Honestly, most people approach flu season like they’re preparing for a light rain shower when a hurricane is actually on the horizon. We buy a bottle of hand sanitizer, maybe eat an extra orange, and hope for the best. But if you’ve ever spent four days staring at the ceiling because your joints ache so bad you can’t even reach for the TV remote, you know that "hoping" isn't exactly a clinical strategy. Learning how to prevent flu requires a bit more than just washing your hands after you touch a grocery cart. It's about biology, timing, and understanding that the Influenza virus is a shapeshifter.
It's a nasty little bugger.
The CDC estimates that since 2010, the flu has resulted in between 9 million and 41 million illnesses annually in the United States alone. Those aren't just numbers; those are missed shifts, cancelled vacations, and, for many, hospital stays. The problem is that we treat flu prevention as a one-time checklist item rather than a multi-layered defense system.
✨ Don't miss: Juices to Make in a Juicer: Why Your Recipes Probably Taste Like Grass
The Science of Not Getting Sick
If you want to know how to prevent flu, you have to understand the "Swiss Cheese Model." Imagine several slices of Swiss cheese lined up. Each slice has holes—these are the weaknesses in your individual defenses (like forgetting to wash your hands or being sleep-deprived). If the holes align, the virus gets through. But if you stack enough slices—vaccination, hygiene, air quality, and immune support—the chances of a "hole" going all the way through the stack become remarkably slim.
Let's talk about the big one: the shot.
The annual flu vaccine is the most controversial yet effective tool we have. Every year, the World Health Organization (WHO) monitors "sentinel" sites globally to predict which strains will circulate. Usually, it's a mix of Influenza A (H1N1 and H3N2) and Influenza B lineages. Is it 100% effective? No. Not even close. Depending on the "match" between the vaccine and the circulating virus, effectiveness usually hovers between 40% and 60%.
That sounds low, right? But here is the nuance most people miss: even if you get sick after being vaccinated, the shot acts like a "training manual" for your immune system. You might feel crummy for two days instead of being bedridden for ten. It drastically reduces the risk of cytokine storms—where your immune system overreacts and starts damaging your own lungs. Dr. Helen Chu, an infectious disease expert at the University of Washington, has frequently noted that the goal of the vaccine isn't just "zero infection," but "zero hospitalization."
