You're scrolling through your phone late at night, staring at a cluster of tiny, red spots on your toddler's palm. You feel that sinking sensation in your stomach. Is it just a heat rash, or is this the start of something that's going to keep the whole house awake for a week? Most parents end up frantically searching for hand foot and mouth disease images because, honestly, the clinical descriptions in medical textbooks don't always match what you see on a wiggly two-year-old. It's stressful. It’s messy. And it’s incredibly common.
Hand, Foot, and Mouth Disease (HFMD) is one of those childhood rites of passage that nobody actually wants to go through. It’s usually caused by the coxsackievirus A16 or Enterovirus 71. While it sounds terrifying—sort of like something that should only happen on a farm—it’s a human virus that has nothing to do with animals.
Spotting the Early Signs (Before the Rash Hits)
The tricky thing about HFMD is that the spots aren't usually the first thing you notice. It starts with a vibe. Your kid might be cranky, refusing their favorite snacks, or just running a low-grade fever that won't quit. According to the Centers for Disease Control and Prevention (CDC), the incubation period is roughly three to six days. This means by the time you're looking at hand foot and mouth disease images to confirm your suspicions, the virus has already been hanging out in your home for nearly a week.
One day it’s a sore throat; the next, it’s a full-blown refusal to swallow anything but cold water. This is because the mouth sores—officially called herpangina—often show up first. They aren't just on the tongue. They hide way back on the tonsils and the soft palate. If you take a flashlight and look, you’ll see small red spots that quickly turn into yellowish ulcers with a red ring around them. They look painful because they are.
What Do the Spots Actually Look Like?
When people search for hand foot and mouth disease images, they’re usually looking for the "classic" presentation. But the reality is that HFMD is a bit of a shapeshifter. It doesn't always hit all three areas. Sometimes it's just the mouth. Sometimes it’s just a massive rash on the diaper area that looks suspiciously like a bad case of dermatitis.
🔗 Read more: Why Having Sex in Bed Naked Might Be the Best Health Hack You Aren't Using
The Hands and Feet
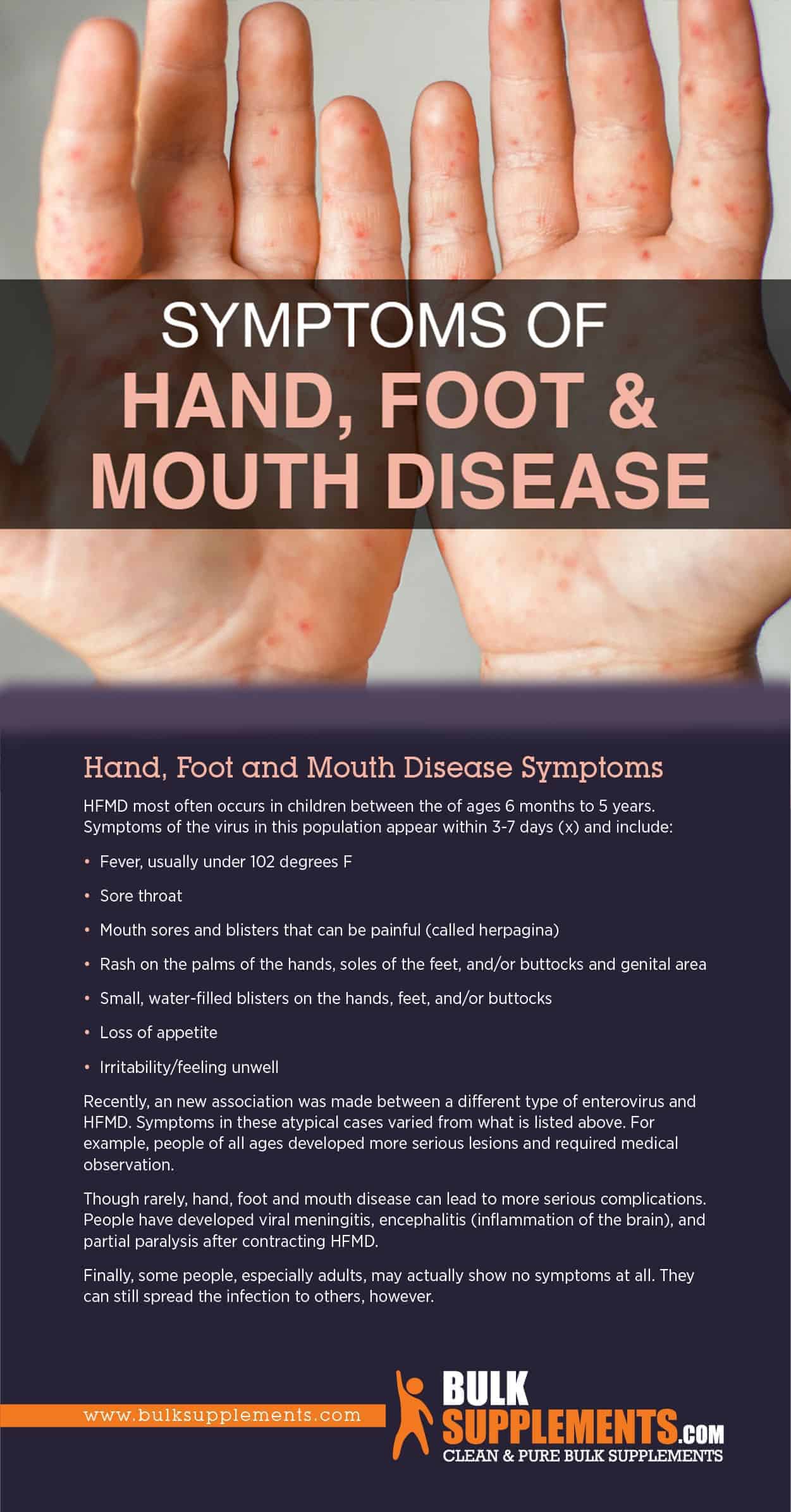
The rash on the hands and feet is distinctive. It’s not usually itchy, which is one way to tell it apart from chickenpox or eczema. Instead, these are small, flat red spots or raised bumps. Sometimes they turn into blisters.
