You're sitting on the couch, maybe scrolling through your phone or watching a rerun, and there’s this... tightness. It’s not a sharp, stabbing pain like a Hollywood actor clutching his chest and falling over a coffee table. It’s more like an elephant is casually sitting on your sternum. Or maybe it’s just bad heartburn from those tacos you had earlier. You wait. You wonder. How do you know if your having a heart attack or if you just need an antacid?
The truth is often messy.
Medical professionals will tell you that the "classic" symptoms are actually just one version of the story. Dr. Sharonne Hayes, a cardiologist at the Mayo Clinic, has spent years pointing out that many people—especially women—experience myocardial infarction in ways that feel completely unrelated to the heart. It’s a silent, creeping dread rather than a lightning bolt. If you're waiting for the "big one" to hit before you call 911, you might be waiting too long.
Why it feels different for everyone
The biological reality is that your nervous system is a bit of a tangled web. When the heart muscle begins to die because it's starved of oxygenated blood—usually due to a ruptured plaque in a coronary artery—the pain signals don't always go straight to "Point A." They radiate.
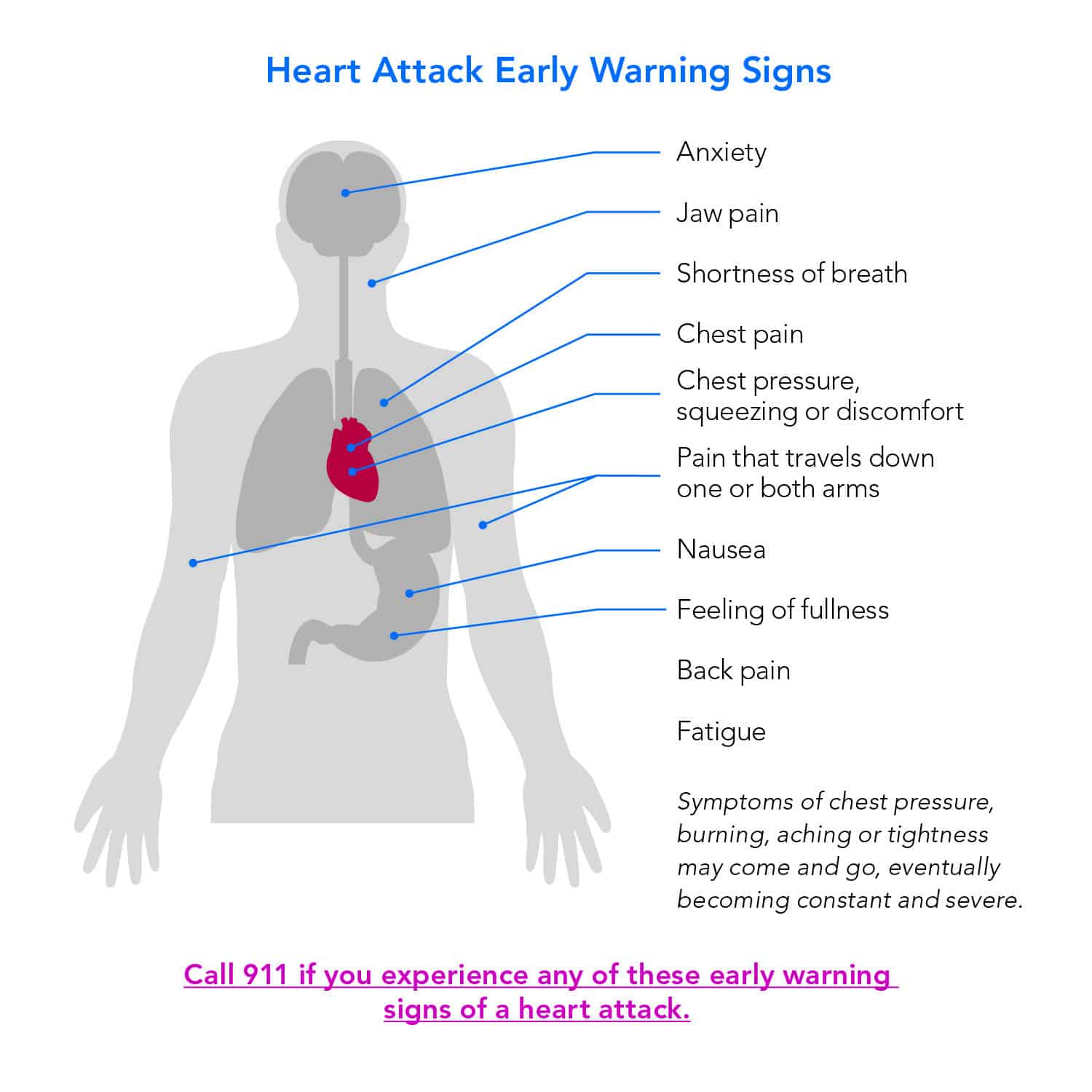
Think about the jaw. Why would your teeth ache during a cardiac event? It's referred pain. The vagus nerve and other pathways get overwhelmed, and your brain interprets the signal as coming from your neck, your shoulders, or even your upper back. I've talked to patients who thought they just pulled a muscle at the gym three days prior. They weren't clutching their chests; they were rubbing their left elbows.
