A positive pregnancy test usually sparks a mix of adrenaline, joy, or maybe some healthy terror. But sometimes, things go sideways—literally. When we talk about what is meant by ectopic pregnancy, we’re talking about a biological mistake where a fertilized egg decides to set up shop anywhere except the uterus.
It’s scary. It’s also fairly common, affecting roughly 1 out of every 50 pregnancies in the United States.
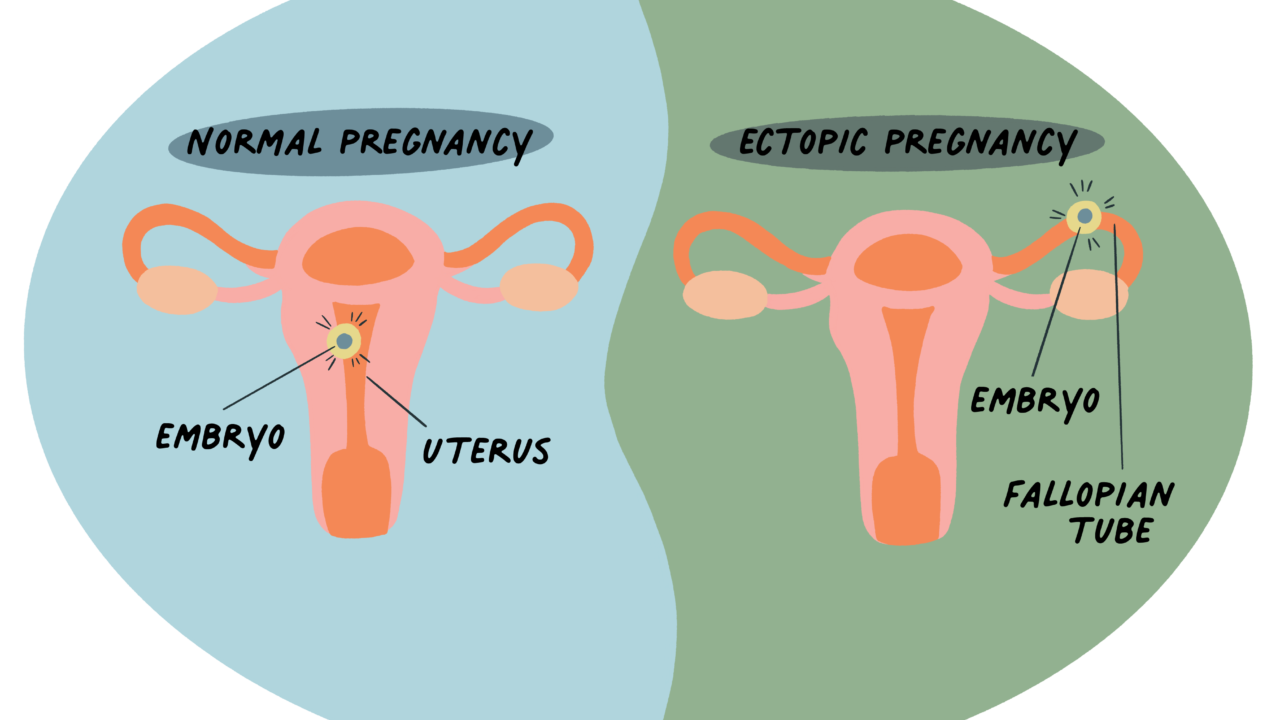
Normally, the egg meets the sperm in the fallopian tube. They hit it off, and the resulting embryo travels down into the uterus to snuggle into the lining. In an ectopic pregnancy, that traveler gets stuck. Most of the time, it stays in the fallopian tube, which is why you’ve probably heard people call it a "tubal pregnancy." The problem is that a fallopian tube isn't an expandable nursery; it’s a narrow straw. It cannot support a growing fetus. If the pregnancy continues, the tube can burst, leading to life-threatening internal bleeding.
Why the "Where" Matters So Much
Location is everything in embryology. While the vast majority of these cases happen in the fallopian tube (about 90%), an embryo can occasionally implant in the ovary, the cervix, or even the abdominal cavity.
Think of the uterus like a specialized balloon. It’s designed to stretch from the size of a lemon to the size of a watermelon. The fallopian tubes? Not so much. They are delicate structures meant for transport, not storage. When a pregnancy starts growing there, it’s essentially a ticking clock. Because the embryo cannot survive outside the uterine environment, and because it poses a direct physical threat to the person carrying it, an ectopic pregnancy is never a viable pregnancy. That’s a hard reality to swallow for many, but it is a biological fact.
The Warning Signs People Often Ignore
Early on, it feels like a regular pregnancy. You might have a missed period, tender breasts, and a touch of nausea. But then, things start feeling "off."
👉 See also: Human body anatomy diagram: What most people get wrong about how we’re built
You might notice sharp, stabbing pains on one side of your pelvis. It isn't just a dull ache; it’s often a localized, intense sensation that comes and goes. Then there’s the spotting. Many people mistake ectopic bleeding for a weirdly light period or "implantation bleeding." Honestly, if you have a positive pregnancy test and start bleeding—even if it's just brown smudges—you need to call a doctor.
