Honestly, the first few signs of ALS—or Amyotrophic Lateral Sclerosis—don’t usually feel like a "death sentence" or a medical emergency. They feel like a nuisance. You’re dropping your car keys more than usual. Or maybe you noticed your left foot "slapping" the pavement while you go for your morning walk.
It’s subtle.
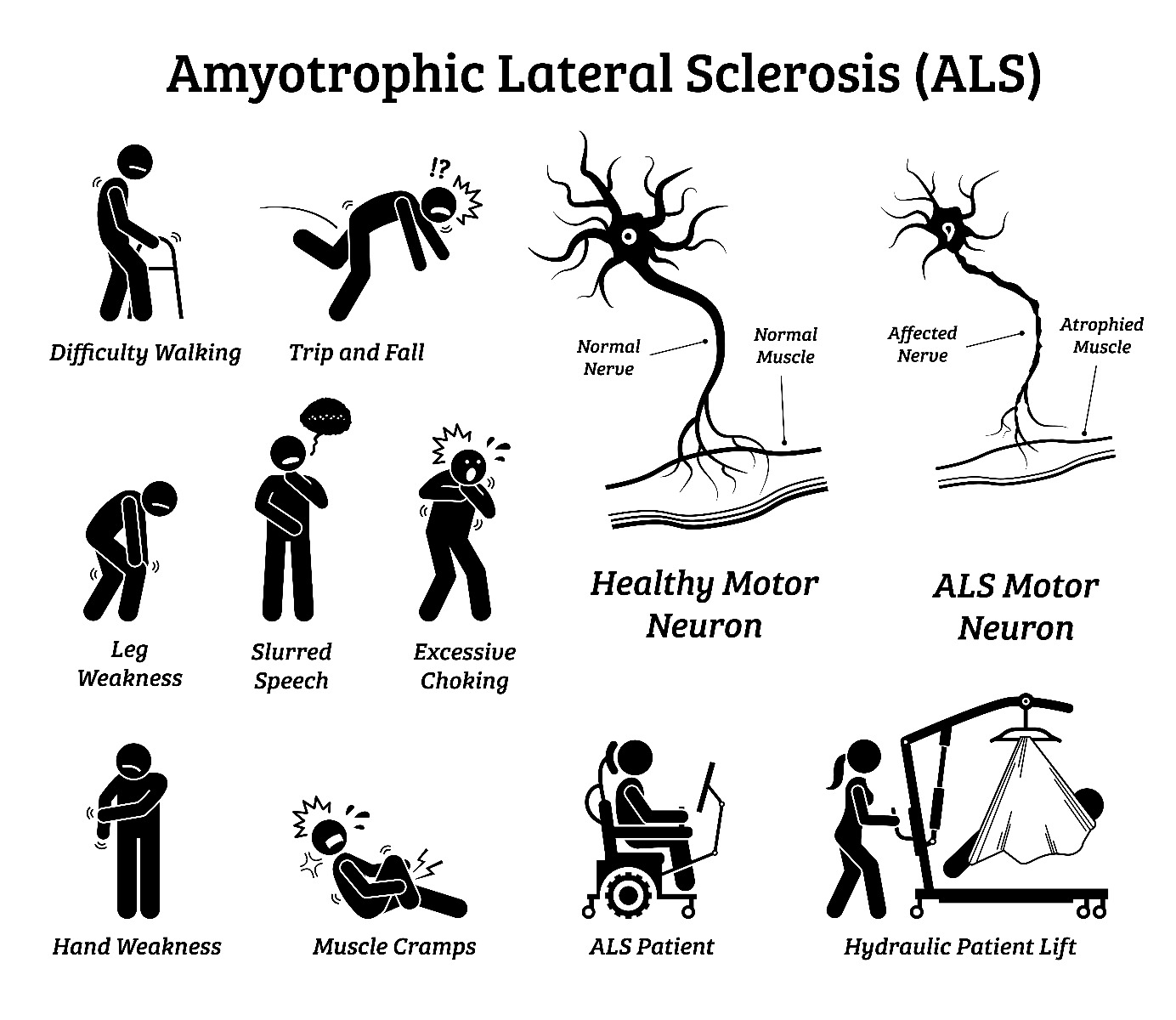
People often spend months, sometimes even a year or more, bouncing between physical therapists and orthopedists before they ever hear the name Lou Gehrig mentioned. Because lou gehrig’s disease symptoms are masters of disguise, they look like a pinched nerve, carpal tunnel, or just the "natural" process of getting older. But the reality of this motor neuron disease is that it's relentlessly progressive, and catching it early—even though there isn't a cure yet—is the only way to get ahead of the management curve.
The weird ways lou gehrig’s disease symptoms actually start
Doctors usually split the beginning of the disease into two main categories: limb onset and bulbar onset.
Limb onset is the most common path. About 70% of people start here. It’s exactly what it sounds like: it starts in the arms or legs. But it isn’t always "weakness" in the way you’d expect. Sometimes it's just a strange twitch in your calf that won't go away. These are called fasciculations. They look like little ripples under the skin, like a worm is moving around in there.
