It happens fast. You’re sitting on the couch, maybe you just finished a big meal, or perhaps you haven’t eaten in six hours, and suddenly everything feels... off. Your vision gets a little blurry. Your heart starts doing a weird fluttery dance in your chest. You might feel a bit shaky, or maybe just incredibly, overwhelmingly sleepy. This isn't just "food coma" territory. You might be hitting a dangerous blood sugar level, and honestly, knowing the difference between a "bad day" and a medical crisis is what keeps people out of the ICU.
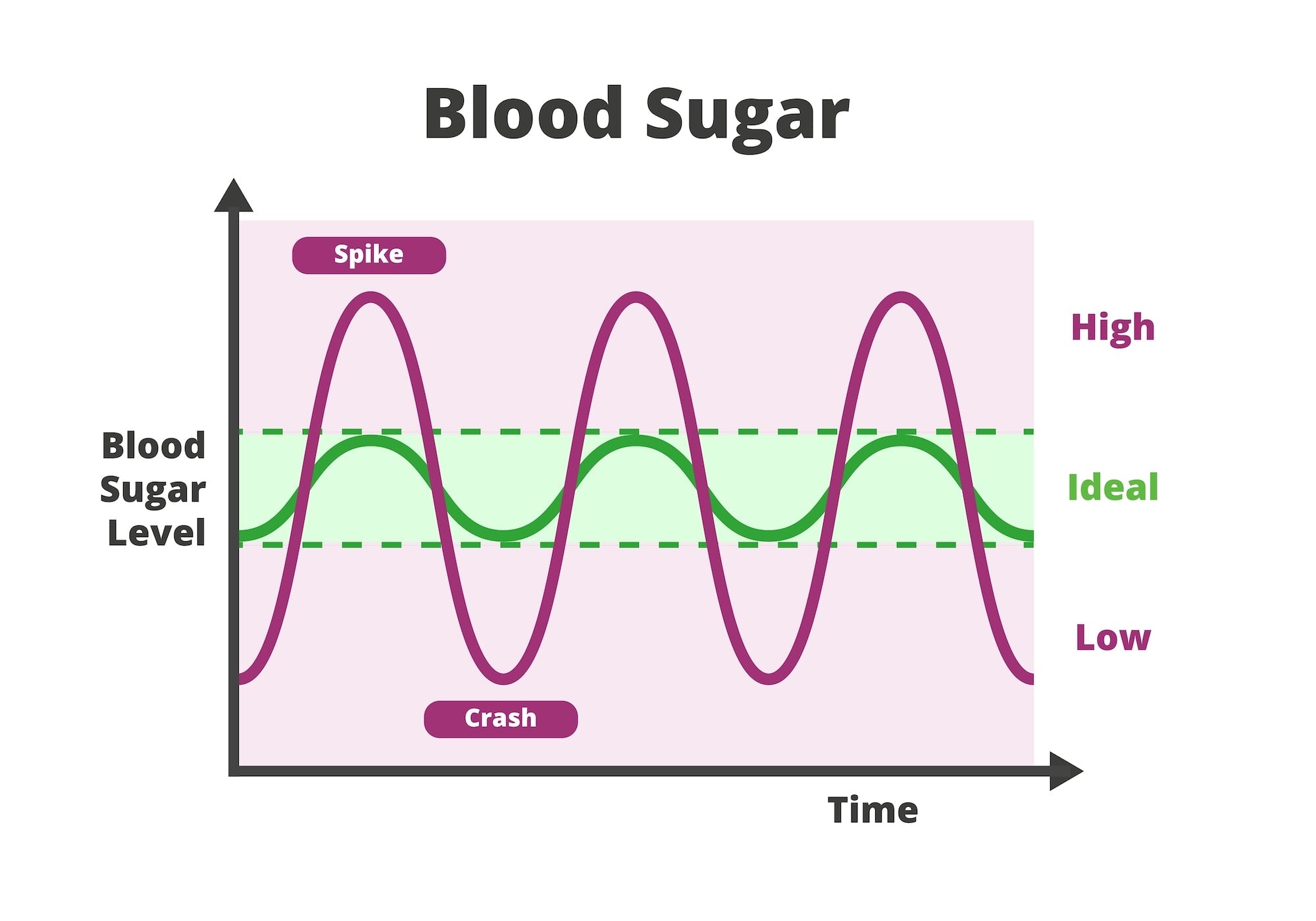
Most folks think blood sugar is just a "diabetes thing." It's not. While people with Type 1 or Type 2 diabetes deal with this daily, anyone can experience spikes or crashes due to medication, severe infection, or even extreme stress. The problem is that our bodies are incredibly sensitive. We operate within a tight window. When you drift outside that window, things break. Fast.
What Does a Dangerous Blood Sugar Level Actually Look Like?
The medical community generally looks at two ends of the spectrum: hypoglycemia (low) and hyperglycemia (high). Both can be lethal, but they kill you in different ways. If your blood sugar drops below 70 mg/dL, you’re entering the danger zone. If it hits below 54 mg/dL, you’re in what doctors call "severely low" territory. This is where your brain stops getting the glucose it needs to function. You might start acting drunk, get confused, or even lose consciousness.
On the flip side, high blood sugar is a slow burn that can turn into a wildfire. A reading over 240 mg/dL is usually the threshold where doctors tell you to start checking for ketones—toxic acids that build up when your body starts burning fat for energy because it can't get to the sugar. If you see 300 mg/dL or higher on a consistent basis, or even as a one-off with symptoms, you are staring down the barrel of Diabetic Ketoacidosis (DKA) or Hyperosmolar Hyperglycemic State (HHS). These aren't just "high" numbers; they are "go to the ER" numbers.
