You’re sitting at the kitchen table, enjoying a crisp Granny Smith apple. Suddenly, your lips start tingling. Within seconds, your throat feels scratchy and your gums itch like crazy. You aren't "allergic" to apples in the way people are allergic to peanuts—you don't need an EpiPen, and you've eaten apples a thousand times before. What's happening is your immune system is being tricked. It’s a glitch in the body's matrix called Pollen Food Allergy Syndrome (PFAS), and if you're looking for an oral allergy syndrome list of foods, you’re likely trying to figure out why your favorite snacks are betraying you.
It's weird. Truly.
Most people think allergies are binary—you either have them or you don't. But Oral Allergy Syndrome (OAS) is a cross-reaction. Your body sees the proteins in certain raw fruits, vegetables, or nuts and mistakes them for the pollen you sneeze at every spring or fall. If you're allergic to birch trees, an apple looks exactly like birch pollen to your immune system. It’s a case of mistaken identity at the molecular level.
The Big Culprits: An Oral Allergy Syndrome List of Foods by Pollen Type
Honestly, the "trigger" isn't the food itself. It’s the pollen you’re already sensitized to. When you look at an oral allergy syndrome list of foods, you have to categorize them by their "parent" pollen. If you don't know what you're allergic to in the environment, this list might actually help you reverse-engineer your seasonal allergies.
If Birch Pollen is Your Enemy
This is the most common trigger for OAS in the Northern Hemisphere. Birch trees release fine, powdery pollen in the spring, and the proteins in that pollen are remarkably similar to those found in the rose family (Rosaceae). If you find yourself reaching for Benadryl after eating a peach, birch is likely the culprit.
The list for birch-sensitive individuals is long and, frankly, annoying because it covers so many staples. You've got apples, pears, peaches, plums, nectarines, and cherries. It also extends to pitted fruits like apricots. On the vegetable side, keep an eye on carrots, celery, and parsley. Even certain legumes and nuts like peanuts, hazelnuts, and soybeans (including soy milk) can trigger that characteristic mouth itch.
The Ragweed Connection
Ragweed is the bane of existence for millions in late summer and autumn. If you spend August sneezing, you might notice that certain late-summer produce makes your mouth feel "fuzzy." The primary offenders here are bananas, melons (cantaloupe, honeydew, watermelon), and tomatoes. Interestingly, zucchini and cucumbers are also on this list. Have you ever noticed a slight tingle after eating a sunflower seed or sipping chamomile tea? Those are ragweed cousins. Even echinacea, often taken for "immune support," can trigger a reaction in ragweed-allergic people.
📖 Related: Does Ginger Ale Help With Upset Stomach? Why Your Soda Habit Might Be Making Things Worse