One of the weirdest symptoms is shoulder tip pain. It sounds totally unrelated, right? But if a fallopian tube starts leaking blood into the abdomen, it can irritate the phrenic nerve. That nerve sends a "danger" signal that your brain interprets as pain in your shoulder blade. If you feel that, along with dizziness or fainting, it is a medical emergency. Go to the ER. Seriously.
What Actually Causes This?
It’s rarely anyone’s "fault." Most of the time, it’s about a physical roadblock or a slow-moving egg.
If the fallopian tube is scarred or misshapen, the embryo gets physically trapped. Inflammation from previous infections, like Pelvic Inflammatory Disease (PID) or certain STIs like chlamydia or gonorrhea, is a major culprit. These infections can leave behind tiny bits of scar tissue that act like speed bumps. Sometimes, the cilia—the tiny hairs that wave the egg toward the uterus—just aren't working right.
- Previous Ectopics: If you’ve had one before, your risk for another is about 10%.
- Fertility Treatments: Procedures like IVF can slightly increase the odds, though doctors aren't 100% sure why.
- Tubal Surgery: If you’ve had your "tubes tied" or had them repaired, the resulting scar tissue can be an issue.
- Smoking: This is a big one. Smoking affects how the fallopian tubes function, making it harder for the egg to move along.
- IUDs: While an IUD is incredibly effective at preventing pregnancy, if you do happen to get pregnant while using one, there is a higher chance it will be ectopic.
Diagnosis: Beyond the Pee Stick
A standard pregnancy test can't tell you where the pregnancy is located. It only detects hCG, the "pregnancy hormone." To figure out what is meant by ectopic pregnancy in a clinical sense, doctors use a combination of tools.
First, they’ll do a blood test to check your hCG levels. In a healthy pregnancy, these numbers usually double every 48 to 72 hours. In an ectopic pregnancy, they often rise more slowly or plateau.
Then comes the transvaginal ultrasound. This is the gold standard. The technician is looking for a gestational sac. If your hCG levels are high enough that a pregnancy should be visible in the uterus, but the uterus is empty, the doctor starts looking at the tubes. Sometimes they find a "blob" or a mass in the adnexa (the area around the uterus), confirming the diagnosis.
Treatment Options and the Reality of Recovery
There is no way to move an ectopic pregnancy into the uterus. Modern medicine just isn't there yet. Because of the risk of rupture, the pregnancy must be removed.
If it’s caught very early and the person is stable, doctors often use a medication called methotrexate. It’s basically a folic acid antagonist that stops the cells from dividing. Your body then reabsorbs the tissue over a few weeks. It’s non-invasive, but it requires a lot of follow-up blood work to make sure the hCG levels drop to zero.
If the pregnancy is further along, or if there’s a risk of rupture, surgery is necessary. Usually, this is done laparoscopically—small incisions, tiny cameras. The surgeon might perform a salpingostomy (removing the pregnancy but leaving the tube) or a salpingectomy (removing the entire tube). If the other tube is healthy, you can still get pregnant naturally in the future.
💡 You might also like: Soothe Relieve Compression Socks: Why Your Feet Still Hurt After a Long Day
The physical recovery from surgery takes a few weeks, but the emotional recovery? That takes longer. Even though the pregnancy wasn't viable, it’s still a loss. It’s okay to grieve.
Looking Forward: Fertility After an Ectopic
One of the most common questions is: "Can I ever have a baby after this?"
Generally, yes.
Data from organizations like the American College of Obstetricians and Gynecologists (ACOG) shows that most women who have had an ectopic pregnancy go on to have healthy, successful pregnancies later. Even with only one fallopian tube, the remaining tube is surprisingly good at "picking up" an egg from either ovary.
✨ Don't miss: The Truth About How to Make Masturbating Feel Better
However, because the risk of a repeat occurrence is higher, your next pregnancy will be monitored very closely from day one. You'll likely get an ultrasound at the 6-week mark just to confirm the embryo is in the right place. It’s a bit of extra stress, but it’s for your safety.
Immediate Action Steps
If you suspect you are experiencing an ectopic pregnancy, do not "wait and see." Time is the most critical factor in avoiding surgery or permanent damage.
- Monitor Pain Patterns: Track if the pain is localized to one side or if it’s migrating to your shoulder.
- Get a Quantitative hCG Test: Ask your doctor for blood work, not just a urine test, to see how your hormone levels are trending over 48 hours.
- Confirm Placement Early: If you have a history of PID, smoking, or a previous ectopic, insist on an early placement ultrasound between 5 and 6 weeks of pregnancy.
- Know the ER Signs: If you feel sudden, severe abdominal pain, extreme lightheadedness, or fainting, head to the nearest emergency room immediately. These are signs of a rupture.
- Review Your History: Gather your medical records regarding any past pelvic surgeries or infections to help your provider assess your specific risk profile.