You’re sitting on the couch, maybe scrolling through your phone, and you feel that rhythmic thump in your chest. Or maybe your Apple Watch just buzzed with a notification that feels slightly accusatory. You look down. 72 beats per minute. Or maybe it's 58. Or 85. Naturally, you head straight to Google and pull up a heart rate resting chart to see if you’re "normal."
Most of those charts are kinda misleading.
They give you these rigid boxes—"Athlete," "Excellent," "Poor"—as if your heart is a grade school report card. But your heart doesn’t live in a vacuum. It lives in a body affected by yesterday's double espresso, that looming work deadline, and whether or not you actually slept more than five hours last night. A resting heart rate (RHR) is a snapshot, but most people treat it like a fixed identity. It isn't.
The Reality Behind the Heart Rate Resting Chart
So, what is a "normal" resting heart rate? If you ask the American Heart Association, they’ll tell you the standard range for adults is 60 to 100 beats per minute (bpm). That is a massive window. It’s like saying a normal height for a human is between four feet and seven feet. Technically true, but not exactly helpful for the individual standing in front of you.
Research, like the massive 2020 study published in PLOS ONE which analyzed data from over 92,000 individuals using wearable devices, shows that RHR is incredibly personal. The study found that while the "average" was around 65 bpm, the "normal" for individuals could vary by as much as 70 bpm. What’s healthy for a 25-year-old marathon runner is going to look like a medical emergency for a 70-year-old with minor hypertension.
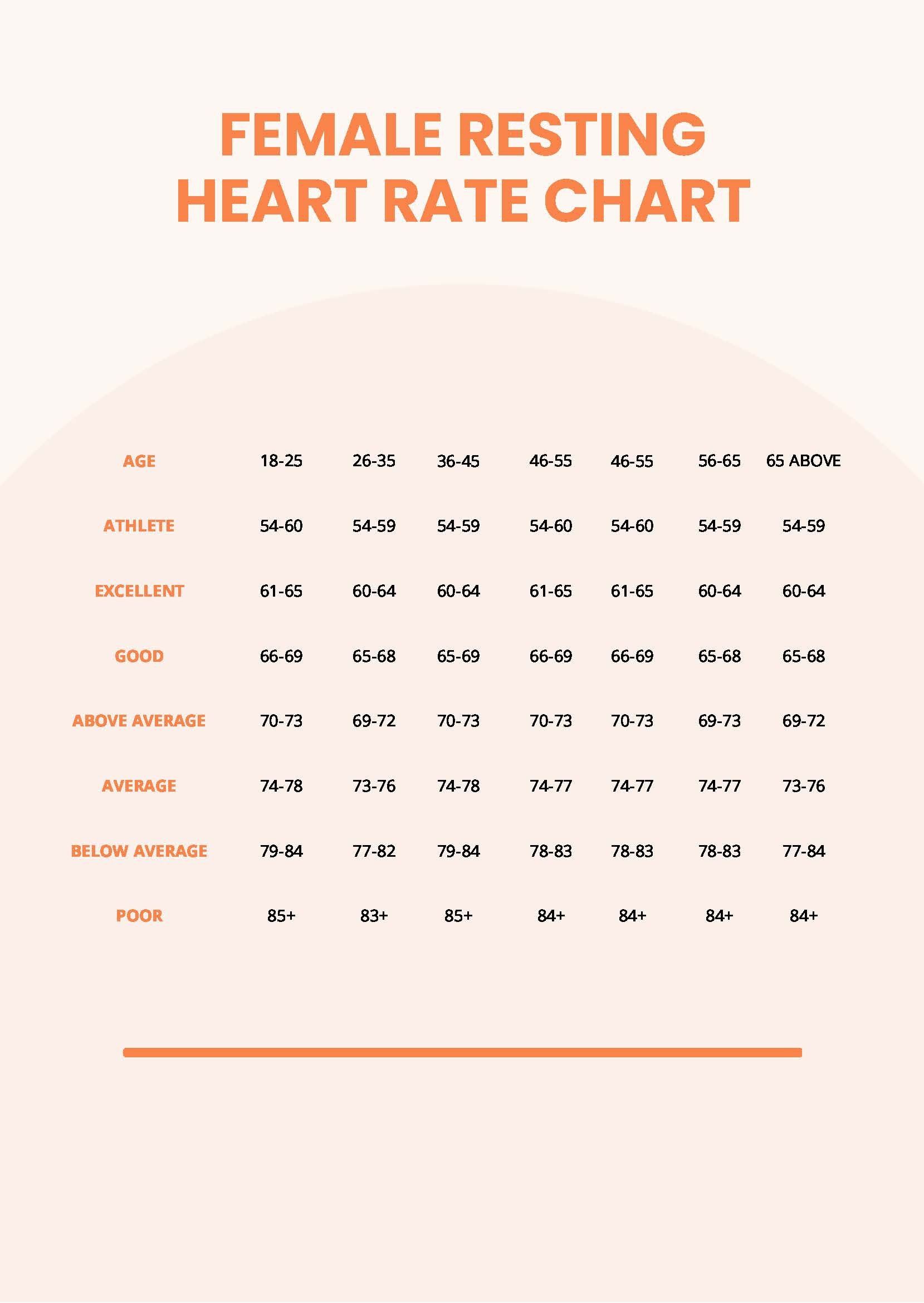
Let's look at how these charts usually break down for adults:
If you're an elite athlete, your RHR might sit comfortably in the 40s or 50s. This is because your heart muscle is so efficient—basically a high-performance engine—that it can move a huge volume of blood with a single, powerful squeeze. For the rest of us, "Excellent" is usually considered 60 to 69 bpm. If you’re in the 70 to 79 range, you’re sitting right in the "Average" or "Good" zone. Once you creep into the 80s and 90s, charts start labeling you as "Fair" or "Poor."
