It looks like a coin. It’s shiny, small, and fits perfectly in the palm of a toddler's hand. But if that tiny silver disc—a button battery—ends up in a child’s mouth and gets swallowed, the clock starts ticking immediately. This isn't just a "wait and see if it passes" situation. It is a genuine medical emergency that can turn fatal in as little as two hours.
The terrifying reality about the symptoms of button battery ingestion is that they are incredibly easy to miss. You might think you'd see a child choking or gasping for air. Honestly? Most of the time, you won’t. The initial signs are often so subtle they mimic a common cold or a mild stomach bug. Parents frequently report that their child seemed "just a bit off" before things spiraled into a life-altering injury.
Why These Batteries Are Basically Tiny Chemical Bombs
To understand the symptoms, you have to understand the mechanism of injury. It's not usually about the battery leaking acid. That’s a common misconception. Instead, when a lithium coin battery gets stuck in the esophagus—the tube leading to the stomach—it creates an electrical circuit.
The tissue of the esophagus is moist. That moisture completes the circuit. This triggers the production of hydroxide ions, which are basically caustic soda (lye). The battery begins to literally "cook" the surrounding tissue. It creates a chemical burn that can eat through the esophagus and into the trachea or, even worse, the aorta.
Dr. Ian Jacobs, a pediatric otolaryngologist at the Children's Hospital of Philadelphia (CHOP), has highlighted that even "dead" batteries often have enough residual charge to cause these catastrophic burns. Don't assume a battery is safe just because it won't power a remote anymore.
The Stealthy Symptoms of Button Battery Ingestion
If you didn't see it happen, you're playing a guessing game.
👉 See also: Magnesio: Para qué sirve y cómo se toma sin tirar el dinero
Early on, a child might experience drooling or a sudden refusal to eat. Think about how your throat feels when you have a nasty case of strep. Now imagine that, but localized. The child might point to their chest or throat, but if they are non-verbal, they'll just be fussy.
Some kids develop a persistent cough or noisy breathing (stridor). Because the esophagus sits right next to the airway, the swelling from the chemical burn can start to compress the windpipe. If you notice your child is suddenly wheezing but has no history of asthma, that should be a massive red flag.
Vague Signs That Trick Most Parents
- Vomiting: Sometimes it’s just clear fluid; other times it might contain blood.
- Irritability: Just general grumpiness that doesn't resolve with a nap or a bottle.
- Chest pain: Older kids might describe a "tightness" or a burning sensation behind the breastplate.
- Low-grade fever: As the tissue begins to die (necrosis), the body may respond with an inflammatory fever.
The danger here is that a doctor who isn't looking for a foreign body might diagnose the child with croup or a viral infection. If you have even a 1% suspicion that a battery is missing from a toy or a key fob, you have to mention it. Be pushy.
The "Window of Opportunity" and the Honey Trick
Speed is everything. If the battery makes it all the way to the stomach, the risk of a catastrophic burn drops significantly because the stomach can handle more irritation, though it's still not "safe." But if it's stuck in the esophagus, you're in trouble.
Recent studies, including research published in The Laryngoscope, suggest that giving honey to a child (over the age of 12 months) who has just swallowed a button battery can buy you some time. Honey is a weak acid. It helps coat the battery and slow down the production of those caustic hydroxide ions.
✨ Don't miss: Why Having Sex in Bed Naked Might Be the Best Health Hack You Aren't Using
You should give 10 milliliters (about two teaspoons) of honey every 10 minutes until you get to the ER. But—and this is a big "but"—don't do this if the child is under one year old due to the risk of botulism, and don't let it delay your trip to the hospital. Get in the car. Have someone else give the honey while you drive.
What Happens at the Hospital?
When you arrive, the first thing they’ll do is an X-ray. A button battery has a very specific look on an X-ray known as the "double-halo" or "double-contour" sign. This distinguishes it from a harmless coin. If that double ring is visible, the child is rushed to surgery for an endoscopy.
The surgeon will use a flexible tube with a camera to go down and grab the battery. Even after the battery is out, the damage can continue. The caustic chemicals can stay in the tissue and keep burning for days. This is why many children remain hospitalized for observation.
Real-World Complications You Need to Know
This isn't just about a sore throat. The long-term effects of missing the symptoms of button battery ingestion can be devastating.
One of the most feared complications is an aorto-esophageal fistula. This happens when the burn goes through the esophagus and into the main artery of the body. It usually results in fatal internal bleeding. This can happen up to weeks after the battery is removed.
🔗 Read more: Why PMS Food Cravings Are So Intense and What You Can Actually Do About Them
Other kids might end up with esophageal strictures, which is basically heavy scarring that makes the throat too narrow to swallow food. These children often need repeated "dilatations," where doctors manually stretch the esophagus back open under general anesthesia. It's a long, painful road.
Common Myths About Battery Safety
A lot of people think the "bitter coating" on some batteries (like Duracell's bitterant) is a silver bullet. It's not. While it might make a child spit the battery out, it doesn't always work, and it does absolutely nothing to stop the chemical burn once the battery is swallowed.
Another myth: "My kid is five, they know better."
Statistically, toddlers are at the highest risk, but older children and even adults with cognitive impairments or those who "tackle" repairs with their teeth are also victims.
Actionable Safety Steps for Every Household
Prevention is the only 100% effective cure.
