuprofen or Naproxen from ten years ago, dig them up. It proves the problem is chronic.
Podiatrists like Dr. Robert Moore have often noted that plantar fasciitis is frequently misdiagnosed or under-treated in the veteran population. Sometimes it's actually "fat pad atrophy" or "tarsal tunnel syndrome." If the VA gives you a low rating, check the diagnosis. If they diagnosed you with simple foot strain but you actually have severe plantar fasciitis with heel spurs, you’re getting shortchanged.
The Bilateral Factor
Don't forget the bilateral factor. The VA recognizes that if both your feet are messed up, the impact is more than just 10% + 10%. They add a 10% "boost" to your combined rating for bilateral conditions. It sounds like small math, but it can be the difference between a 60% and a 70% total disability rating, which is thousands of dollars over a lifetime.
What People Get Wrong About Heel Spurs
There is a huge misconception that you need heel spurs to get va disability for plantar fasciitis. You don't.
Heel spurs are just calcium deposits that sometimes show up on X-rays. Plenty of people have massive heel spurs and zero pain. Plenty of veterans have no spurs but can barely walk because the ligament is inflamed or tearing. The VA rates based on pain and function, not on what shows up on a grainy X-ray. If your examiner says, "I don't see any spurs, so you're fine," they are wrong. You can appeal that.
Navigating the Appeals Process
If you get a 0% rating (non-compensable), don't panic. A 0% rating is actually a win in a way—it means the VA acknowledges your condition is service-connected. You’ve cleared the hardest hurdle. Now, you just have to prove it's more severe than they think.
You can file a Supplemental Claim if you have new evidence, like a private medical opionion. Or, you can go for a Higher-Level Review (HLR) if you think the rater ignored evidence already in your file.
The Board of Veterans' Appeals (BVA) is the last resort. It takes forever. But sometimes, you need a judge to look at the law because the local Raters are just checking boxes.
Actionable Steps for Your Claim
If you're ready to stop hurting and start getting paid, here is the blueprint. No fluff.
First, get a formal diagnosis. Don't rely on a self-diagnosis or a "maybe" from a general practitioner. Go to a podiatrist. Get an ultrasound or an MRI if possible to show the thickness of the fascia. Anything over 4mm is usually considered pathological.
Second, track your "episodes." Keep a simple log for two weeks. When does it hurt? How long does it last? What do you have to stop doing because of the pain? This is "lay evidence" and it’s powerful.
Third, check your shoes. If you are wearing custom orthotics prescribed by a doctor, make sure that is in your record. The VA rating criteria for 20% or 30% often hinges on whether the condition is "unresponsive to treatment," and orthotics are the first line of treatment. If they don't work, you've met that criteria.
Fourth, look at your gait. If you’re limping, your knees, hips, and back are at risk. Get a doctor to document your "antalgic gait" (that’s medical speak for a limp). This sets the stage for future secondary claims.
Finally, write your Statement in Support of Claim (Form 21-4138). Don't be stoic. Be honest. Describe the "first step" pain. Describe the throbbing at night. Explain how it has limited your career or your ability to exercise.
The VA system is built on paper. If it isn't on paper, it didn't happen. Most veterans with va disability for plantar fasciitis are underrated because they didn't provide enough "functional loss" evidence. Change that. Document everything. Be persistent. The "pains of service" don't have to be suffered in silence, and they certainly shouldn't be suffered for free.