Timing is everything
You can't just get the shot in August and expect it to hold up through April. Immunity wanes. For most people, late October is the "Goldilocks" zone. Get it too early, and your antibodies might dip just as the February peak hits. Get it too late, and you’re vulnerable during the initial holiday surge.
Why Hand Sanitizer Isn't a Magic Wand
We've become obsessed with gels. But here’s the reality: hand sanitizer is a backup, not the main event. The flu virus is an enveloped virus, meaning it has a fatty outer layer. Alcohol breaks that layer down, which is great. However, if your hands are physically dirty or greasy, the alcohol can't reach the virus.
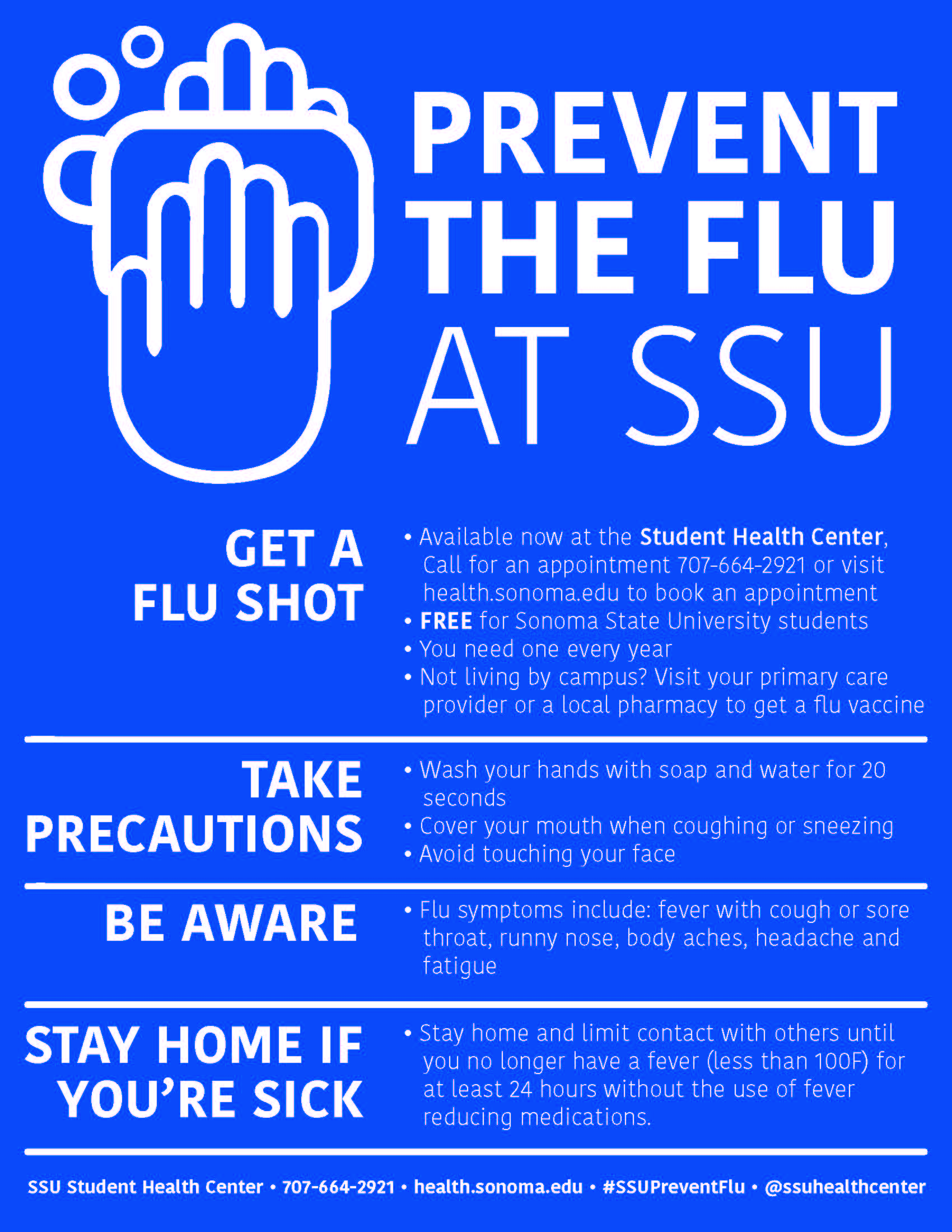
Good old-fashioned soap and water for 20 seconds is still the gold standard.
Why? Because soap is a surfactant. It literally lifts the virus off your skin so it can be rinsed down the drain. Plus, the mechanical action of rubbing your hands together breaks the viral bonds.
🔗 Read more: The Peculiar Science of the Human Shoulder: Why It Breaks So Easily
And stop touching your face. Seriously. The average person touches their face about 23 times per hour. Your eyes, nose, and mouth are the highways to your respiratory system. You could have the virus on your thumb for an hour and be fine, but the second you rub your eye, it's game over.
The Air You Breathe Matters More Than You Think
Recent studies, particularly those spurred by the COVID-19 pandemic, have shifted our understanding of how respiratory viruses move. We used to think it was all about "large droplets"—the wet stuff that flies out when someone sneezes. Now we know aerosols (tiny particles that linger in the air) play a huge role.
If you're in a stuffy, poorly ventilated office with someone who has the flu, you’re breathing in their viral load.
- Humidity is your friend. In winter, indoor air becomes incredibly dry. This dries out your mucous membranes—the sticky lining in your nose that’s supposed to trap viruses. When that lining cracks, the virus has an open door.
- Open a window. Even five minutes of fresh air can significantly lower the viral concentration in a room.
- HEPA filters. If you can't control the windows, a high-quality air purifier can capture those tiny viral particles before you inhale them.
The "Lifestyle" Defense: It's Not Just Vitamin C
Everyone reaches for the Emergen-C the moment they hear a coworker cough. But the truth about Vitamin C is a bit disappointing. Meta-analyses of dozens of studies show that starting Vitamin C after symptoms appear does almost nothing to shorten the flu.
