When a nurse is caring for a client who has osteoporosis, the room feels different. There’s a specific kind of quiet tension. You aren't just checking vitals or handing out meds. You are essentially walking on eggshells, except the eggshells are the patient's femur or vertebrae. It’s high-stakes nursing.
Osteoporosis is often called a "silent disease" because, honestly, you don't feel your bones getting porous. You don't feel the density slipping away like sand through a sieve until—crack. A sneeze, a trip over a rug, or even just rolling over in bed leads to a fracture. For a nurse, the priority shifts from general wellness to an aggressive, hyper-vigilant form of injury prevention.
The Reality of the "Silent" Break
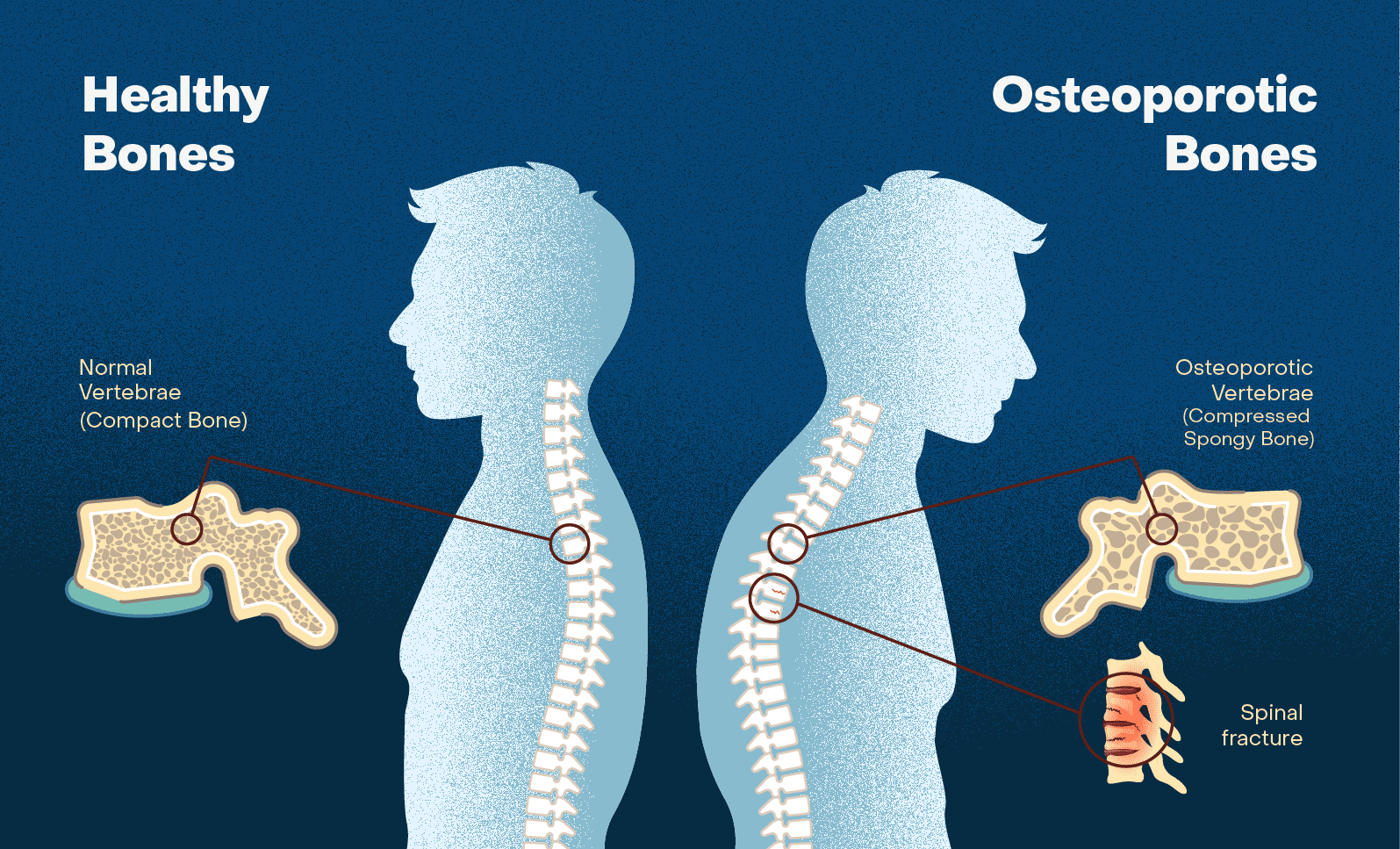
Bone health isn't static. It's a constant tug-of-war between osteoblasts building bone up and osteoclasts tearing it down. In a client with osteoporosis, the wrecking crew is winning.
When you’re at the bedside, the first thing you notice isn't the bone density score. It’s the posture. You’ll see that classic kyphosis—the "dowager’s hump"—which isn't just a cosmetic issue. It’s a sign that the vertebrae have already begun to collapse. This changes everything about how a nurse interacts with the patient. You can't just "help them up." You have to use a draw sheet. You have to move with a level of intentionality that avoids any shearing force on the spine.
I remember a specific case involving an 82-year-old woman. She was admitted for a respiratory infection, but her primary underlying struggle was severe bone loss. Every time she coughed, the nursing staff winced. We weren't just worried about her lungs; we were worried her ribs might give way under the pressure of a productive cough. That’s the reality of caring for this population.
Fall Prevention Is the Only Metric That Matters
If a nurse is caring for a client who has osteoporosis, their number one job is preventing a fall. Period. A fall for a healthy 20-year-old is an embarrassment; a fall for an osteoporotic senior is a life-altering, and often life-ending, event.
