You're sitting at your desk, staring at a half-finished email. Your phone pings. You check it. Ten minutes later, you’re looking at a Wikipedia page about the history of salt. You can't remember why you opened the browser. If this sounds like ADHD, you're right. But if you fell off a bike two years ago or took a nasty hit during a soccer game, it might not be ADHD at all. It might be the lingering ghost of a brain injury.
Traumatic brain injury and ADHD share a messy, overlapping Venn diagram of symptoms that drive doctors and patients absolutely bonkers.
We’re talking about the same "executive dysfunction" bucket. Memory lapses. Impulsivity. That feeling like your brain is a browser with 50 tabs open and three of them are playing music but you can't find which ones. Honestly, it’s a diagnostic nightmare.
Dr. Russell Barkley, a heavyweight in the ADHD research world, often points out that ADHD is a developmental disorder—you're basically born with the wiring. A traumatic brain injury (TBI), however, is an event. It’s a "before and after" scenario. Yet, when you're standing in the pharmacy line, the struggle feels identical.
The Secondary ADHD Phenotype
There is a specific term for this: "Secondary ADHD." It’s what happens when a person who never had focus issues suddenly develops them after a concussion or a more severe TBI.
Research published in JAMA Pediatrics has tracked kids for years after head injuries. The findings are a bit chilling. Kids with severe TBIs are nearly four times more likely to develop secondary ADHD symptoms compared to those with minor injuries. But here’s the kicker: the symptoms might not show up immediately. Sometimes, there’s a "silent period." The brain compensates for a while, then hits a wall when the academic or work demands get harder.
✨ Don't miss: Average Male Heart Rate: What Most People Get Wrong
It’s not just "being ditzy."
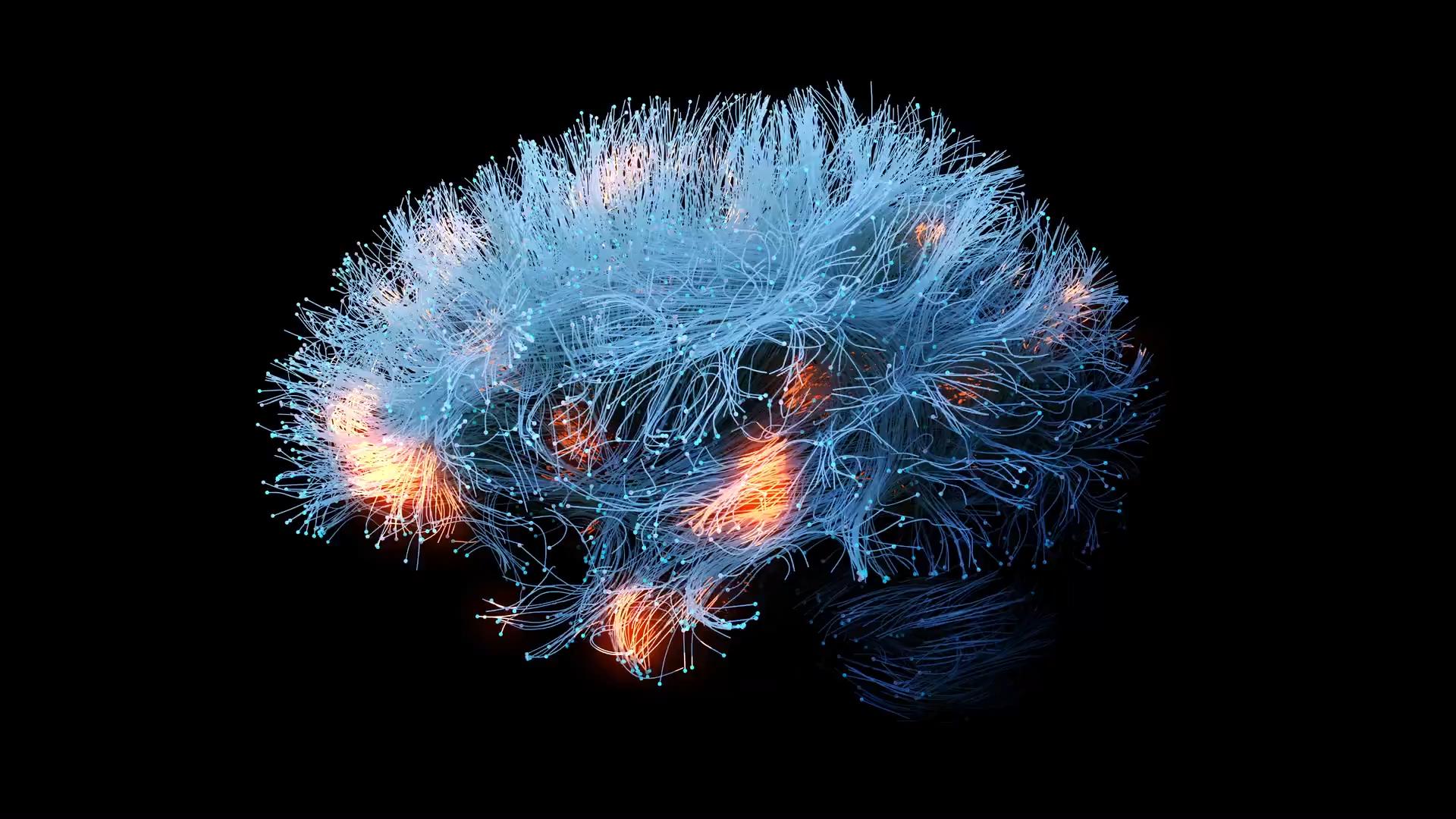
The frontal lobe is the CEO of your brain. It handles the "stop and think" part of your personality. When you experience a traumatic brain injury and ADHD symptoms follow, it’s often because the physical shearing of axons—the wires connecting your brain cells—has disrupted the CEO's office. The CEO isn't firing people; the phone lines are just down.
Why the distinction is actually a big deal
If you treat a TBI like standard ADHD, you might fail.
Standard ADHD usually responds well to stimulants like Adderall or Ritalin because the issue is primarily a dopamine signaling problem. With a TBI, the architecture of the brain is physically altered. Stimulants might help some people, but for others, they can actually increase irritability or trigger "flooding"—that feeling where every sound and light is suddenly way too loud and bright.
