Ever sat in a doctor's office staring at one of those laminated posters on the wall? You know the one. It’s got all the pluses and minuses, lines crossing everywhere like a chaotic subway map. It’s the blood type donor recipient chart, and honestly, most of us just ignore it until we’re actually sitting in a donation chair or, heaven forbid, waiting for a transfusion in a hospital bed.
It matters. A lot.
If you get the wrong blood, your body doesn’t just "not like it." It freaks out. Your immune system sees those new red blood cells as invaders—like a virus or bacteria—and starts a full-scale war. This is called an acute hemolytic transfusion reaction. It’s scary, it’s fast, and it’s why doctors are so obsessed with double-checking your Type A+ status before the bag even touches the IV pole.
The Basic Science of Who Gets What
Let's break down the "why" behind the chart. Your blood type is determined by antigens. These are basically little protein markers sitting on the surface of your red blood cells. Think of them like a specialized ID badge. If you have the A antigen, you're Type A. If you have B, you're Type B. If you have both? You're AB. If you have neither, you're the "blank slate" known as Type O.
Then there’s the Rh factor. That’s the "positive" or "negative" part. It’s another protein (the D antigen). If you have it, you're positive. If you don't, you're negative.
This creates the eight main types we see on every blood type donor recipient chart: A+, A-, B+, B-, AB+, AB-, O+, and O-.
The Universal Donor Mythos
Everyone talks about O- as the "Universal Donor." It’s true, mostly. Because O- blood lacks A, B, and Rh antigens, almost anyone can receive it without their immune system throwing a punch. Emergency rooms keep "Uncrossed O Neg" on hand for when a trauma patient is bleeding out and there’s no time to check their type.
But here’s the kicker: O- is rare. Only about 7% of the population has it.
On the flip side, we have the "Universal Recipients." That’s the AB+ crowd. If you are AB+, you are the lucky winner of the genetic lottery in terms of receiving blood. You’ve already got the A antigen, the B antigen, and the Rh factor. Your body recognizes everything. You can take a pint from literally anyone on the street and your body will just say, "Cool, thanks for the refill."
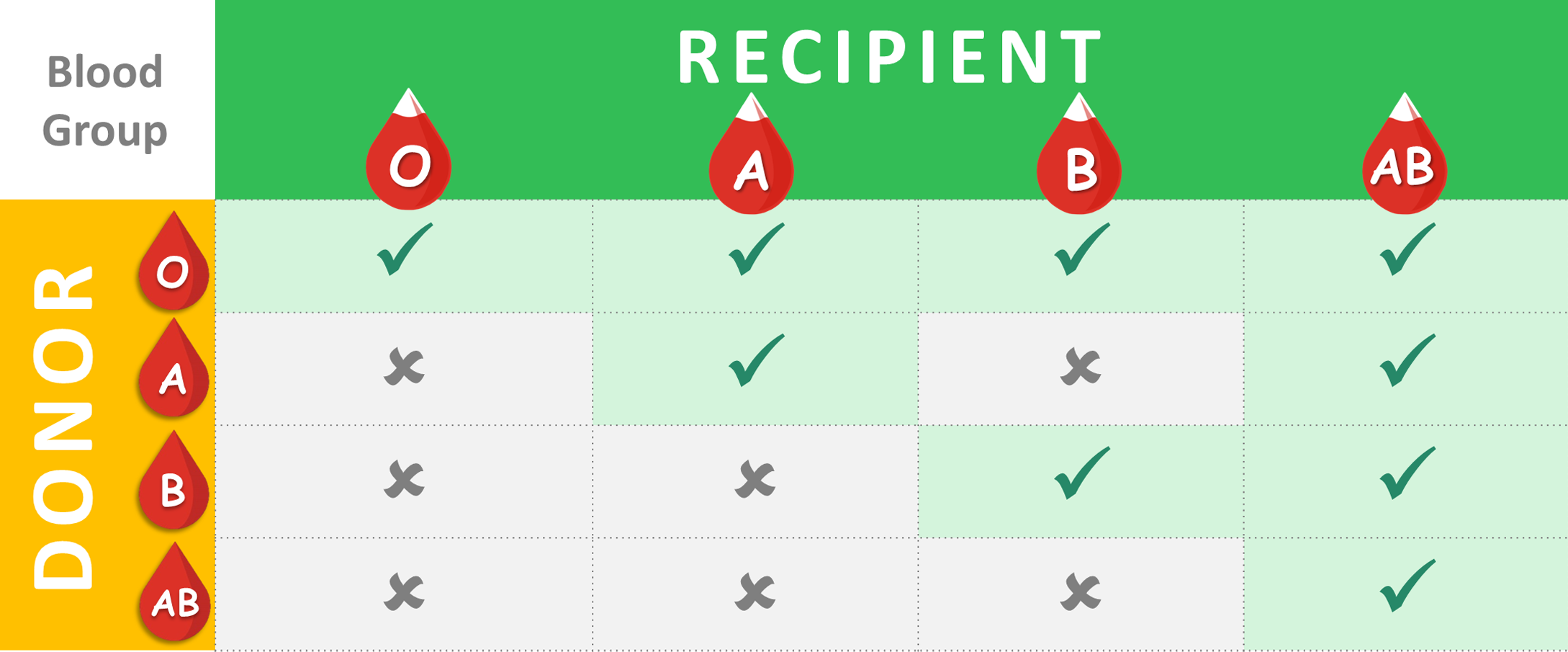
Breaking Down the Blood Type Donor Recipient Chart Relationships
Instead of a confusing grid, let's just look at how these groups actually interact in the real world.