But here is the kicker: being in the 80s doesn't mean you're about to have a heart attack. It just means your heart is working a bit harder at rest. Maybe you’re stressed. Maybe you’re dehydrated. Or maybe that’s just where your biology naturally sits.
Why Your Numbers Change (And Why It Isn't Always Bad)
Context is everything. You can't just look at a heart rate resting chart and panic because you're ten beats off the "ideal." Your RHR is a moving target.
Take temperature, for instance. If you’re sitting in a room that’s 90 degrees, your heart rate is going to climb. Your body is trying to cool itself down by pumping more blood to the surface of your skin. It’s a cooling mechanism. Your heart is just doing its job.
Then there’s the "White Coat Effect." Honestly, many people have a higher heart rate the second they walk into a doctor’s office. The anxiety of being "checked" spikes the sympathetic nervous system. If you're measuring your RHR while sitting in a sterile exam room, you’re probably not getting a true resting reading.
💡 You might also like: Air Pollution and Causes: Why We Are Still Getting This So Wrong
The Influence of Age and Gender
Biological sex plays a role, too. Generally, women tend to have slightly higher resting heart rates than men. Why? It's mostly down to heart size. Women’s hearts are typically smaller, so they need to beat a bit more frequently to circulate the same amount of blood.
And then we have age. You’d think RHR would go up as we get older and the heart wears out, but it actually often stays stable or even decreases slightly. What does change is your maximum heart rate—the ceiling of what your heart can handle during intense exercise.
Medication and "Hidden" Factors
Beta-blockers, often prescribed for high blood pressure, will tank your heart rate. If you’re on them, you might see a 50 bpm on your watch and think you’re an Olympic cyclist. You’re not; it’s the meds. On the flip side, asthma medications or even some over-the-counter cold meds can send your RHR soaring.
Even your thyroid matters. An overactive thyroid (hyperthyroidism) can cause a racing heart, while an underactive one (hypothyroidism) can slow it down to a crawl. If your RHR has shifted significantly over a few months without a change in your fitness level, that's usually more telling than the raw number itself.
How to Get a Real Measurement
If you want to compare yourself to a heart rate resting chart, you have to do it right. Checking your pulse after walking up the stairs or while arguing on social media doesn't count.
Timing is vital. The best time to check is the absolute second you wake up, before you even get out of bed. Don't check after your first cup of coffee. Caffeine is a stimulant; it’s literally designed to kick your heart into a higher gear.
Find your pulse. Use your index and middle fingers—not your thumb, which has its own pulse—and place them on your radial artery (wrist) or carotid artery (neck).
Count for a full minute. Or count for 30 seconds and multiply by two. If you count for only 10 seconds, a single-beat error in your counting turns into a 6-beat error in your final number.
Consistency over perfection. Do this for three or four days in a row and take the average. That is your true RHR.
💡 You might also like: Why Pictures of Bug Bites to Identify Often Lie and What to Look For Instead
When Should You Actually Worry?
Numbers are just data points, but some data points deserve a phone call to a professional.
If your resting heart rate is consistently over 100 bpm—a condition called tachycardia—it’s worth investigating. It might be nothing, or it could be anemia, an infection, or a rhythm issue like SVT.
Conversely, if you aren't an athlete and your heart rate is consistently below 60 bpm (bradycardia), especially if you feel dizzy, lightheaded, or short of breath, that’s a red flag. It could mean your heart isn't pushing enough oxygen-rich blood to your brain.
But if you’re at 62 bpm and the chart says "Excellent" while you’re at 74 bpm and the chart says "Average," don't sweat it. The trend is what matters. If your RHR has been 65 for years and suddenly it’s 85 every morning, your body is trying to tell you something. Maybe you’re overtraining. Maybe you’re coming down with the flu. Maybe you’re just burned out.
Actionable Steps for Heart Health
You don't need to obsess over the heart rate resting chart, but you should care about the direction your heart health is moving.
Stop over-caffeinating. If you’re on your fourth espresso by noon, your resting heart rate isn't "resting" at all. It’s under chemical duress.
Focus on "Zone 2" cardio. To lower your RHR over time, you need to make your heart more efficient. This doesn't mean sprinting until you puke. It means long, slow movements—walking fast enough that you can still hold a conversation but you're definitely huffing a bit. This strengthens the heart's stroke volume.
Manage the "invisible" stress. Your nervous system can’t distinguish between a saber-toothed tiger and a passive-aggressive email from your boss. Both trigger the release of cortisol and adrenaline, which keep your heart rate elevated.
Hydrate like you mean it. When you’re dehydrated, your blood volume drops. To compensate, your heart has to beat faster to maintain blood pressure and move what's left of your blood around. Drinking water is literally the easiest way to "lower" a spiked heart rate.
At the end of the day, a chart is just a map of a city you don't live in. It shows you the general layout, but it doesn't know your specific streets. Use the numbers as a guide, not a gospel. Watch the trends, listen to how you feel, and remember that a healthy heart is one that can adapt to whatever life throws at it—whether that's a sprint to catch the bus or a quiet morning on the porch.