You’re sitting there, maybe nineteen or twenty years old, and suddenly the back of your jaw starts throbbing. It’s not a sharp cavity pain, but a dull, pressurized ache that feels like your skull is literally expanding. Welcome to the club. Most of us eventually have to deal with wisdom teeth, those third molars that show up late to the party and usually realize there’s no room left on the guest list.
Evolution is kinda weird like that.
Anthropologists like Dr. Noreen von Cramon-Taubadel have looked into this extensively, noting how our ancestors actually needed these beefy molars. Thousands of years ago, the human diet consisted of raw roots, tough meats, and fibrous plants that required some serious mechanical grinding. Because of that heavy lifting, prehistoric jaws were much larger and wider. But as we started cooking food and using tools, our diets softened. Over time, the human jaw shrunk. The teeth? They didn't get the memo.
What Are Wisdom Teeth and Why Do We Still Have Them?
Strictly speaking, wisdom teeth are the third set of molars located at the very back of your mouth. Most people have four—one in each corner—though it’s not unheard of for people to have fewer or even none at all. Scientists call this "hypodontia." If you're one of the lucky ones born without them, you’ve essentially fast-tracked your own evolution.
They usually pop up between the ages of 17 and 25. That’s why they’re called "wisdom" teeth; the idea is that you're supposedly wiser by the time they emerge compared to when your "6-year-old" or "12-year-old" molars came in. Honestly, the name is a bit of a participation trophy for surviving puberty.
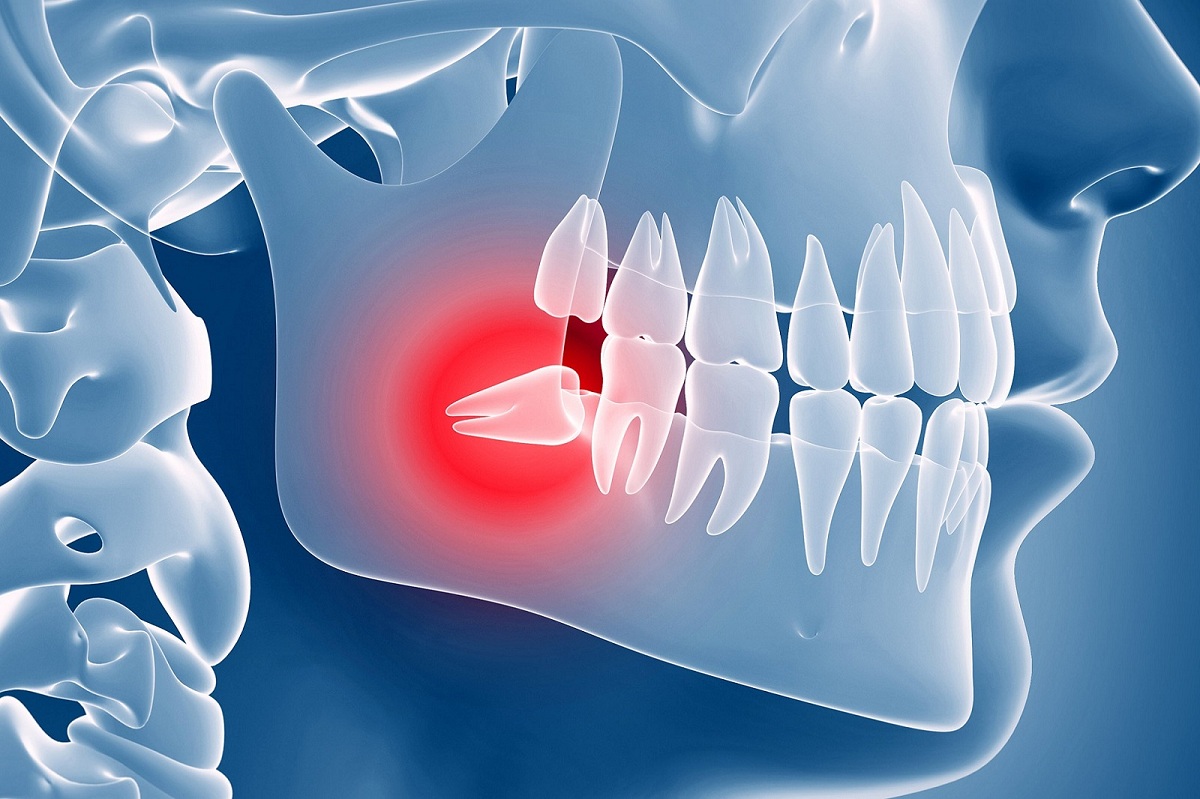
The biological mismatch here is the real issue. We have a 32-tooth blueprint crammed into a 28-tooth jaw. When these molars try to force their way in, they hit a wall—specifically, the back of your second molars. This is what dentists refer to as "impaction."
