You’re sitting on the couch, maybe scrolling through your phone or watching a rerun of a show you've seen a dozen times, and you feel a weird tightness in your chest. It isn't a crushing weight. It doesn't feel like an elephant is sitting on you, despite what every medical drama from the last thirty years told you to expect. It’s just... off. Maybe it feels like bad heartburn from that taco you had three hours ago. You ignore it. You go to sleep.
But you might actually be in the middle of a myocardial infarction.
To have a heart attack is often a much quieter, more confusing experience than the movies suggest. We’ve been conditioned to look for the "Hollywood Heart Attack"—the dramatic gasp, the clutching of the left arm, the sudden collapse. In reality, according to the American Heart Association, many people wait hours before seeking help because their symptoms are so vague they don't think they're "sick enough" for the ER.
The Biology of the Blockage
Basically, your heart is a pump that never gets a day off. It needs a constant supply of oxygenated blood to keep the muscle tissue alive. This blood travels through the coronary arteries. Over time, stuff called plaque—a mix of fat, cholesterol, and other cellular waste—builds up on the inner walls of these pipes. Doctors call this atherosclerosis.
Think of it like old plumbing in an apartment building.
Everything is fine until a piece of that "gunk" (the plaque) ruptures. When it breaks, your body tries to fix the wound by forming a blood clot over it. If that clot is big enough, it completely plugs the artery. Within minutes, the heart muscle downstream starts to starve. It begins to die. This is the moment you have a heart attack.
🔗 Read more: Exercises to Get Big Boobs: What Actually Works and the Anatomy Most People Ignore
Research from the Mayo Clinic emphasizes that the damage isn't always instant. It’s a process. If you can get that blockage opened within the first 90 minutes—what doctors call the "Golden Window"—the chances of long-term survival and heart function recovery skyrocket. Wait six hours? The damage might be permanent.
It Doesn't Always Hurt
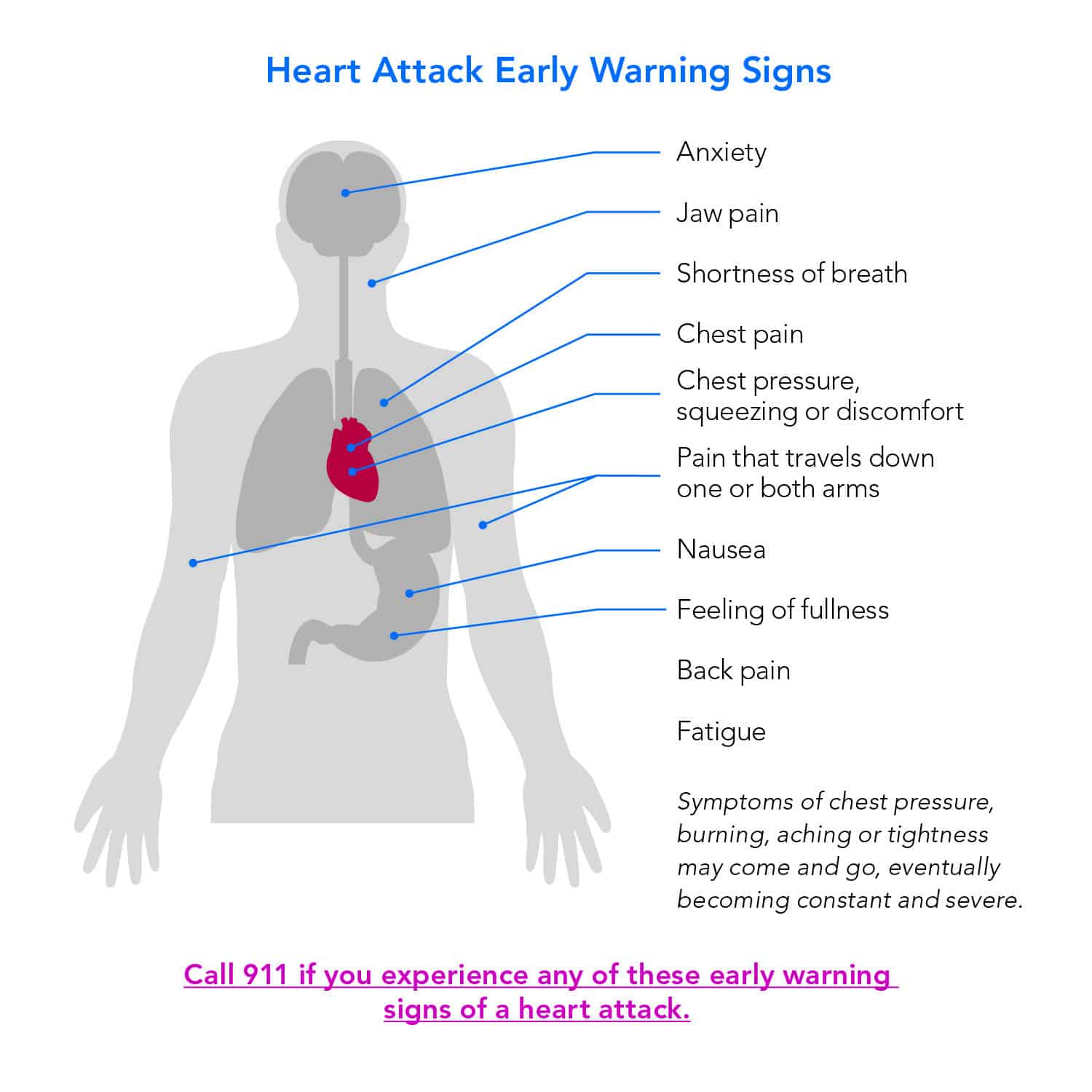
Men and women often experience this differently. It's a huge problem in emergency medicine. While men are more likely to report that classic chest pressure, women frequently show up with "atypical" symptoms.