The blisters are often oval-shaped and have a grayish center. If you look closely at high-resolution hand foot and mouth disease images, you’ll notice the "long axis" of the blister often follows the line of the skin. They show up on the palms and the soles of the feet. Most other rashes avoid the palms and soles like the plague, so if you see spots there, it’s a huge red flag for HFMD.
The "Other" Spots
Don't be surprised if the rash shows up in places the name doesn't mention. It loves knees, elbows, and the buttocks. In babies, the diaper area can get absolutely covered. It looks angry. It looks sore. But surprisingly, the skin rash usually bothers the parents more than the kids—it’s those mouth ulcers that cause the real misery.
Is it Getting Worse? New Strains and Different Looks
In recent years, doctors have seen a rise in "atypical" HFMD, often linked to Coxsackievirus A6. This version is a bit of a jerk. It produces a much more widespread rash. It might look like "eczema coxsackium," where the virus targets skin already weakened by eczema.
💡 You might also like: Why PMS Food Cravings Are So Intense and What You Can Actually Do About Them
If you're looking at hand foot and mouth disease images and seeing large, fluid-filled bullae (basically giant blisters) or widespread skin peeling, you might be dealing with this A6 strain. It’s more intense, and it doesn't follow the rules. Adults are also more likely to catch this version. Trust me, if you’re an adult with HFMD, you’ll know it—it feels like walking on shards of glass.
Why the "Peeled" Look Happens Later
About three to four weeks after the initial infection, something weird might happen. You might notice your child's fingernails or toenails starting to peel or even fall off. This is called onychomadesis. It’s terrifying if you don’t know it’s coming, but it’s actually a common, harmless after-effect of the virus. The nail almost always grows back perfectly fine.
The skin on the fingers and toes might also peel in large sheets. This is just the body's way of clearing out the damaged tissue where the blisters were. It doesn't mean the infection is back; it just means the skin is regenerating.
Telling the Difference: HFMD vs. Other Rashes
It’s easy to get confused when you’re looking at pictures online. A few things to keep in mind:
📖 Related: 100 percent power of will: Why Most People Fail to Find It
- Chickenpox: These blisters are usually very itchy and start on the torso before spreading. HFMD starts with the mouth and extremities.
- Measles: This comes with a very high fever, a nasty cough, and runny nose. The rash starts at the hairline and moves down. It doesn't usually blister.
- Impetingo: This bacterial infection usually has a "honey-colored" crust and is often found around the nose and mouth, but it doesn't typically appear on the palms or soles.
Managing the Chaos at Home
Since this is a virus, antibiotics won't touch it. It’s all about symptom management. The main goal is preventing dehydration. When those mouth sores are active, swallowing is a nightmare.
- Cold is your friend. Milkshakes, popsicles, and ice-cold water are much easier to handle than warm soups or acidic juices like orange or apple juice.
- Pain relief. Acetaminophen or ibuprofen (following your pediatrician's dosing) can make a world of difference. It takes the edge off the mouth pain so they can actually drink.
- Soft foods. Think yogurt, pudding, or lukewarm pasta. Avoid anything salty or spicy—it’ll sting like crazy.
How to Stop the Spread (Or Try To)
The virus is shed in saliva, mucus, and feces. It’s incredibly hardy. It can live on a plastic toy for days. This is why it rips through daycare centers like wildfire.
Handwashing is the big one. Wash your hands after every diaper change, even if you think you didn't touch anything. Disinfect "high-touch" surfaces like doorknobs and remote controls. If your child has it, they should stay home until the fever is gone and the blisters have dried up.
When to Call the Doctor
Most cases of HFMD are mild and resolve on their own within seven to ten days. However, you should pick up the phone if:
- Your child hasn't urinated in 8-12 hours (a sign of dehydration).
- The fever lasts more than three days or is exceptionally high.
- Your child seems unusually lethargic or is difficult to wake up.
- The skin looks infected (increased redness, swelling, or pus leaking from the blisters).
Actionable Steps for the Next 48 Hours
If you've just confirmed the diagnosis by comparing your child's spots to hand foot and mouth disease images, here is your immediate plan of action:
- Audit the Fridge: Stock up on non-acidic, cold liquids and soft treats. Think slushies and smoothies.
- Separate the Toys: If you have other children, try to keep the infected child's toys separate and wash them in hot, soapy water or a mild bleach solution.
- Monitor Fluid Intake: Keep a log of how much they are drinking. If they are only taking small sips, that's okay, as long as it's frequent.
- Check Your Own Skin: Keep an eye on your own hands and throat. While adults get it less often, it's definitely possible, and it’s usually more painful for us.
- Notify the School: Let the teacher or daycare provider know immediately so they can ramp up their cleaning protocols.
Dealing with HFMD is exhausting, but it is temporary. Once the blisters dry and the appetite returns, life gets back to normal pretty quickly. Just keep the popsicles stocked and the hand sanitizer ready.