If you want to use nutrition to figure out how to prevent flu, you have to look at Vitamin D and sleep.
Vitamin D deficiency is rampant in northern latitudes during winter. A study published in the British Medical Journal found that Vitamin D supplementation can help prevent respiratory infections, especially in people who are deficient. It helps the body produce cathelicidins and defensins, which are essentially natural antibiotics and antivirals.
Then there’s sleep. This isn't just about feeling rested. When you sleep, your body produces cytokines, proteins that help the immune system communicate. A famous study in the journal Sleep showed that people who slept less than six hours a night were four times more likely to catch a cold or flu than those who got seven hours or more. If you're "grinding" on four hours of sleep, you're basically leaving your front door unlocked and inviting the virus in for coffee.
Common Misconceptions That Get People Sick
"I got the flu from the flu shot."
No, you didn't. It is biologically impossible. The injectable flu vaccine contains "killed" (inactivated) virus or just a single protein from the virus. It cannot replicate. What you likely felt was your immune system's "fire drill"—aches and a low-grade fever mean the vaccine is working. Or, you were already incubating a different virus when you got the shot.
"I have a 'strong' immune system so I don't need the vaccine."
The irony is that many of the worst flu symptoms are caused by a strong immune system. The high fever and lung inflammation are your body’s scorched-earth policy to kill the virus. Sometimes, a "strong" immune system overreacts so violently it causes more harm than the virus itself. The vaccine teaches your body to respond precisely rather than blowing everything up.
What to Do if You Feel "The Tingle"
We all know the feeling. That slight scratch in the throat. The sudden, inexplicable chill.
- Test, don't guess. In 2026, home molecular tests (like Lucira or Cue) are much more accessible. Knowing if it's Flu A, Flu B, or COVID-19 changes your treatment plan.
- The 48-Hour Window. Antivirals like Oseltamivir (Tamiflu) or the newer Baloxavir marboxil (Xofluza) are highly effective, but they are time-sensitive. If you don't take them within the first 48 hours of symptom onset, they barely do anything. They work by stopping the virus from replicating or exiting your cells. Once the virus has already spread through your system, the horse has left the barn.
- Hydration or Bust. Flu causes high fevers, which lead to dehydration. Dehydration thickens mucus, making it harder for your lungs to clear out the junk. Drink more water than you think you need.
Practical Steps for High-Risk Environments
If you work in a school, a hospital, or an open-plan office, your risk profile is different. You can't just "avoid people."
Wear a mask in high-density areas during peak weeks (usually January and February). An N95 or KF94 doesn't just protect others; it protects you from inhaling those lingering aerosols we talked about. It’s not about being fearful; it’s about being pragmatic.
Also, consider the "fomite" factor in shared spaces. The office coffee pot handle? The elevator button? These are high-traffic viral landing pads. Use your knuckle instead of your fingertip. It sounds paranoid until you realize that the flu virus can live on hard surfaces for up to 24 hours.
Actionable Strategy Checklist
To truly master how to prevent flu, move away from reactive habits and toward a proactive system.
🔗 Read more: Average calories consumed on Thanksgiving: What the numbers actually say about that one big meal
- Audit your Vitamin D levels via a blood test and supplement if necessary under medical supervision.
- Book your vaccine for late October to ensure coverage lasts through the spring "second wave."
- Invest in a cool-mist humidifier for your bedroom to keep respiratory barriers intact.
- Create a "Sanitizing Station" by your front door. Sanitize your hands and phone the second you walk in from public spaces. Your phone is basically a Petri dish you carry against your face.
- Prioritize 7-9 hours of sleep during peak transmission months. Think of it as a free medicine.
- Keep a supply of high-quality masks and a thermometer ready so you aren't scrambling to the pharmacy when you already feel weak.
- Consult your doctor early about a prescription for antivirals if you are in a high-risk group (over 65, asthmatic, or immunocompromised), so you know the plan before you get sick.
The flu isn't an inevitability. It's a calculated risk. By layering these defenses—vaccination, air quality, sleep, and hygiene—you shift the odds significantly in your favor. Stay vigilant, keep your humidity up, and treat your sleep like your life depends on it, because during a bad flu year, it just might.