You’re sitting in that crinkly paper-covered chair at the doctor's office. The cuff squeezes your arm until it pulses. The nurse mutters "125 over 72" and moves on to the next thing.
Wait. Is that good?
Most of us grew up thinking 120/80 was the gold standard, the "perfect" score. So, seeing 125 over 72 can feel like you’ve slightly failed a test you didn't study for. It’s a weird middle ground. You aren't "hypertensive" in the way your grandfather was, but you aren't exactly in the green zone either. It’s basically the yellow light of cardiovascular health.
The truth is, blood pressure 125 over 72 is technically classified as elevated blood pressure.
The American Heart Association (AHA) and the American College of Cardiology changed the rules back in 2017. They lowered the bar. Suddenly, millions of people who thought they were "fine" were told they were "elevated." It caused a bit of a stir in the medical community. Some doctors thought it was over-medicalizing normal aging. Others argued that catching these numbers early saves lives. Honestly, both sides have a point, but the data leans toward being proactive.
Breaking down the numbers
Let's talk about what these two numbers actually represent. The top number, 125, is your systolic pressure. It measures the force your heart exerts on the walls of your arteries each time it beats. The bottom number, 72, is the diastolic pressure. That’s the pressure in your arteries when your heart rests between beats.
In a 125 over 72 reading, your diastolic (72) is actually fantastic. It’s well within the "normal" range, which is anything under 80. The "issue"—if we even want to call it that—is the 125.
Anything between 120 and 129 for that top number is now considered elevated.
Why does five points matter? It’s about the long game. Think of your arteries like a garden hose. If you turn the pressure up just a tiny bit too high for twenty years, the hose starts to wear out faster. It gets stiff. It might develop little cracks. In your body, those "cracks" are where plaque builds up, leading to the scary stuff like strokes or heart attacks.
💡 You might also like: Foods to Eat to Prevent Gas: What Actually Works and Why You’re Doing It Wrong
Dr. Paul Whelton, who chaired the committee that wrote the 2017 guidelines, has been very vocal about this. He points out that the risk of cardiovascular disease doesn't magically start at 140/90. It’s a sliding scale. The risk starts climbing much earlier than we used to think.
The "White Coat" factor and why one reading is meaningless
Don't panic over one 125 over 72 reading. Seriously.
Blood pressure is incredibly fickle. It’s more like a movie than a still photograph. If you rushed into the clinic because you were late for your appointment, your 125 is probably a lie. If you had a double espresso twenty minutes before the nurse wrapped the cuff around your arm, that 125 is definitely a lie.
There is a real phenomenon called White Coat Hypertension. Some people’s blood pressure spikes just because they are in a medical setting. Their brain perceives the doctor as a "threat" and kicks off a mild fight-or-flight response.
Then there’s the opposite: Masked Hypertension. This is when your pressure looks great at the doctor but spikes when you’re dealing with a stressful deadline at work or an argument at home.
To really know if 125 over 72 is your "real" number, you need a trend. Doctors usually want to see a week’s worth of readings taken at home, under calm conditions, before they make any declarations.
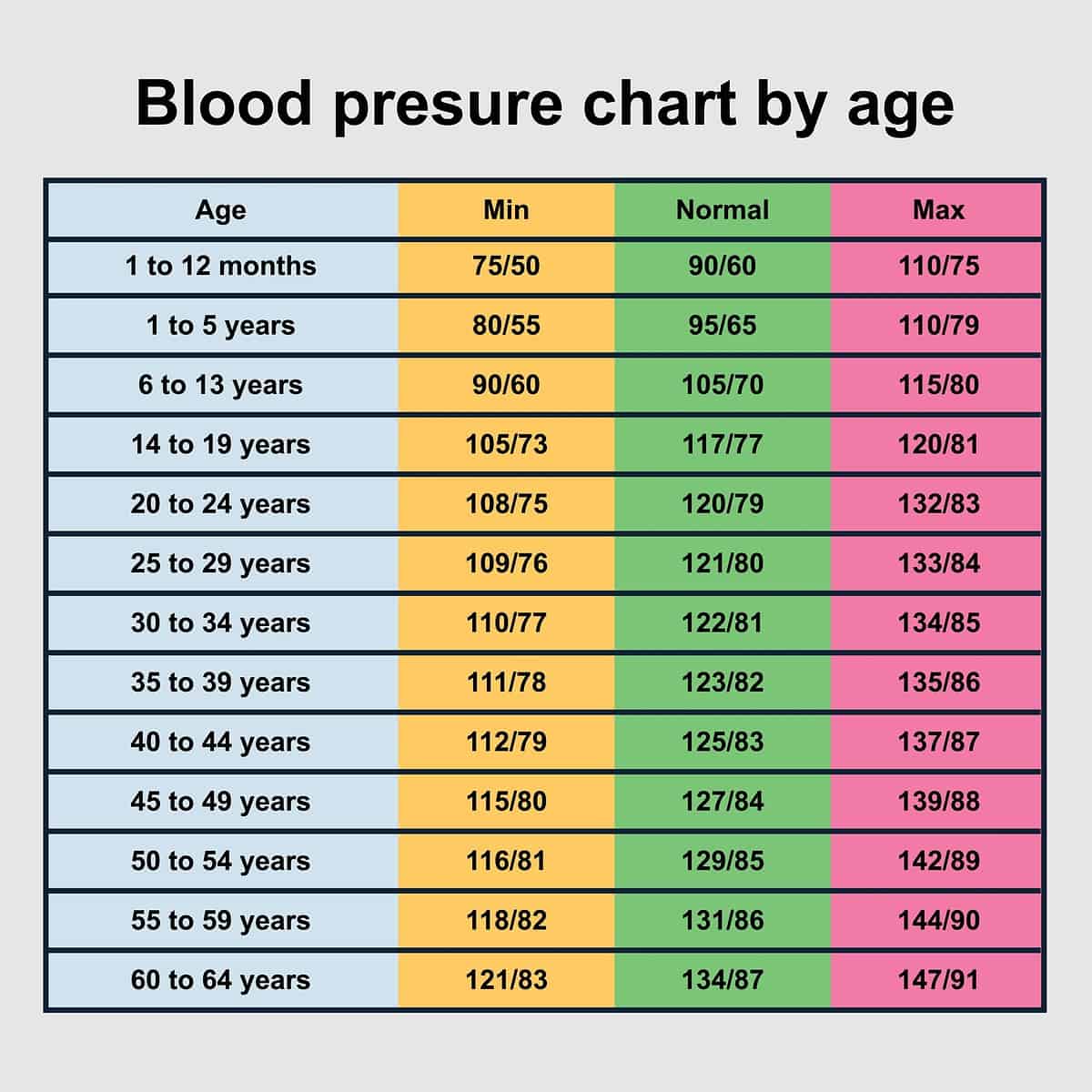
Does age change the math?