The Low End: Hypoglycemia and the 15-Minute Rule
Low blood sugar is often more immediately terrifying. My friend Sarah, who has lived with Type 1 diabetes for twenty years, describes a "low" as a feeling of impending doom. You’re sweating, but you’re cold. Your hands won't stop shaking.
💡 You might also like: Foods to Eat to Prevent Gas: What Actually Works and Why You’re Doing It Wrong
When your blood sugar hits a dangerous blood sugar level on the low side, the standard protocol is the "15-15 Rule." You eat 15 grams of fast-acting carbs—think a half-cup of juice or some glucose tabs—and wait 15 minutes. You check again. If it’s still low, you do it again. But here’s the kicker: if you can't swallow or if you're drifting in and out of consciousness, someone needs to use a glucagon kit. Don't try to force-feed a person orange juice if they’re passing out; they’ll choke.
The High End: The Dangers of DKA
Hyperglycemia feels different. It’s a heavy, lethargic, thirsty kind of misery. You’ll feel like you could drink a gallon of water and still have a mouth like sandpaper. Why? Because your kidneys are working overtime. They are trying to flush all that excess sugar out through your urine. This leads to massive dehydration.
In 2023, the Journal of the American Medical Association highlighted that DKA cases have been rising, partly because people miss the early warning signs. If your breath smells fruity—almost like nail polish remover or rotting apples—that’s the ketones. It’s a sign your blood is becoming acidic. That is a dangerous blood sugar level that requires IV insulin and fluids. You cannot "walk it off" or just drink more water at home to fix it.
Why Your "Normal" Might Be Someone Else's Crisis
Context matters. This is where the nuance comes in. If you’ve had high blood sugar for years, your body gets "used" to it. Doctors call this a high glycemic set point. If your sugar is usually 250 mg/dL and it suddenly drops to 100 mg/dL (which is technically "normal"), you might feel like you're crashing. You'll get the shakes and the sweats.
📖 Related: Magnesio: Para qué sirve y cómo se toma sin tirar el dinero
Conversely, some people have "hypoglycemia unawareness." This is genuinely scary. It means your body has stopped sending out the adrenaline signals that tell you you're low. You could be sitting at a desk with a blood sugar of 45 mg/dL, feeling totally fine, right up until the moment you have a seizure. This is why Continuous Glucose Monitors (CGMs) like the Dexcom or Freestyle Libre have been absolute game-changers. They alert you before you hit the cliff.
Real Talk: When to Call 911
If you're looking at a monitor and the number is screaming at you, look at the person, not just the machine. Technology fails. Sensors glitch. But if you see these "Red Flag" symptoms alongside a dangerous blood sugar level, stop reading and call for help:
- Confusion or Combativeness: If they're acting like they've had six shots of tequila but haven't touched a drop.
- Persistent Vomiting: If you can't keep fluids down and your sugar is high, you're headed for DKA fast.
- Deep, Rapid Breathing: Known as Kussmaul breathing. It's the body's way of trying to blow off carbon dioxide to compensate for the acidity in the blood.
- Seizures or Fainting: This is non-negotiable.
The Role of "Hidden" Spikes
We talk a lot about the obvious stuff like candy or soda, but some of the most dangerous blood sugar level spikes come from things you wouldn't expect. Steroid medications (like prednisone) are notorious for sending blood sugar into the stratosphere. Severe infections, like a UTI or pneumonia, trigger a stress response in the body that dumps stored glucose into the bloodstream.
I’ve seen patients who were normally well-controlled suddenly hit 400 mg/dL because they had a silent infection they didn't even know about. The body is an interconnected system. If one part is under siege, your glucose is going to react.
👉 See also: Why Having Sex in Bed Naked Might Be the Best Health Hack You Aren't Using
Modern Management: Beyond the Fingerstick
We live in a wild era for medical tech. We have insulin pumps that talk to monitors (closed-loop systems) to prevent a dangerous blood sugar level before it happens. But even with all that, "human error" is real. A bubble in an insulin line, a bad batch of test strips, or even extreme heat can mess with your readings.
Did you know that leaving your insulin in a hot car can make it essentially useless? It's a protein. It "cooks" in the heat. If you're injecting "cooked" insulin, your blood sugar will stay at a dangerous blood sugar level no matter how many units you take. It's these little details that often lead to emergency room visits.
Immediate Actionable Steps for Safety
If you or someone you're with is dealing with a blood sugar reading that looks risky, don't panic, but don't wait.
- Verify the reading. If a CGM says you’re 40 mg/dL but you feel fine, wash your hands and do a manual fingerstick. Sugar on your skin from a piece of fruit can give a false "high," and a compressed sensor can give a false "low."
- Hydrate, but don't overdo it. If you're high, water helps the kidneys, but it doesn't replace the need for insulin.
- Check for Ketones. If you're over 240 mg/dL, use a urine strip. If they are "moderate" or "large," that’s an automatic ER trip.
- The Glucagon Talk. If you're prone to lows, make sure your family/roommates know where the emergency glucagon is. The newer nasal sprays (like Baqsimi) are way easier to use than the old-school needles.
- Audit your "Why." Was it a missed dose? A "hidden sugar" in a restaurant meal? An upcoming flu? Identifying the cause helps prevent the next spike.
Managing your health isn't about being perfect. It's about being aware. A dangerous blood sugar level is a signal from your body that the balance is off. Listen to it. Treat the numbers with respect, but treat the symptoms with urgency. If you're ever in doubt, the ER is there for a reason. It's much better to be sent home with a "you're fine" than to wait until you can't make the call yourself.
Keep a kit ready. Keep your sensors charged. And most importantly, keep your people informed about what to do when you can't help yourself.