Then there’s the "clumsiness."
- The Tripping: You catch your toe on the carpet constantly. This is often "foot drop," where the muscles that lift the front of your foot start to give out.
- The Grip: Opening a jar of pickles becomes an Olympic sport. Or you find that buttoning your shirt takes five minutes because your fingers just feel... "dumb."
- The Cramping: Not just a Charlie horse after a long run, but deep, painful, involuntary muscle tightening that happens for no reason at all.
Bulbar onset is different and, quite frankly, a bit more aggressive. It starts in the muscles used for speaking and swallowing. You might notice your voice sounds a little "nasal" or like you've had a glass of wine when you're completely sober. Your tongue might feel heavy. Friends might ask if you're tired because your speech is slightly slurred.
💡 You might also like: Como tener sexo anal sin dolor: lo que tu cuerpo necesita para disfrutarlo de verdad
What most people get wrong about the "painless" disease
There’s this persistent myth that ALS doesn't cause pain.
While it's true that the disease doesn't attack the sensory nerves—meaning you can still feel heat, cold, and a light touch—the consequences of the disease are often very painful. Imagine your muscles are constantly stiff (spasticity) or cramping. Or imagine the strain on your neck because the muscles aren't strong enough to hold your head up. That hurts.
Also, it doesn’t just affect the muscles you use to move your arms. It eventually hits the ones you use to breathe.
Interestingly, your heart is usually fine. The heart is an involuntary muscle, and ALS primarily targets the voluntary ones. Your bladder and bowel control usually stay intact too, which is a small mercy in a very difficult situation.
The emotional "glitch": Pseudobulbar Affect
This is one of the most misunderstood lou gehrig’s disease symptoms. It’s called Pseudobulbar Affect (PBA). Basically, the "wiring" between the brain and the emotional response gets frayed. You might start laughing hysterically at something that isn't funny, or crying uncontrollably when you aren't even sad.
It’s not a mood disorder like depression. It’s a physical reflex.
📖 Related: Chandler Dental Excellence Chandler AZ: Why This Office Is Actually Different
It can be incredibly embarrassing for patients because it makes them feel like they’re losing their mind, even though their "thinking" brain is usually working perfectly fine. Most people with ALS remain sharp as a tack until the very end.
The 2026 diagnostic landscape: Why it takes so long
Despite all our tech, there is no single "ALS test."
Instead, it's a process of elimination. Doctors have to rule out everything else first. They’ll look for Multiple Sclerosis, Parkinson’s, Lyme disease, or even a simple Vitamin B12 deficiency. They use a tool called an Electromyography (EMG) to see if the electrical activity in your muscles is behaving the way it should.
If you’re seeing a general neurologist, the average time to get a diagnosis is about 16 months. At a specialized ALS clinic? That drops to about 9 months.
That time gap matters.
Dr. Jaimin Shah and other experts have noted that the sooner you start disease-modifying therapies like Riluzole or the newer Tofersen (if you have the specific genetic mutation), the better the outcome. We’re even seeing Phase 3 trials in 2026 for drugs like PrimeC, which showed a 33% slower progression in earlier studies.
👉 See also: Can You Take Xanax With Alcohol? Why This Mix Is More Dangerous Than You Think
Real talk on what to look for right now
If you’re worried, don’t spiral into a WebMD hole just yet. Fasciculations (twitches) on their own are usually benign—literally everyone gets them from stress or too much caffeine.
But if you have twitches plus a noticeable loss of strength in one specific area, that's when you need a neurologist.
- Check for "focal" weakness. Is it just your right hand? Just your left ankle? ALS usually starts in one spot and then spreads.
- Watch your speech. Record yourself reading a paragraph. Does it sound "slushy"?
- Monitor "micro-tasks." Are you suddenly struggling with things you've done for 20 years, like using a key or tying shoes?
Actionable steps for the path forward
If the symptoms seem to match up, don't wait for it to "clear up." It won't.
First, get a referral to a multidisciplinary ALS clinic. These clinics are game-changers. Instead of just seeing one doctor, you see a whole team: a neurologist, a physical therapist, a speech pathologist, and a nutritionist. Studies consistently show that patients who use these clinics live longer and have a much better quality of life than those who go it alone.
Second, look into genetic testing. We used to think only 10% of cases were "familial" (inherited). We’re learning that "sporadic" cases can have genetic links too. Knowing your status might open doors to clinical trials that are specific to your DNA.
Lastly, start the "hard" conversations early. ALS is a thief of time and voice. Look into "voice banking" while your speech is still clear. This allows a computer to recreate your actual voice later on if you need a communication device. It’s a small way to keep your identity intact as things change.
The road is undeniably tough. But with the current pace of research and the new therapies hitting the market in 2025 and 2026, the goal has shifted from just "surviving" to making the disease livable.
Stay proactive. Document the changes. And get to a specialist who knows exactly what they're looking at.