- Extreme, unexplained fatigue that lasts for days.
- Nausea or a feeling of "heavy" indigestion.
- Pain in the jaw, neck, or upper back.
- Lightheadedness or a "sense of impending doom."
I've talked to patients who thought they just had the flu. They spent two days in bed with a cold sweat and a nagging ache in their shoulder blades, only to find out later they’d suffered a significant cardiac event. This "silent" version is particularly common in people with diabetes because nerve damage can dull the sensation of pain.
What Actually Increases the Risk?
We know the usual suspects: smoking, high blood pressure, and high LDL cholesterol. But there’s more nuance to it. For instance, chronic stress isn't just a mental health issue; it's a physical one. When you're constantly "on," your body pumps out cortisol and adrenaline. This keeps your blood pressure elevated and can trigger inflammation in your arteries.
Recent studies published in The Lancet have looked at environmental factors too. Did you know that long-term exposure to high levels of noise pollution or air pollution is now linked to higher rates of cardiac events? It’s not just about whether you eat your broccoli. It’s about the environment your heart is forced to live in every single day.
💡 You might also like: Products With Red 40: What Most People Get Wrong
Then there’s genetics. You can be a marathon runner who eats nothing but kale and still have a heart attack if your liver is genetically programmed to overproduce certain types of cholesterol, like Lipoprotein(a). Life isn't always fair.
The Immediate Action Plan
If you think it's happening, stop reading and call 911. Seriously.
Don't drive yourself. Paramedics can start treatment the second they walk through your front door. They have EKGs in the ambulance. They can transmit that data to the hospital while they’re still in your driveway. If you drive yourself and black out behind the wheel, you're not just a cardiac patient anymore; you're a car crash victim.
Chew an aspirin. Don't just swallow it. Chewing it helps it get into your bloodstream faster. Aspirin works by thinning the blood and potentially slowing down the growth of the clot that’s causing the trouble. It’s a simple 81mg or 325mg tablet that has saved more lives than almost any high-tech medical device.
Survival is Just the Beginning
Surviving the event is the first hurdle. The second is the mental toll. Many people who have a heart attack experience significant depression or anxiety afterward. It’s a trauma. Your body, the thing you trust to carry you through the world, just "failed" you.
📖 Related: Why Sometimes You Just Need a Hug: The Real Science of Physical Touch
Cardiac rehab is a literal lifesaver here. It's not just about walking on a treadmill while a nurse watches your heart rate. It’s about education. You learn how to eat, how to manage stress, and how to trust your heart again. Data shows that patients who complete a full course of cardiac rehab have a significantly lower risk of a second event compared to those who skip it.
Moving Forward With Your Health
Prevention isn't a one-time thing. It’s a series of boring, daily choices.
Check your numbers. Know your blood pressure. If it's consistently over 130/80, talk to your doctor. Don't wait for a "sign." High blood pressure is the silent killer because it usually doesn't feel like anything at all until the moment you have a heart attack.
Get a calcium score test if you're over 40 and have a family history. This is a quick CT scan that looks for actual calcified plaque in your arteries. It’s far more predictive than a simple cholesterol test. Sometimes a person with "normal" cholesterol has a shockingly high calcium score, which changes the entire treatment plan.
Move your body. You don't need to run a 5k. A 20-minute brisk walk five days a week lowers your risk of heart disease by nearly 30 percent. Your heart is a muscle; it needs the workout to stay resilient.
Lastly, pay attention to your sleep. Sleep apnea—where you stop breathing periodically during the night—puts a massive strain on the cardiovascular system. If you snore loudly or wake up feeling exhausted, get a sleep study. Fixing your breathing at night might be the single most important thing you do for your heart this year.
Monitor your body's "baseline." If you suddenly find that you're winded walking up a flight of stairs that used to be easy, don't just blame it on getting older. Get it checked. Early intervention is the difference between a minor scare and a life-altering tragedy.