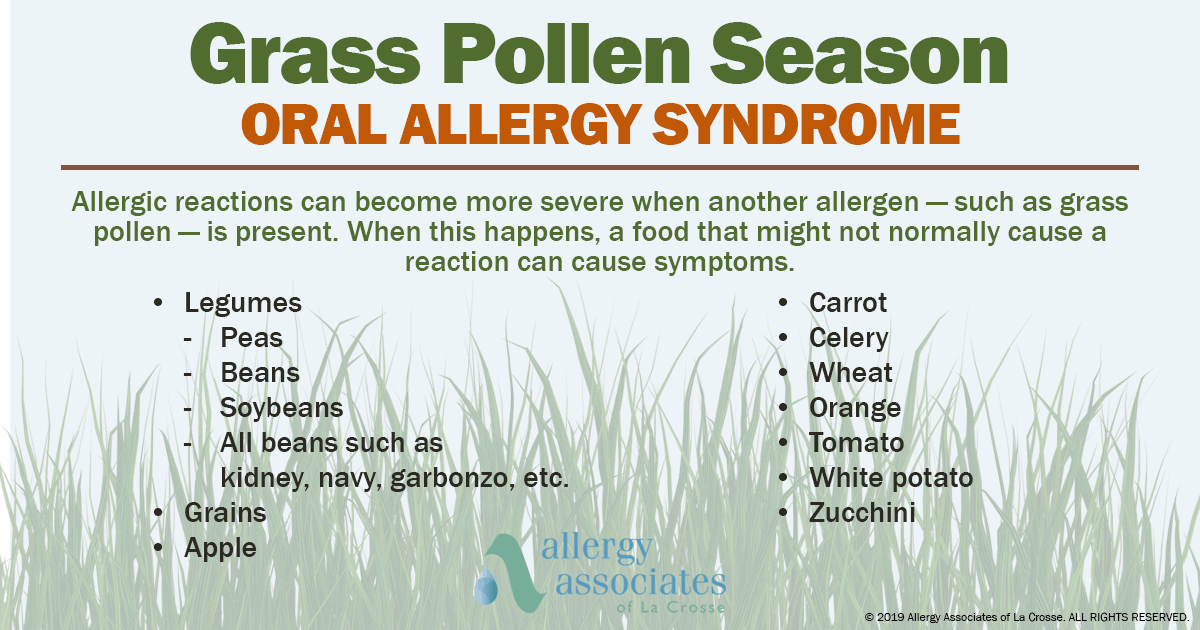
Grass Pollen and Your Salad
Grass allergies are incredibly common, but the food cross-reactivity is slightly less frequent than birch. Still, it happens. The main items on the oral allergy syndrome list of foods for grass-allergic folks include tomatoes, oranges, peanuts, and Swiss chard. Sometimes potatoes or melons show up here too. It’s less about a "scratchy throat" and often more of a localized lip swelling.
Mugwort: The Hidden Trigger
Mugwort is a weed that many people don't even realize they're allergic to until they eat a salad. The "Celery-Mugwort-Spice" syndrome is a real medical observation. If mugwort is your trigger, you might react to celery, carrots, and peppers. But the real kicker is spices. Coriander, fennel, garlic, parsley, and onion can all cause reactions. This makes dining out particularly tricky because these ingredients are the foundation of almost everything savory.
Why Does This Happen? (The Science Part)
Let’s get technical for a second. The proteins involved are called Pathogenesis-Related (PR) proteins, specifically the PR-10 family. These proteins are defense mechanisms for plants. They are "heat-labile," which is a fancy way of saying they are fragile. They break down almost immediately when exposed to heat or stomach acid.
This is why you can eat a McDonald’s apple pie or a jar of applesauce without any issues, but a raw Gala apple makes your mouth feel like it’s on fire. The cooking process denatures the protein. Your immune system no longer recognizes the "enemy" because the "uniform" has been melted away.
It’s also why you don't usually see systemic reactions like hives or anaphylaxis with OAS. By the time the food hits your stomach, your gastric acid has basically dismantled the allergens. The reaction is strictly local—lips, tongue, throat.
The "Latex-Fruit" Mystery
There is another version of this that isn't related to pollen at all. It’s called Latex-Fruit Syndrome. If you are sensitive to natural rubber latex (the kind found in medical gloves or some balloons), your body might freak out when you eat avocados, kiwis, chestnuts, or papayas.
👉 See also: Horizon Treadmill 7.0 AT: What Most People Get Wrong
Unlike pollen-related OAS, this one can occasionally be more serious. The proteins in these fruits are more stable than the birch-pollen lookalikes. If you notice your mouth itching after avocado toast and you also get a rash from rubber bands, you need to talk to an allergist immediately. This isn't just a "minor annoyance" situation.
How to Manage Your Diet Without Losing Your Mind
Living with an oral allergy syndrome list of foods doesn't mean you have to stop eating healthy. It just means you have to be strategic. You aren't actually allergic to the fruit; you're allergic to a protein in the fruit.
