You’re sitting on the couch, maybe scrolling through your phone, and you feel that familiar thump in your chest. Or perhaps your smartwatch just buzzed with a notification that your heart rate is "elevated" while you're just watching Netflix. It’s a weirdly personal metric, isn't it? We look at a normal resting pulse rate chart and immediately try to figure out if we’re winning at health or if something is falling apart inside. But here’s the thing: those numbers are way more flexible than most "health gurus" let on.
Most people think 72 beats per minute (bpm) is the magic number. It isn't. Not really.
✨ Don't miss: Tubby Todd Baby Acne: Does It Actually Work or Is It Just Great Marketing?
The American Heart Association (AHA) and the Mayo Clinic generally agree that a "normal" range is anywhere from 60 to 100 bpm. That’s a massive gap. It's the difference between a slow, steady drumbeat and a frantic pitter-patter. If you’re at 62, you’re fine. If you’re at 98, you’re technically "fine" too, though your doctor might want to chat about your caffeine intake or stress levels.
Decoding the normal resting pulse rate chart
When we talk about resting heart rate (RHR), we’re talking about the minimum amount of blood your heart needs to pump because you’re not doing anything. Your heart is a muscle. Like any muscle, the more efficient it is, the less work it has to do. That's why an Olympic marathoner might have a resting pulse of 38 bpm. Their heart is basically a high-performance engine that only needs to idle at a whisper.
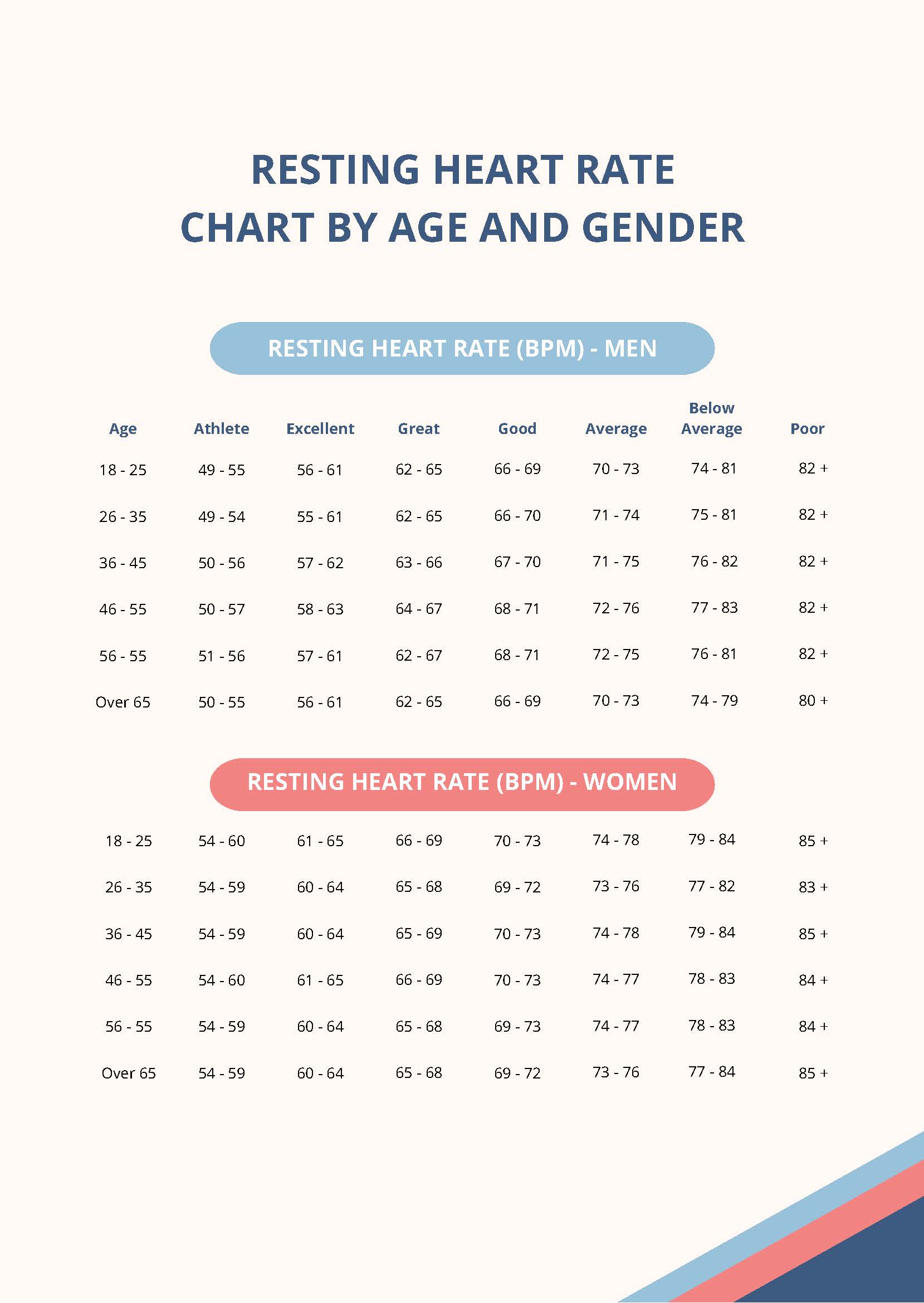
For the rest of us? The numbers shift as we age.
