You're lying in bed, the sheets feel like sandpaper against your skin, and every bone in your body aches as if you’ve just run a marathon you never signed up for. That’s the flu. It isn’t a "bad cold." It’s a systemic inflammatory event that shuts people down. Every year, we hear the same buzz about the flu vaccine, and honestly, it’s easy to tune it out. We get busy. We forget. Or maybe we had a bad experience once and decided it wasn't worth the hassle. But here’s the thing: influenza is a shape-shifter, and the science behind how we fight it is more nuanced than most people realize.
The virus doesn't care about your schedule. It’s looking for a host. Specifically, it’s looking for a way to hijack your respiratory cells and turn them into tiny factories for more virus particles. The flu vaccine is essentially a "Most Wanted" poster for your immune system, but because the virus mutates faster than almost any other pathogen we track, that poster has to be updated every single year.
The Reality of How the Flu Vaccine Actually Works
Most people think the shot is a magical shield. It isn’t. Think of it more like a specialized training camp for your white blood cells. When you get the flu vaccine, you’re introducing inactivated (dead) virus pieces or specific proteins to your body. Your immune system looks at these "invaders," gets annoyed, and starts building antibodies.
The CDC and organizations like the World Health Organization (WHO) spend the entire year tracking which strains are circulating in the Southern Hemisphere during their winter. They use that data to predict what’s going to hit us. Sometimes they get it exactly right. Other times, like in the 2014-2015 season, a strain called H3N2 mutated after the vaccine was already in production, which dropped the effectiveness significantly. That’s just the nature of biology. It’s a literal arms race between human ingenuity and viral evolution.
But here is the part that gets lost in the headlines: even if the match isn't perfect, the flu vaccine often prevents the most "catastrophic" outcomes. There’s this concept called "prime-boost" or "cross-reactivity." Even if you still get sick, those antibodies you built from the shot can recognize parts of the virus, making the illness shorter and significantly less likely to land you in the ICU.
Why We Can't Just Get One Shot and Be Done
Why do we need a new flu vaccine every year? Why can't it be like polio or measles where you get your shots as a kid and you're mostly good for life?
👉 See also: Magnesio: Para qué sirve y cómo se toma sin tirar el dinero
Antigenic drift.
That’s the technical term for the small genetic changes that happen as the virus replicates. Influenza is sloppy. When it copies its genetic code, it makes mistakes. Most of those mistakes are useless, but occasionally, a mistake changes the shape of the proteins on the surface of the virus—the hemagglutinin (H) and neuraminidase (N). Suddenly, the antibodies your body made last year don't "fit" the new shape of the virus. It’s like trying to put a key into a lock that someone has jammed a toothpick into.
Then there’s "antigenic shift," which is much scarier. That’s when two different flu viruses infect the same cell (usually in a pig or a bird) and swap entire chunks of DNA. This creates a brand-new subtype that no human has immunity to. That’s how pandemics start. This is why the global surveillance network is so obsessed with tracking avian and swine flu; we need to know the moment the virus changes its "costume" entirely.
Common Misconceptions That Just Won't Die
"The shot gave me the flu."
No, it didn't. It’s physically impossible for the injectable flu vaccine to give you the flu because the virus in the needle is dead. Now, the nasal spray (FluMist) uses a weakened "live" virus, but even that is engineered to only replicate in the cooler temperatures of your nose, not your warm lungs.
✨ Don't miss: Why Having Sex in Bed Naked Might Be the Best Health Hack You Aren't Using
So why do people feel like garbage after the shot?
- Your immune system is working. That low-grade fever or arm soreness is actually proof that your body is responding to the vaccine.
- Bad timing. It takes about two weeks for the flu vaccine to provide full protection. If you were exposed to a virus in the pharmacy waiting room, you might get sick before the shot kicks in.
- Other bugs. There are hundreds of respiratory viruses (like RSV or rhinoviruses) that circulate at the same time as the flu. People get a cold, assume it’s the flu, and blame the vaccine.