Microwave it. Seriously. If you're craving a peach, popping it in the microwave for 10 to 30 seconds can sometimes denature the proteins enough to stop the reaction without completely ruining the texture. It won't be a "fresh" peach anymore, but it won't itch.
Peel it. In many fruits, like apples and pears, the offending proteins are concentrated in the skin. If you peel the fruit, you might find you can tolerate the flesh just fine. This isn't a 100% guarantee, but for many, the skin is where the trouble lies.
Buy canned. Canned fruits and vegetables are processed with high heat. This effectively "kills" the allergen. If you miss pears, canned pears are a perfectly safe alternative.
Know the "High Season." Your OAS will almost always be worse during the peak of the corresponding pollen season. If it's April and the birch trees are dumping yellow dust everywhere, your body is already on high alert. That apple is the "last straw" for your immune system. You might find you can eat apples just fine in December but have to avoid them in the spring.
✨ Don't miss: How to Treat Uneven Skin Tone Without Wasting a Fortune on TikTok Trends
When to See a Doctor
Most cases of OAS are mild. You itch, you drink some water, it goes away in ten minutes. But "most" isn't "all." According to the American Academy of Allergy, Asthma & Immunology (AAAAI), about 1% to 2% of people with OAS may experience a more severe reaction, including throat swelling or systemic symptoms.
If your symptoms go beyond the mouth—if you get hives, if you feel dizzy, or if you have trouble swallowing—that isn't simple OAS. That’s a primary food allergy. You need a skin prick test or a blood test (IgE) to confirm what’s actually going on.
Dr. Scott Sicherer, a leading expert at Mount Sinai, often points out that the history of the reaction is more important than the test itself. If you tell an allergist that you only itch with raw apples but eat apple pie fine, they can almost diagnose you on the spot without even poking you.
Nuance: It’s Not Just "Fruits and Veggies"
We often forget about nuts. Hazelnuts and almonds are frequently on the oral allergy syndrome list of foods. This is a terrifying cross-section because nut allergies can be fatal. If you have a birch allergy and your mouth itches when you eat an almond, it might just be OAS. However, you cannot assume that.
The danger is "masking." You might think your almond itch is just OAS, but it could be the start of a true, systemic nut allergy. Never self-diagnose when it comes to nuts. The stakes are too high. Get the testing done to ensure you aren't carrying a ticking time bomb in your snack bag.
Actionable Steps for Relief
If you’ve just looked at an oral allergy syndrome list of foods and realized your diet is a minefield, don't panic. Here is exactly what you should do next to manage the discomfort:
- Keep a "Symptom Diary." Don't just write down what you ate. Write down the time of year and whether the food was raw, cooked, or peeled. You’ll start to see patterns. Maybe you only react to Red Delicious apples but not Galas. (Yes, the protein levels vary by cultivar!)
- The "Heat Treatment" Test. Next time you want a "forbidden" fruit, try a small piece of it cooked. If you can eat a roasted carrot but not a raw one, you’ve confirmed it’s likely OAS and not a permanent, dangerous food allergy.
- Rinse Your Mouth. If a reaction starts, immediately rinse your mouth with cool water. Sometimes simply washing away the surface proteins can shorten the duration of the itch.
- Check Your Spices. If you have unexplained mouth irritation after eating out, look at the "hidden" ingredients. Cumin, coriander, and fennel are huge triggers for those with weed allergies.
- Talk to an Allergist About Immunotherapy. Sometimes, treating the underlying pollen allergy with allergy shots or sublingual drops can actually reduce or eliminate the food cross-reactivity. If you fix the "root" (the pollen), the "branches" (the food) often follow suit.
Oral Allergy Syndrome is a nuisance, but it’s a manageable one. It’s your body being a bit too overprotective. By understanding which pollens correlate to which foods, you can stop guessing and start eating with a lot less anxiety. Just remember: if it's raw and it itches, it’s probably the protein, not the produce. Keep your fruits peeled, your veggies steamed, and your antihistamines handy during peak season.