It’s not always the dramatic, clutch-your-chest-and-fall-over moment Hollywood loves. Honestly, the way a heart attack starts is usually much stealthier, and frankly, more terrifying because of how mundane it can feel at first. You might just think it’s bad carnitas or a pulled muscle from the gym.
But beneath the surface, your biology is hitting a breaking point.
When people ask how does a heart attack start, they’re usually looking for a timeline. They want to know the "when" and the "why" of that first spark of pain. To understand it, you have to look at your coronary arteries not just as pipes, but as living, reacting tunnels that have been under siege for decades. It starts with a microscopic tear, a bit of cholesterol, and a sudden, violent chemical reaction that shuts everything down.
👉 See also: St. Elizabeth in Edgewood: What You Actually Need to Know Before You Go
The Slow Burn: It Starts Decades Before the Pain
A heart attack doesn't technically start the moment you feel pain. It starts when you're a teenager. That sounds extreme, but the American Heart Association has shown that fatty streaks begin appearing in our arteries very early in life. This is the "pre-game" for a myocardial infarction.
Think of your arteries like a busy highway. Over time, LDL cholesterol (the "bad" kind) starts seeping into the inner lining of the artery wall. Your body sees this as an injury. It sends white blood cells called macrophages to clean up the mess. But these cells eat too much cholesterol, get bloated, and turn into "foam cells." These cells eventually die and sit there, rotting into a waxy, yellow gunk we call plaque.
This process, atherosclerosis, is silent. You can’t feel it. You could have a 70% blockage and feel totally fine while jogging. The danger isn't necessarily the size of the blockage; it’s the stability of the plaque.
The Moment of Impact: Plaque Rupture
This is the "Big Bang" of the cardiac event. Most heart attacks aren't caused by a pipe getting slowly narrowed until it closes. Instead, a relatively small, "vulnerable" plaque—one that’s soft and fatty—suddenly ruptures.
Imagine a blister. When that thin cap over the plaque tears, the "lava" inside—a mix of fats, proteins, and inflammatory gunk—is exposed to your blood. Your blood reacts instantly. It thinks there’s a massive internal leak that needs to be plugged. Platelets rush to the scene. Within seconds, a blood clot forms.
This is exactly how does a heart attack start in the clinical sense. The clot grows so fast that it completely chokes off the blood flow to a section of the heart muscle. The clock is now officially ticking.
The Starvation Phase: Myocardial Ischemia
Once that clot is in place, the heart muscle downstream is suddenly starving. It’s screaming for oxygen. In medical terms, this is ischemia.
✨ Don't miss: Eyes Yellow in the Corners: Why it Happens and When to Worry
The heart is a greedy muscle. It never rests, so it needs a constant, high-pressure stream of oxygenated blood. When that stops, the cells start to malfunction. They can't pump right. They start leaking potassium and taking in too much calcium.
Why the Pain Travels
Ever wonder why your jaw hurts when your heart is the problem? It’s basically a wiring issue in your nervous system. The nerves that carry pain signals from the heart enter the spinal cord at the same levels as the nerves from the jaw, neck, and left arm. Your brain gets "confused" and attributes the heart’s distress to your arm or throat. This is called referred pain.
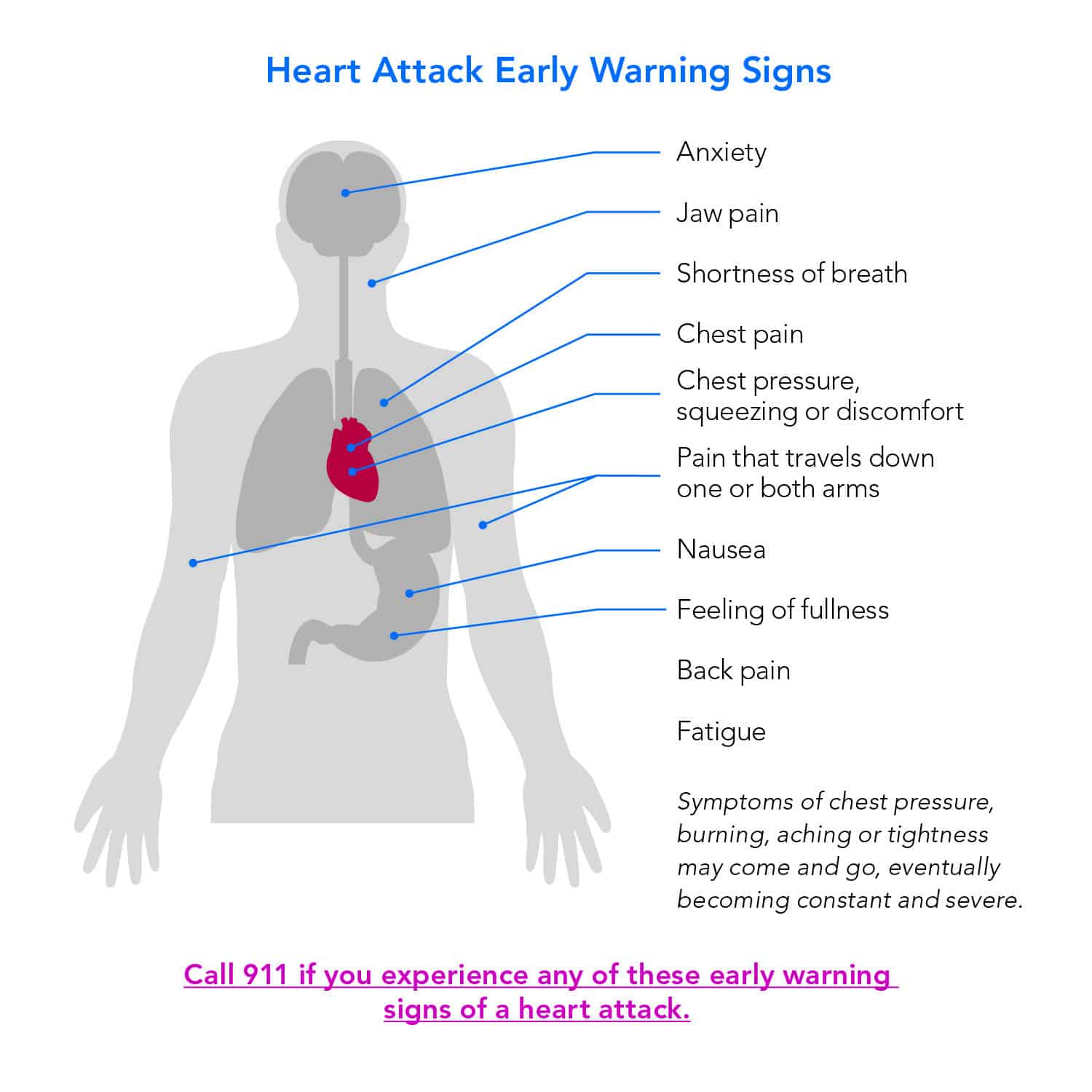
For some people—especially women and those with diabetes—the nervous system response is even weirder. You might not feel pain at all. Instead, you get "silent" symptoms:
- Extreme, unexplained fatigue that feels like you've run a marathon while sitting still.
- Cold sweats that come out of nowhere.