The Type O Group
- O Positive: This is the most common blood type. About 38% of people have it. If you’re O+, you can give to any other "positive" type (A+, B+, AB+, or O+). But, you can only receive from O+ or O-.
- O Negative: The unicorn. You can give to everyone. However, you are incredibly restricted in what you can receive. You can only take O- blood. This is why O- donors are constantly hounded by the Red Cross.
The Type A Group
- A Positive: You can give to A+ and AB+. You can receive from A+, A-, O+, and O-.
- A Negative: You can give to A-, A+, AB-, and AB+. You can receive from A- and O-.
The Type B Group
- B Positive: You can give to B+ and AB+. You can receive from B+, B-, O+, and O-.
- B Negative: You can give to B-, B+, AB-, and AB+. You can receive from B- and O-.
The Type AB Group
- AB Positive: You can give only to other AB+ people. But you can receive from everyone.
- AB Negative: You can give to AB- and AB+. You can receive from all negative types (A-, B-, O-, AB-).
Why This Isn't Just Academic
In 2026, we still haven't perfected "synthetic blood." We are still entirely dependent on the kindness of strangers. According to the American Red Cross, someone in the U.S. needs blood every two seconds. Think about that. By the time you finish this paragraph, three or four people just needed a transfusion.
And it isn't just about car crashes or surgeries.
Sickle cell disease patients often require frequent transfusions throughout their lives. For these patients, the blood type donor recipient chart is just the tip of the iceberg. Doctors often have to look for "phenotype matching," which goes way beyond A, B, and O. They look for minor antigens like Kell, Duffy, and Kidd. If a patient receives blood that matches their ABO type but has a different minor antigen, they can develop antibodies that make future transfusions nearly impossible.
This is why ethnic diversity in the donor pool is so vital. Some rare blood phenotypes are found almost exclusively in specific ancestral groups.
The Plasma Twist
Here is something that usually trips people up. Everything I just said about the blood type donor recipient chart? It flips when you talk about plasma.
Plasma is the liquid part of your blood that carries the cells. It contains the antibodies against the antigens you don't have.
✨ Don't miss: Finding Knots Under Skin on Stomach: When to Worry and What’s Likely Going On
So, while O- is the universal red cell donor, AB+ is the universal plasma donor. AB plasma doesn't have any antibodies against A or B, so it can be given to anyone. In a trauma situation where a patient needs clotting factors, AB plasma is gold. If you’re AB, don’t just think about donating whole blood; your plasma is what the hospitals are screaming for.
What Most People Get Wrong
People often think blood types are static across the globe. They aren't.
In Central and South America, Type O is overwhelmingly dominant—in some indigenous populations, it’s nearly 100%. In parts of Asia, Type B is much more common than it is in Europe or the United States. This geographical shift matters for global health logistics.
Another misconception? That your blood type can change.
Barring a bone marrow transplant, your blood type is yours for life. If you get a marrow transplant from someone with a different blood type, your blood will eventually transition to the donor's type because the marrow is the "factory" where your blood cells are made. It’s one of the few ways humans can actually change their biological "ID card."
Practical Steps for You Today
Knowing your type is more than just a trivia fact. It’s part of your personal health literacy.
1. Check your records.
Most people don't actually know their type. It’s not usually on your driver's license anymore (though some people wish it was). Look at birth records, old lab results, or just ask your primary care doctor at your next physical.
2. Use the chart to plan your impact.
If you are O- or O+, your whole blood is incredibly valuable for general use. If you are AB, consider "apheresis" donation to give just your plasma or platelets. Platelets have an incredibly short shelf life—only five days—so those donations are constantly in demand for cancer patients undergoing chemotherapy.
3. Download a blood donor app.
Organizations like the Red Cross or Vitalant have apps that track your donations, tell you your blood type after your first visit, and even show you where your blood is going. There is a weirdly satisfying "ping" you get when your blood arrives at a specific hospital to save a life.
4. Understand the "Rh-Null" outlier.
While the standard blood type donor recipient chart covers 99.9% of us, there is a type called "Golden Blood" (Rh-null). It lacks all 61 possible antigens in the Rh system. There are fewer than 50 people in the entire world known to have it. If you have this, you are the ultimate donor for anyone with rare Rh types, but you can only receive Rh-null blood yourself. It's a heavy burden to carry.
Final Perspective
The blood type donor recipient chart is essentially a map of human compatibility. It shows us that, despite all our perceived differences, our survival is literally wired into our ability to share our life force with one another. Whether you’re an O- giving to a stranger or an AB+ being grateful for the wide net of safety you have, understanding these connections is fundamental to modern medicine.
Next time you see that chart, don't just see a grid. See the logic of a system designed to keep us alive when things go wrong. Go find out your type. It takes five minutes, a quick finger prick, and it might be the most important piece of data you ever learn about your own body.
Log into your patient portal or make a donation appointment this week to confirm your status. It’s better to know now than to have a doctor trying to figure it out while you’re headed into the OR.
Once you know your type, keep a digital copy of it in your phone's "Medical ID" section. This allows first responders to see your blood type even if your phone is locked. It’s a small step that significantly streamlines the process when seconds are the only currency that matters.