- The High-Shelf Rule: Store all spare batteries in a locked container, high up. Not just in a drawer.
- Tape the Compartments: Even if a toy has a screw-on battery cover, put a layer of heavy-duty duct tape over it. Kids are surprisingly good at finding ways to break plastic.
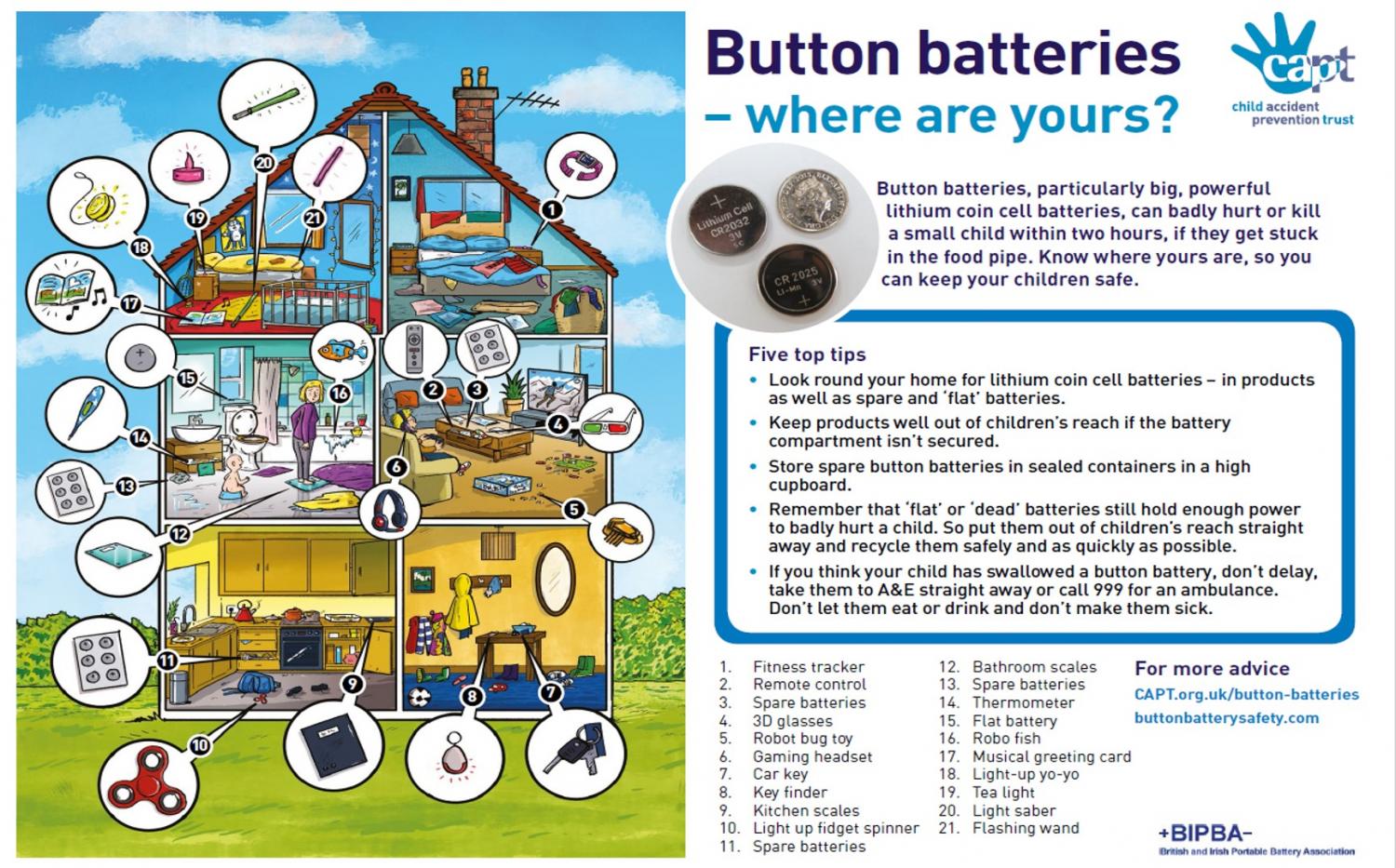
- Audit Your Devices: Walk through your house. Key fobs, flameless candles, musical greeting cards, tile trackers, and remote controls are the biggest culprits. If a device uses a button battery and doesn't have a screw-secured compartment, get rid of it or keep it entirely out of reach.
- Dispose Properly: When a battery dies, wrap it in tape immediately. This insulates the terminals and makes it less likely to cause a burn if found before it hits the recycling bin.
If you suspect an ingestion has occurred, call the National Battery Ingestion Hotline at 800-498-8666 or head straight to the nearest emergency room that has pediatric surgical capabilities. Do not induce vomiting. Do not wait for symptoms to worsen.
The silence of a button battery is its most dangerous trait. By the time the symptoms become obvious—like vomiting blood or extreme respiratory distress—the damage is often irreversible. Vigilance is the only thing that stands between a curious toddler and a life-threatening injury.
Immediate Next Steps
- Check your remotes now: Ensure all battery compartments are secured with screws or reinforced with tape.
- Locate your nearest Level 1 Pediatric Trauma Center: Not every local ER is equipped to handle pediatric endoscopic battery removal; know where you need to go before an emergency happens.
- Save the Hotline: Put the National Battery Ingestion Hotline (800-498-8666) in your phone contacts immediately.