- A sense of "impending doom"—this is a real clinical symptom where your sympathetic nervous system is firing off "danger" signals before your conscious mind knows why.
- Nausea that feels like a stomach flu but doesn't go away with antacids.
The Role of Inflammation and Stress
We used to think it was just about high cholesterol. We were wrong.
Dr. Paul Ridker from Brigham and Women’s Hospital has done massive amounts of research showing that inflammation is just as big a player as LDL. If your body is in a state of chronic inflammation—maybe from smoking, chronic stress, or an autoimmune condition—your plaques are much more likely to be "unstable."
Stress can be the final nudge. A massive surge of adrenaline can increase heart rate and blood pressure so sharply that it literally shears the cap off a plaque. This is why you hear about people having heart attacks during high-stress events or even intense physical exertion they aren't used to.
💡 You might also like: 24 Hour Fitness Memorial Day Hours: What to Know Before You Head Out
Biological Differences: Men vs. Women
It’s frustrating, but the medical world spent decades only studying how heart attacks start in men. In men, it’s often that classic "elephant on the chest" feeling.
In women, the start of a heart attack can look very different. Women are more likely to have "microvascular disease." Instead of one big blockage in a main artery, the tiny "tributary" vessels of the heart get constricted or damaged. This leads to symptoms like shortness of breath or pressure in the lower chest or upper abdomen.
Because these symptoms don't scream "HEART ATTACK," women often wait longer to go to the ER. That delay is deadly. If you feel like something is "off" in your chest or breathing, do not worry about being "dramatic." Go get checked.
What Happens if You Wait?
Every minute matters. "Time is muscle" is the mantra in every cardiology ward.
After about 20 to 40 minutes of zero blood flow, the heart muscle cells start to die. This is permanent. Unlike skin or bone, heart muscle doesn't really regenerate; it replaces itself with scar tissue. Scar tissue doesn't pump. If you lose too much muscle, you end up with heart failure, which is a lifelong struggle with fluid buildup and exhaustion.
If the clot is in the Left Main Coronary Artery—often called the "Widowmaker"—the damage is so widespread that the heart can stop beating entirely within minutes. This leads to sudden cardiac arrest, which is different from a heart attack but often caused by one.
Actionable Steps: What to Do When the Process Starts
If you suspect a heart attack is starting, there is a very specific sequence of events that can save your life.
- Call emergency services immediately. Do not drive yourself. Paramedics can start an EKG in your living room and transmit it to the hospital so the cath lab is ready before you even arrive.
- Chew an aspirin. Don't just swallow it; chew it. This gets the medicine into your bloodstream faster. Aspirin helps "slick" the platelets, potentially preventing that clot from getting any bigger. A standard 325mg dose is the usual recommendation, but check with your doctor beforehand if you have a known allergy or bleeding risk.
- Sit down and stay calm. Try to lower your heart's oxygen demand. Don't pace. Don't try to "walk it off."
- Know your numbers. If you know you have high C-Reactive Protein (a marker of inflammation) or high Calcium Scores, you need to be on high alert.
Understanding how does a heart attack start isn't about memorizing a textbook; it's about recognizing that your body is a complex system that gives off subtle warnings before the system crashes.
If you have a family history, talk to a cardiologist about a Calcium Score test (CT Heart Scan). It’s a quick, non-invasive way to see if you actually have those "blisters" building up in your pipes before they ever have a chance to rupture. Prevention is always quieter than the cure.