Men often get the "Hollywood" version. Pressure, squeezing, and that radiating pain down the left arm. But for women, diabetics, and the elderly, the symptoms are sneakier. You might just feel "off." A profound, bone-deep exhaustion that makes it hard to walk across the room. Nausea that feels like a stomach flu. Shortness of breath that doesn't go away when you sit down.
✨ Don't miss: I'm Cranky I'm Tired: Why Your Brain Shuts Down When You're Exhausted
The nuance of chest discomfort
It isn't always "pain." People describe it as fullness, squeezing, or a heavy weight. If the sensation lasts for more than a few minutes—or if it goes away and then comes back with a vengeance—that’s a massive red flag.
Don't ignore the sweat. We aren't talking about the kind of sweat you get after a jog. This is a cold, clammy moisture that breaks out while you're resting. If you’re sitting in an air-conditioned room and suddenly look like you’ve been standing in a rainstorm, your body is screaming at you.
How do you know if your having a heart attack or just anxiety?
This is the billion-dollar question in every Emergency Room. Panic attacks and heart attacks have a Venn diagram that is almost a circle. Both cause a racing heart. Both cause sweating. Both cause a sense of impending doom.
However, there are clues.
A panic attack usually peaks within about 10 minutes. Heart attack symptoms tend to persist or worsen over time. Also, position matters. If you can change the intensity of the pain by moving your body, twisting, or taking a deep breath, it might be musculoskeletal or pleuritic. Heart attack pain usually doesn't care if you're standing, sitting, or lying on your side; it remains a constant, crushing presence.
🔗 Read more: Foods to Eat to Prevent Gas: What Actually Works and Why You’re Doing It Wrong
But honestly? Doctors would much rather tell you it’s a panic attack in the ER than have a coroner explain why you stayed home. The phrase "better safe than sorry" is a cliché for a reason.
Real-world indicators to watch for:
- Pressure in the center of the chest: Not always on the left.
- Lightheadedness: Feeling like you might actually faint.
- Discomfort in the "V": That area from your jaw down to your belly button.
- Sudden Fatigue: Not "I didn't sleep well" tired, but "I can't lift my arms" tired.
The window of opportunity
Time is muscle. That’s the mantra in cardiology. From the moment that artery is blocked, heart cells begin to die. You have a "golden hour" to get to a hospital where they can perform a percutaneous coronary intervention (PCI)—basically, popping a balloon in the artery to restore flow.
Wait.
If you wait four hours because you're embarrassed about making a scene, you're looking at permanent scarring of the heart tissue. This leads to heart failure later in life. It’s not just about surviving the day; it’s about what your quality of life looks like five years from now.
What about "Silent" heart attacks?
About 20% of heart attacks go unnoticed at the time. These are the "silent" ones. You might think you had a bad bout of indigestion or a weird flu. Later, an EKG for a routine physical shows damage you didn't even know you had. This is particularly common in people with diabetes, as high blood sugar can damage the nerves that carry pain signals, effectively "muting" the alarm system.
💡 You might also like: Magnesio: Para qué sirve y cómo se toma sin tirar el dinero
Actionable steps if you suspect trouble
If you are reading this because you feel weird right now: stop reading and call emergency services. Do not drive yourself. If you black out behind the wheel, you’re a danger to everyone else. Paramedics can start treatment the second they walk through your door, including performing an EKG and administering aspirin.
If you're in a "maybe" situation, here is the protocol:
- Call 911 (or your local emergency number). Don't call your doctor. Don't call your sister. Call the people with the sirens.
- Chew an aspirin. Unless you're allergic, chew a full-strength (325mg) or four baby aspirins. Chewing it gets it into your bloodstream faster than swallowing it whole. It helps thin the blood and can potentially break up the clot.
- Sit down and stay calm. Try to slow your breathing. Do not try to "walk it off." Physical exertion puts more demand on an already struggling heart.
- Unlock your front door. If you lose consciousness, you want the EMTs to be able to get in without breaking the door down.
When you get to the hospital, be blunt. Don't say "I have some chest discomfort." Say, "I think I'm having a heart attack." This triggers a specific triage protocol that moves you to the front of the line.
The medical community, including organizations like the American Heart Association (AHA), emphasizes that the "wait and see" approach is the leading cause of pre-hospital cardiac death. We have the technology to stop a heart attack in its tracks, but we can't use it if you're still sitting on your couch wondering if it's just the tacos.
Listen to your gut. If something feels profoundly wrong, it probably is. Your body has a way of knowing things before your brain catches up. Trust that instinct.
Immediate Next Steps:
- Check your medicine cabinet for unexpired aspirin today so you have it if needed.
- Save your local emergency number and the address of the nearest "Chest Pain Center" (a specialized ER) in your phone.
- If you have risk factors like high blood pressure or smoking, schedule a calcium score test or a stress test with a cardiologist to understand your baseline.