It starts as a dull gnaw. Maybe you think it’s just the coffee you had on an empty stomach or perhaps that deadline-induced stress finally catching up with your gut. But then the bloating hits, and it isn't the "I ate too much pasta" kind of bloat; it’s the "my stomach is an overinflated basketball" kind. If you are looking for clarity on gastritis symptoms in females, you’re likely already dealing with that specific, burning discomfort right below your ribs.
Gastritis is basically just a fancy medical term for inflammation. Specifically, the inflammation of your stomach lining. While the biology of a stomach is the same regardless of gender, women often experience and report symptoms that get tangled up with other issues like hormonal shifts, pelvic pain, or even gallbladder trouble. It’s annoying. It’s painful. And honestly, it’s often misdiagnosed as "just stress" for way too long.
The Burning Truth About Gastritis Symptoms in Females
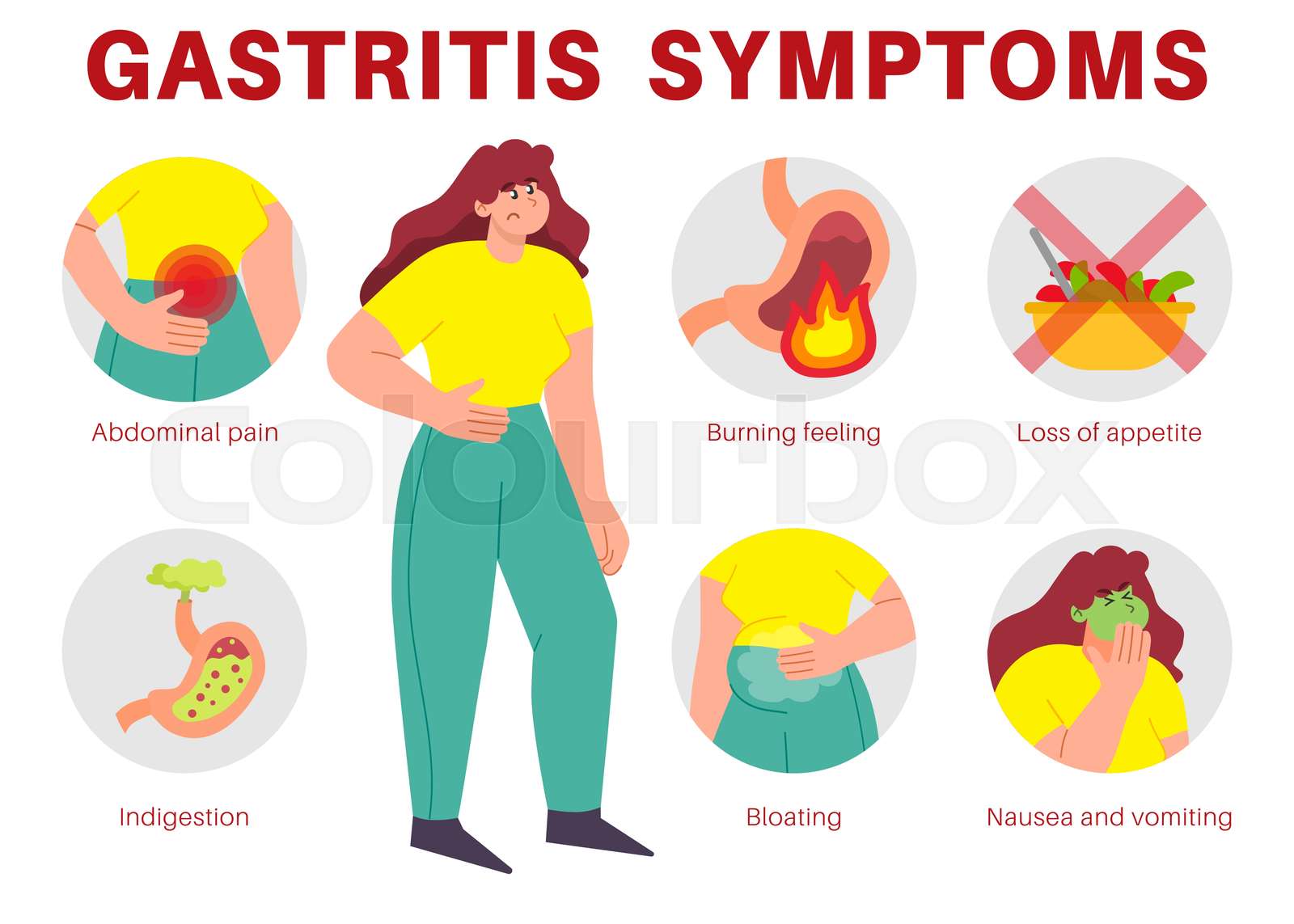
The most common sign is that classic burning sensation in the upper abdomen. Doctors call it dyspepsia. You probably call it "my chest is on fire but it's not a heart attack." This pain often changes based on when you last ate. For some women, eating makes it better because the food buffers the acid. For others? A single bite of anything—even a plain cracker—feels like pouring gasoline on a campfire.