Newborns and Infants
Their hearts are tiny and fast. A newborn (0 to 1 month) usually sits between 70 and 190 bpm. By the time they hit their first birthday, that range narrows to about 80–130 bpm. It’s frantic. It’s supposed to be. Their metabolic demands are through the roof.
Children (Ages 1 to 10)
As kids grow, the heart matures. You’ll see a range of 70 to 110 bpm. If your ten-year-old is sitting at 95 while reading a book, don't panic. Their nervous systems are still calibrating.
Adults (18 and Over)
This is where the standard 60–100 bpm window applies. But even here, "normal" is a moving target. Research published in The Lancet has suggested that a resting heart rate on the higher end of this scale—specifically above 80 bpm—might actually correlate with higher risks of cardiovascular issues over a long period. Dr. Valentin Fuster, a renowned cardiologist at Mount Sinai, has often pointed out that while 90 bpm is "within range," it’s a very different health profile than someone sitting at 65 bpm.
Why your heart rate is a total liar sometimes
Numbers don't tell the whole story. Honestly, your pulse is a snitch. It tells on your lifestyle before you even realize what's happening.
You stayed up too late? Your pulse will show it the next morning.
Dehydrated? Your blood volume drops, making your heart work harder to move what’s left, which spikes your RHR.
Even that extra shot of espresso or a particularly stressful email from your boss can send your pulse climbing by 10 or 15 beats.
Then there’s "White Coat Hypertension." It’s a real thing. You walk into a doctor’s office, see the stethoscope, smell the antiseptic, and suddenly your heart is racing. If the nurse takes your pulse right then, the normal resting pulse rate chart they’re looking at might suggest you have tachycardia (a heart rate over 100 bpm) when, in reality, you’re just anxious about being poked with a needle.
The Fitness Factor
Athletes are the outliers. If you’re a serious cyclist or runner, your RHR might dip into the 40s or 50s. This is often called "Athletic Bradycardia." Usually, a pulse under 60 is a concern, but if you’re fit, it’s a badge of honor. Your heart is so strong that one single contraction moves a massive volume of blood.
When should you actually worry?
Consistency matters more than a single data point. If you’re usually a 65 bpm person and suddenly you’re waking up at 85 bpm every day for a week, that’s a signal. Your body might be fighting off an infection before you even feel symptoms.
Tachycardia is the term for a resting rate over 100.
Bradycardia is the term for a rate under 60 (unless you’re an athlete).
You should seek medical advice if your pulse is consistently outside the 60-100 range and you feel:
- Dizzy or lightheaded.
- Short of breath when you haven't been moving.
- Chest pain or "fluttering."
- Like you might faint.
According to the British Heart Foundation, it’s not just the speed, but the rhythm. An irregular pulse—where it skips a beat or adds an extra one—could point to Atrial Fibrillation (AFib). This is especially common as we get older.
How to get an accurate reading (The right way)
Stop checking your pulse right after you’ve walked up the stairs. That’s not "resting."
To get a true reading that actually compares to a normal resting pulse rate chart, you need to be still. Lie down or sit quietly for at least five to ten minutes. No phone. No coffee. No talking.
- Find the pulse: Use your index and middle fingers. Place them on your wrist (radial pulse) just below the thumb or on the side of your neck (carotid pulse).
- The Count: Use a watch and count the beats for 30 seconds.
- The Math: Double that number.
Do this for three mornings in a row right after you wake up, before you even get out of bed. Average those three numbers. That is your true resting heart rate. Everything else is just noise.
Factors that "fake out" the chart
Temperature plays a huge role. If it’s 95 degrees and humid, your heart has to pump more blood to the surface of your skin to help you cool down. Your pulse will go up.
Medications are another big one. Beta-blockers, often prescribed for high blood pressure, are designed specifically to slow the heart down. On the flip side, some asthma inhalers or thyroid medications can send your pulse soaring.
And let’s talk about emotions. High-intensity stress—the kind that makes your palms sweat—triggers the "fight or flight" response. Your adrenal glands dump cortisol and adrenaline into your system. Your heart rate jumps because your body thinks it needs to run away from a tiger, even if that "tiger" is just a deadline.
Moving the needle: Can you lower your resting pulse?
Yes. Absolutely. But it’s not an overnight fix.
Interval training is one of the most effective ways to strengthen the heart muscle. By pushing your heart rate high for short bursts and then letting it recover, you’re teaching your cardiovascular system to be more resilient. Over months, this typically leads to a lower RHR.
Magnesium and potassium intake also matter. These electrolytes are what allow the electrical signals in your heart to fire correctly. A deficiency can lead to palpitations or a higher-than-normal resting rate.
Actionable Next Steps:
- Establish your baseline: For the next three days, take your pulse as soon as you wake up. Write it down.
- Audit your "spikes": If you see a high number, look at your previous 24 hours. Did you drink alcohol? (Alcohol significantly raises RHR during sleep). Are you dehydrated?
- Consult the professionals: If your resting rate is consistently above 100 or below 60 (and you aren't a high-level athlete), book an appointment. Bring your three-day log with you. It’s much more helpful for a doctor than a single "high" reading in their office.
- Check your tech: If you use a wearable (Apple Watch, Garmin, Whoop), ensure the band is snug. Loose sensors give "phantom" high readings that cause unnecessary stress.
Your heart is a dynamic organ. It’s meant to change. Don’t obsess over a single beat, but pay attention to the trend. That’s where the real health story lives.