Statistics from the National Osteoporosis Foundation and the CDC are staggering. About 25% of seniors who suffer a hip fracture die within a year. That’s not because the bone break itself is fatal, but because of the cascade of complications: pneumonia from immobility, blood clots, and the sheer psychological toll of losing independence.
📖 Related: Why Poetry About Bipolar Disorder Hits Different
Safe environments are built, not found. A nurse has to be a bit of a detective here.
- Are there throw rugs? They have to go.
- Is the lighting dim? Crank it up.
- Is the patient wearing those "non-slip" socks that have lost their grip? Toss them.
We focus on the "Get Up and Go" test. Can the client rise from a chair, walk three meters, turn, and sit back down? If they’re shaky, we aren't just suggesting a walker; we’re documenting the necessity and training the family on its use immediately.
Medications: It’s More Than Just Calcium
Everyone thinks osteoporosis care is just about popping a few Tums or drinking milk. It’s not. While Calcium and Vitamin D are the bedrock, the pharmacological side is way more complex.
Bisphosphonates, like Alendronate (Fosamax), are the heavy hitters. But they come with a catch. If a nurse is caring for a client who has osteoporosis and they are taking an oral bisphosphonate, the morning routine is strict. The patient must sit bolt upright for at least 30 to 60 minutes after taking it with a full glass of plain water. Why? Because these drugs are incredibly corrosive to the esophagus.
Then there’s the newer stuff. Monoclonal antibodies like Denosumab (Prolia) or bone-building agents like Teriparatide (Forteo). These aren't just "pills." They require refrigeration, specific injection techniques, and a deep understanding of the patient's renal function. You can't just wing it.
The Hormone Factor
We also have to talk about estrogen. Post-menopausal women are the "face" of osteoporosis for a reason. When estrogen levels crater, bone resorption speeds up. While Hormone Replacement Therapy (HRT) isn't the go-to for everyone anymore due to cardiovascular risks, it's still a conversation a nurse needs to facilitate between the patient and the endocrinologist.
👉 See also: Why Bloodletting & Miraculous Cures Still Haunt Modern Medicine
Nutrition and the "Protein Gap"
Calcium gets all the glory, but protein is the unsung hero of the bone matrix. Bones are about 50% protein by volume. If a nurse is caring for a client who has osteoporosis and that client is malnourished, no amount of Calcium supplements will fix the problem. The "scaffold" isn't there to hold the mineral.
We look for:
- Magnesium intake: It helps with the biochemical reactions that regulate calcium.
- Vitamin K2: This is the "traffic cop" that tells calcium to go into the bones instead of the arteries.
- Weight-bearing exercise: This is "mechanical nutrition." The bone needs the stress of weight to signal the body to keep it strong. This is why we push for walking or resistance bands even when the patient is tired.
The Psychological Weight of Fragility
Living with bones that might break at any moment is terrifying. It creates "fear of falling," which leads to "activity restriction." This is a death spiral. The less a patient moves because they are scared, the weaker their muscles get. The weaker their muscles get, the more likely they are to fall.
A nurse’s role is part cheerleader, part drill sergeant. We have to validate the fear but push through it. We use "motivational interviewing." Instead of saying "You need to walk," we ask, "What is one thing you’d like to be able to do without help?" Usually, it's something simple, like getting the mail or visiting a grandchild. We use that as the leverage for physical therapy compliance.
Pain Management Without the Fog
Pain in osteoporosis usually comes from vertebral compression fractures. It’s a grinding, deep ache. The temptation is to use heavy-duty opioids, but for a nurse, that’s a red flag. Opioids cause dizziness. Dizziness causes falls.
We look for alternatives. Heat therapy, gentle TENS unit applications, or "back-sparing" mechanics. We teach the "log roll" for getting out of bed. You don't twist. You move your whole body as one unit. It sounds simple, but for someone used to hopping out of bed, it’s a total lifestyle redesign.
✨ Don't miss: What's a Good Resting Heart Rate? The Numbers Most People Get Wrong
Real-World Action Steps for Caregivers
If you are currently in the position of a nurse or a family caregiver looking after someone with this condition, the "to-do" list needs to be practical. Forget the abstract theories.
Conduct a Home Audit Immediately
Walk through the house. If you see a cord across a walkway, tape it down or move it. If the bathroom doesn't have a grab bar, get one installed this weekend. These aren't "nice-to-haves." They are life-saving equipment.
Review the Med Schedule
Check the timing of bone-building meds. If they are taking Calcium and Iron at the same time, stop. They compete for absorption. Space them out by at least two hours.
Push for a DXA Scan
If it's been more than two years since the last Dual-Energy X-ray Absorptiometry (DXA) scan, it’s time for a new one. You can't manage what you aren't measuring. We need to see if the T-score is improving or if the current treatment plan is failing.
Focus on "Core" Stability
Stronger abs and back muscles act as a natural brace for the spine. Work with a physical therapist specifically trained in osteoporosis (someone who knows not to do spinal flexion exercises like crunches, which can actually cause fractures).
Hydration and Orthostatic Hypovolemia
Make sure the client is drinking enough water. Dehydration leads to a drop in blood pressure when standing up (orthostatic hypotension). That split second of dizziness is when the hip fracture happens. Encourage them to "dangle" their feet over the side of the bed for a full minute before standing.
Nursing a client with osteoporosis is a marathon of vigilance. It requires a blend of pharmacological knowledge, environmental engineering, and deep empathy for a person who feels their own frame is failing them. The goal is never just "survival"; it's the preservation of a life worth living, free from the confinement of a hospital bed.