Nausea is another big one. It’s not always the "I’m going to throw up" kind of nausea, though that happens. Often, it’s a lingering, low-grade queasiness that makes you lose your appetite entirely. You might feel full after only three bites of dinner. This "early satiety" is a huge red flag for doctors because it suggests the stomach lining is so irritated it can’t expand properly or move food along the digestive tract at a normal pace.
Then there is the bloating. In women, this is particularly tricky. Because of our menstrual cycles, we are used to a certain amount of puffiness. But gastritis bloating feels higher up, right under the breastbone. It’s frequently accompanied by excessive burping. Like, an embarrassing amount of burping that happens even if you haven't touched a carbonated drink in weeks.
Why Hormones Make Things More Complicated
Let’s talk about estrogen. It’s not just for reproductive health; it actually plays a role in how your gut functions. Some research suggests that fluctuations in progesterone and estrogen can affect gastric emptying—how fast food leaves your stomach. When your period is about to start, or during pregnancy, those shifts can make gastritis symptoms in females feel significantly more intense.
👉 See also: Understanding MoDi Twins: What Happens With Two Sacs and One Placenta
Prostaglandins are another culprit. These are hormone-like substances that help your uterus contract during your period. The problem? They can also cause contractions in your intestines and stomach. If your stomach lining is already inflamed from gastritis, these extra contractions feel like a localized earthquake. This is why many women find their "stomach issues" flare up like clockwork every month. It’s a double whammy of inflammation and hormonal sensitivity.
What’s Actually Causing the Fire?
You don't just wake up with an inflamed stomach for no reason. Usually, there’s a villain. The most frequent offender is a bacteria called Helicobacter pylori (H. pylori). It’s incredibly common—nearly half the world has it—but in some people, it burrows into the mucus layer of the stomach and starts wreaking havoc.
Then there are NSAIDs. Think ibuprofen, naproxen, or aspirin. Women are statistically more likely to suffer from chronic pain conditions like migraines or menstrual cramps, leading to a higher consumption of these over-the-counter painkillers. They work by blocking enzymes that cause pain, but those same enzymes are responsible for maintaining the protective lining of your stomach. You take the pill to stop the cramp; the pill eats the stomach lining. It's a frustrating cycle.
- Alcohol and Coffee: Both are irritants. If your lining is already thin, that morning espresso is like rubbing salt in a wound.
- Autoimmune Gastritis: This is a less common version where your own immune system attacks the stomach cells. It’s more prevalent in women and can lead to Vitamin B12 deficiency because your stomach can't absorb it anymore.
- Bile Reflux: Sometimes bile backs up from the small intestine into the stomach. It’s caustic and causes a specific type of intense burning.
The Connection to Stress and Anxiety
We have to address the "it’s just stress" myth. Stress doesn't magically create bacteria or cause autoimmune disease, but it does change how your body handles acid. When you're in "fight or flight" mode, your body diverts blood flow away from the digestive system. This weakens the stomach's defenses. If you already have a mild case of gastritis, a high-stress week can turn it into a full-blown crisis. It’s not "all in your head," but your head is definitely talking to your gut.