High-Dose vs. Standard: Does Age Matter?
If you’re over 65, the standard flu vaccine might not be enough. As we age, our immune systems go through something called immunosenescence. Basically, our internal "army" gets a little slower and less reactive.
This is why the Fluzone High-Dose or the adjuvanted vaccine (Fluad) exists. These versions contain four times the amount of antigen or a specific ingredient called an adjuvant that "wakes up" the immune system. A study published in the New England Journal of Medicine showed that the high-dose version was 24.2% more effective in preventing the flu in seniors compared to the standard dose. If you’re in that age bracket, or you're caring for someone who is, you should specifically ask for the "senior shot."
What About the "Universal" Vaccine?
The holy grail of infectious disease research is the universal flu vaccine. Imagine a shot you get once every ten years that covers every strain of influenza A and B. Researchers at places like the NIH’s Vaccine Research Center are looking at the "stalk" of the flu protein.
While the "head" of the virus protein changes constantly (drift), the "stalk" stays relatively the same across different strains. The problem is that our bodies naturally ignore the stalk and focus on the head. Scientists are trying to find ways to force our immune systems to target that stable stalk. We aren't there yet, but the progress in mRNA technology—the same tech used for COVID-19—is accelerating this research.
🔗 Read more: Why PMS Food Cravings Are So Intense and What You Can Actually Do About Them
Real World Impact: It’s Not Just About You
There's a lot of talk about "herd immunity," but with the flu, it’s really about protecting the vulnerable people in your immediate orbit. When you get the flu vaccine, you’re creating a dead-end for the virus.
Think about infants under six months old. They are too young to get the vaccine. They rely entirely on the "cocoon" of vaccinated people around them. Or consider people undergoing chemotherapy. Their immune systems are decimated; they can't fight off a "mild" case of the flu. For them, your decision to get vaccinated is a matter of life and death. In the 2022-2023 season, the CDC estimated that flu vaccination prevented roughly 65,000 hospitalizations in the U.S. alone. That’s a stadium full of people who stayed home instead of being hooked up to monitors.
How to Handle a Flu Infection if it Hits
Sometimes, despite your best efforts, the virus wins. If you start feeling that sudden onset of fever, chills, and cough, time is of the essence.
Antiviral medications like Oseltamivir (Tamiflu) or the newer Baloxavir (Xofluza) work by blocking the virus from exiting your cells and spreading to others. But—and this is a big but—they really only work if you start them within 48 hours of your first symptoms. If you wait until day four, you’re basically just paying for expensive side effects.
Hydration is non-negotiable. When you have a fever, you lose fluid through your skin and breath much faster than normal. If your urine isn't pale yellow, you aren't drinking enough. And please, for the love of everyone around you, stay home. A "hero" who comes to work sick is just a biological hazard in a necktie.
Actionable Steps for Flu Season
Don't wait until the local news starts reporting on hospital surges. Proactivity is the only way to win this.