This is where things get nuanced. If you are 22 years old and sitting at 125 over 72, your doctor might give you a bit of a "look." At that age, your arteries should be very elastic. A 125 could suggest that your lifestyle—maybe too much salt, not enough sleep, or high stress—is starting to take a toll.
However, if you are 75? A systolic of 125 is often celebrated.
📖 Related: Magnesio: Para qué sirve y cómo se toma sin tirar el dinero
As we age, our arteries naturally stiffen. It’s called arteriosclerosis. Because the pipes are stiffer, the pressure naturally goes up. For older adults, trying to force the blood pressure down to 110/70 can sometimes do more harm than good. It can cause dizziness, which leads to falls.
The SPRINT trial (Systolic Blood Pressure Intervention Trial) was a massive study that looked into this. It showed that for many people, getting that top number below 120 significantly reduced heart problems. But, and this is a big "but," it also increased the risk of kidney issues and fainting. Medicine is always a trade-off.
Salt, Stress, and the 125 over 72 lifestyle
If you're consistently hitting 125 over 72, you aren't at the stage where most doctors will reach for the prescription pad. You're in the "lifestyle modification" zone.
Salt is the obvious villain here. Most of us eat way more than we realize. It’s not the salt shaker on the table; it’s the sodium hidden in bread, pasta sauces, and deli meats. Sodium makes your body hold onto water. More water in your blood means more volume. More volume means higher pressure. It’s basic physics.
Potassium is the unsung hero. It helps your body flush out sodium and eases the tension in your blood vessel walls. If you aren't eating bananas, spinach, or sweet potatoes, you're missing out on a natural "chilling" effect for your arteries.
Then there’s alcohol. This one hurts to hear, but even "moderate" drinking can nudge that 125 closer to a 130. Alcohol constricts blood vessels and can mess with the nervous system's control of blood pressure.
Why the 72 is your best friend
We spend a lot of time obsessing over the top number, but that 72 is doing some heavy lifting.
A diastolic pressure of 72 means that when your heart is relaxing, your system is under very little stress. It suggests your heart is able to fill with blood efficiently. When the diastolic number starts creeping up toward 80 or 90, it means the "baseline" pressure is too high. That's a different kind of problem.
👉 See also: Why Having Sex in Bed Naked Might Be the Best Health Hack You Aren't Using
Having a 125 over 72 is often what we call Isolated Systolic Hypertension (though 125 is a very mild version of it). It basically means your heart is pumping a bit hard, but your resting state is totally fine.
Practical steps to move from "Elevated" to "Normal"
You don't need a radical overhaul to shave five points off that top number. Small, annoying consistency usually wins here.
Watch the "hidden" sodium. Check the labels on things you wouldn't suspect. Salad dressings and "healthy" frozen meals are notorious for having 800mg of sodium per serving. The goal for most people with elevated pressure is to stay under 1,500mg a day.
The 150-minute rule. You don't have to run marathons. Brisk walking for 30 minutes, five days a week, is the sweet spot. Exercise makes your heart stronger. A stronger heart can pump more blood with less effort, which lowers the force on your arteries.
Breathing, seriously. If your 125 over 72 is driven by a high-stress job, look into "slow breathing." Taking six deep breaths over a minute has been shown in small studies to acutely lower systolic pressure. It’s not a permanent fix, but it trains your nervous system to stay out of that "high-alert" mode.
The DASH diet. Dietary Approaches to Stop Hypertension. It’s not a fad; it’s one of the most clinically proven ways to lower blood pressure. It’s heavy on fruits, veggies, and low-fat dairy. It’s basically the Mediterranean diet’s slightly more focused cousin.
Monitor at home. Get a validated arm cuff (not a wrist one—those are notoriously flaky). Take your pressure at the same time every morning before you eat or have caffeine. Do this for two weeks and show the log to your doctor.
A single reading of 125 over 72 is a snapshot, not a destiny. It’s a gentle nudge from your body saying, "Hey, let's keep an eye on things." It’s an opportunity to make tiny shifts now so you don't have to make massive, forced changes ten years down the road. Focus on the trend, not the moment. Adjust the salt, keep moving, and check back in a month. Your heart will thank you for the lower workload.