How to Tell if It’s Something Else
Because the symptoms of gastritis are so broad, they often overlap with other conditions. This is where it gets confusing for women.
✨ Don't miss: Necrophilia and Porn with the Dead: The Dark Reality of Post-Mortem Taboos
- Gallstones: Pain from gallstones usually hits the upper right side and can radiate to your back or shoulder blade. Gastritis is usually more central.
- GERD (Acid Reflux): Reflux is about the acid coming up into the esophagus. Gastritis is about the inflammation inside the stomach. You can have both, which is just as fun as it sounds.
- Ovarian Cysts: Sometimes lower abdominal pain can be mistaken for digestive issues, though gastritis is almost always higher up in the torso.
- IBD vs. IBS: Irritable Bowel Syndrome (IBS) usually involves lower abdominal cramping and changes in bowel movements (diarrhea or constipation), whereas gastritis is focused on the stomach itself.
Getting a Real Diagnosis
Don't just live on antacids. If you’ve been popping Tums like candy for more than two weeks, you need a doctor. They’ll likely start with a breath or stool test to check for H. pylori. It’s quick and non-invasive.
If things are more serious, they might suggest an endoscopy. I know, the idea of a camera going down your throat is terrifying. But honestly? You’re usually sedated, and it’s the only way for a gastroenterologist to actually see the redness, the erosions, or any ulcers that might have formed. They can also take a tiny biopsy to rule out anything scary like stomach cancer or specific infections.
Actionable Steps to Cool the Flame
If you are dealing with gastritis symptoms in females, you need a multi-pronged approach. You can't just change one thing and expect a miracle. It’s about creating an environment where your stomach lining can actually heal.
Change the Way You Eat
Stop eating three massive meals. Your stomach can't handle the volume when it’s inflamed. Switch to five or six tiny meals. This keeps a small amount of food in the stomach to buffer acid without overextending the stomach wall. Avoid the "Big Three" irritants for at least a month: spicy foods, high-acid citrus/tomatoes, and caffeine. Also, watch out for "hidden" fats. Fried foods linger in the stomach longer, meaning more acid production and more pain.
Review Your Medicine Cabinet
If you’re taking ibuprofen for every headache, stop. Talk to your doctor about switching to acetaminophen (Tylenol), which doesn't affect the stomach lining the same way. If you absolutely must take an NSAID, never do it on an empty stomach.
🔗 Read more: Why Your Pulse Is Racing: What Causes a High Heart Rate and When to Worry
Natural Support That Actually Works
Zinc carnosine is a supplement that has some legitimate backing for gut lining repair. Slippery elm or marshmallow root tea can also provide a temporary "bandage" effect by coating the esophagus and stomach in a soothing mucilage. It's not a cure, but it can make getting through the day easier.
Manage the "Brain-Gut" Axis
Since stress thins the stomach's protective mucus, finding a way to signal "safety" to your nervous system is vital. This isn't "woo-woo" science; it’s physiology. Deep diaphragmatic breathing for five minutes before a meal can switch your body from sympathetic (stress) to parasympathetic (digest) mode. It makes a difference.
Moving Forward
Healing from gastritis isn't overnight. It took time for the lining to wear down, and it will take time for it to knit back together. Most people see significant improvement within 2 to 4 weeks of strict dietary changes and medication (like PPIs or H2 blockers) if prescribed.
Immediate Next Steps:
- Start a food and symptom diary. Note down exactly what you ate and how you felt two hours later. Look for patterns involving dairy, gluten, or high-fat meals.
- Book an appointment for an H. pylori breath test. It is the most common cause and the easiest to treat with a specific round of antibiotics.
- Switch your morning coffee to a low-acid herbal tea like chamomile or ginger to give your stomach a "rest day" from chemical irritants.
- Check your B12 levels if you’ve been feeling unusually fatigued along with your stomach pain; chronic gastritis often leads to malabsorption issues that require supplementation.
Gastritis is a physical condition with clear causes and clear treatments. You don't have to just "deal with" the burning. By identifying the triggers and addressing the underlying inflammation, you can actually get back to a life where you aren't constantly thinking about your stomach.