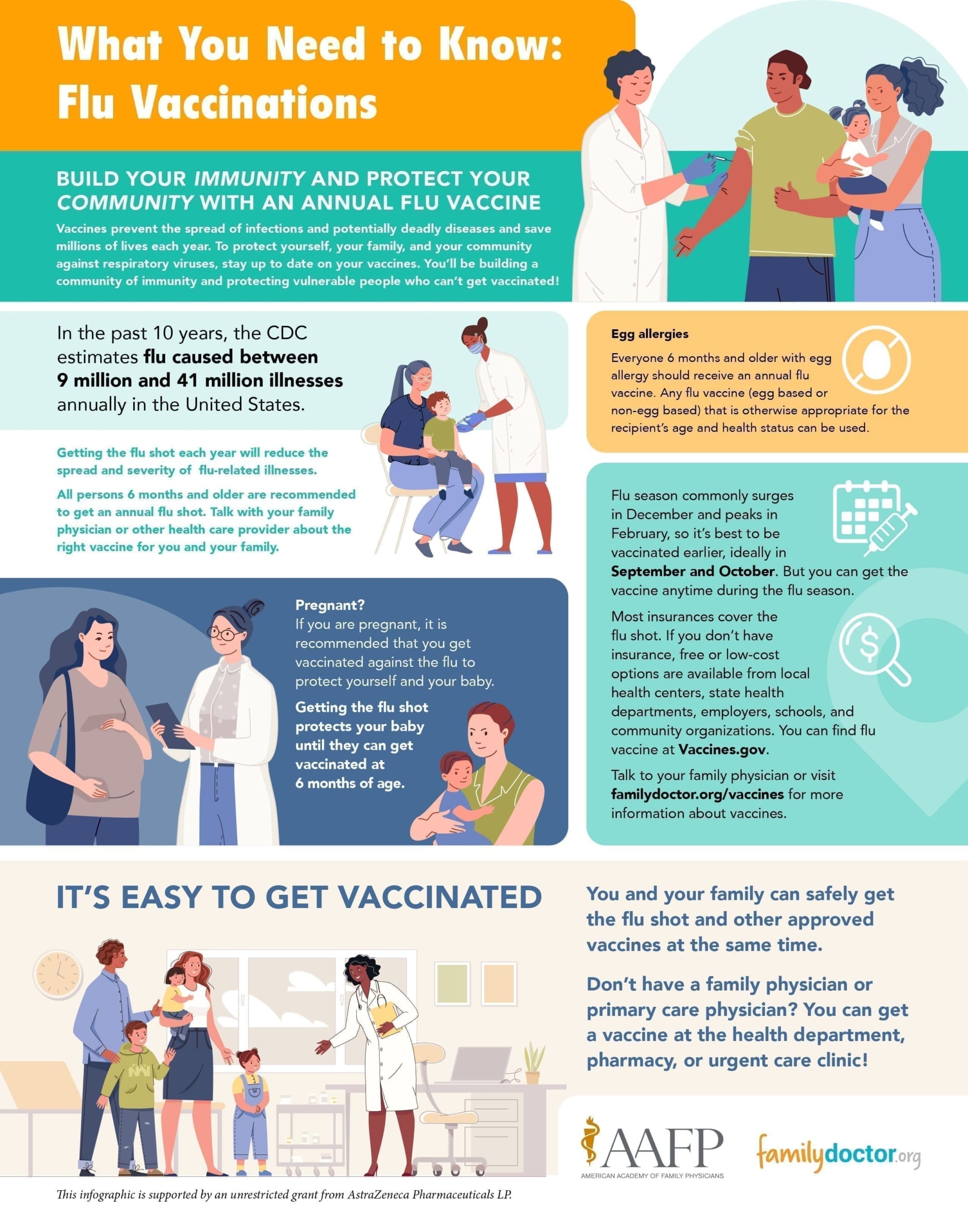
- Check the timing. Late September through October is usually the "sweet spot" for the flu vaccine. If you get it too early (like July), your immunity might wane before the late-season surge in February or March.
- Locate the right version. If you have a severe egg allergy, ask for the cell-based or recombinant vaccine (like Flucelvax or Flublok), which doesn't use chicken eggs in the manufacturing process.
- Audit your medicine cabinet. Check expiration dates on Ibuprofen or Acetaminophen. You don't want to be hunting for a thermometer at 3:00 AM when your head is spinning.
- Optimize your environment. The flu virus survives longer in dry, cold air. Using a humidifier to keep your indoor humidity between 40% and 60% can actually help reduce the stability of viral particles in the air.
- Wash your hands—properly. Not a three-second rinse. Use soap, friction, and twenty seconds. The virus has a lipid (fatty) envelope that soap literally pulls apart, destroying the virus on contact.
Influenza has been with us for centuries, and it’s not going anywhere. It’s a relentless, evolving machine. But with the right tools—mainly the flu vaccine and a bit of common sense—we can make sure it doesn't do the damage it’s capable of. Take the half hour out of your day to get the shot. Your future self, and the people you encounter in the grocery store, will thank you.