📖 Related: Why the EMS 20/20 Podcast is the Best Training You’re Not Getting in School
The Messy Reality of Impaction
Not every wisdom tooth is a disaster, but many are. When a tooth is "impacted," it means it’s stuck under the gum line or can’t fully break through because there’s literally no physical space.
It’s not just a matter of a little crowding. Sometimes a tooth decides to grow in sideways. I’m talking a full 90-degree angle, aiming straight for the roots of your healthy molars. Other times, they come in at an awkward tilt. This creates these tiny, microscopic pockets where bacteria love to hang out. You can't reach those spots with a toothbrush. You definitely can't reach them with floss. This leads to pericoronitis, which is just a fancy way of saying your gums are infected and angry because food and plaque are trapped in a "flap" of tissue.
According to the American Association of Oral and Maxillofacial Surgeons, about 85% of these teeth eventually need to come out. It’s not just a cash grab by your dentist. Leaving an impacted tooth alone can lead to cysts. In rare cases, those cysts can hollow out your jawbone or damage the nerves that give your chin and lips sensation.
Do They Always Need to Be Pulled?
There is actually a bit of a debate here. Some researchers, particularly in the UK and through organizations like NICE (National Institute for Health and Care Excellence), have argued against "prophylactic" removal—basically, taking them out "just because." They suggest that if the teeth are healthy, fully erupted, and positioned correctly, you might be able to leave them alone.
However, the "wait and see" approach has its own risks. As you get older, the bones in your mouth get denser. The roots of the wisdom teeth also grow longer and can wrap around the mandibular nerve. If you wait until you're 40 to get them pulled because they finally started hurting, the recovery is way more brutal than if you did it at 18. Younger patients heal faster. Their bone is more "plastic" and forgiving.
👉 See also: High Protein in a Blood Test: What Most People Get Wrong
If you can see the teeth, you can clean them, and they aren't pushing your other teeth into a zigzag pattern, your dentist might just keep an eye on them during your six-month cleanings. But for most of us, they’re a ticking time bomb.
The Surgery: Expectation vs. Reality
If you’re told they need to go, don’t panic. It’s one of the most common surgical procedures in the world. Usually, you'll have a choice between local anesthesia (you're awake but numb), sedation (you're "loopy" and won't remember much), or general anesthesia (completely out).
The procedure itself is often surprisingly fast. The surgeon numbs the area, makes a small incision if the tooth is under the gum, and might even break the tooth into smaller pieces to make it easier to remove.
The real work starts afterward.
Managing the Aftermath
The first 24 hours are about the "clot." This is the most important thing you’ll learn: your body creates a blood clot in the empty socket to protect the bone and nerves. If that clot gets dislodged, you end up with "dry socket" (alveolar osteitis). Ask anyone who’s had it—it’s a special kind of hell. It’s a dull, radiating pain that ear-throbs and makes you regret every life choice.
✨ Don't miss: How to take out IUD: What your doctor might not tell you about the process
- No straws. The suction can pull the clot right out.
- No smoking. Same reason, plus the chemicals mess with healing.
- No vigorous spitting. Just let the spit fall out of your mouth like a toddler. It’s ungraceful, but it works.
- Ice is your friend. 20 minutes on, 20 minutes off for the first day to keep the "chipmunk cheeks" at bay.
Common Misconceptions
People think wisdom teeth cause all their front teeth to go crooked. This is actually a point of contention in orthodontics. While the "pressure" of erupting molars can contribute to crowding, many studies, including some published in the Journal of the American Dental Association, suggest that our teeth naturally drift forward as we age anyway. Even people without wisdom teeth see their bottom front teeth get a bit crowded in their 20s.
Another myth is that if they don't hurt, they're fine. Chronic low-grade inflammation doesn't always "hurt" until it has already caused a cavity on the tooth next to it. By the time you feel the pain, you might be losing two teeth instead of just the one you didn't need.
Practical Steps Moving Forward
If you still have yours, or your teenager is starting to complain about jaw soreness, here is the roadmap.
- Get a Panoramic X-ray. A standard "bite-wing" X-ray you get at the dentist won't show the whole picture. You need the big wrap-around image that shows where the roots are in relation to your nerves.
- Monitor "Eruption Pain." A little soreness when the tooth is cutting through the gum is normal. Throbbing, foul tastes, or swelling in the neck is not.
- Clean the "Danger Zone." If yours are partially out, use an end-tuft brush. It’s a tiny brush designed for those hard-to-reach nooks.
- Consult an Oral Surgeon early. Even if you don't get the surgery yet, an expert can tell you if the roots are likely to interfere with your sinus cavity or lower jaw nerves later in life.
The reality of wisdom teeth is that they are evolutionary leftovers—the "appendix of the mouth." While some people manage to keep theirs without issue, most of us simply don't have the skeletal real estate to accommodate them. Dealing with them early is almost always better than waiting for an emergency on a holiday weekend when your dentist is closed. Keep an eye on the back of your mouth; your future self will thank you for being proactive.