- TBIs often come with "neuro-fatigue." This isn't just being tired; it’s a total system shutdown after doing an hour of cognitive work.
- ADHD brains usually crave stimulation. TBI brains are often overwhelmed by it.
- The emotional "short fuse" in TBI patients is frequently more explosive than the typical emotional dysregulation seen in ADHD.
The Misdiagnosis Trap
I've talked to people who spent years on the wrong meds. One guy, let's call him Mike, was treated for ADHD for five years in his late twenties. He was struggling at his job, losing his keys, and snapping at his wife. He felt like a failure. It wasn't until a new neurologist asked, "Have you ever lost consciousness?" that the lightbulb went on.
Mike had a massive "bell-ringer" in college football. He never thought to mention it because he didn't "break" his brain. He just got a concussion.
💡 You might also like: Natural remedies for chest pain: What Most People Get Wrong
But a concussion is a TBI.
The medical community is finally moving away from the "just a concussion" language. We now know that the metabolic crisis in the brain after an impact can last much longer than the headache. If you have a pre-existing ADHD diagnosis and then get a TBI? It’s like adding gasoline to a campfire. It’s what experts call "double jeopardy." Your baseline was already shaky, and now the structural integrity is compromised.
The Dopamine Connection
Both conditions involve the prefrontal cortex and the basal ganglia. These are the parts of the brain that help you choose what to pay attention to. In a standard ADHD brain, the dopamine is being reabsorbed too quickly. In a brain with traumatic brain injury and ADHD-like traits, the receptors themselves might be damaged, or the pathways to transport that dopamine are broken.
It's the difference between a car having no gas (ADHD) and a car having a broken fuel line (TBI). You can keep trying to put gas in, but if the line is leaking, the engine still won't turn over properly.
Practical Strategies for Navigating Both
If you’re dealing with the fallout of a head injury or suspect your ADHD is actually TBI-related, you have to change the game. You can't just "hustle" your way through it.
1. The Low-Stimulation Workday
Unlike classic ADHDers who might need music or a fidget spinner to focus, TBI-impacted brains often need a "sensory diet." This means noise-canceling headphones are a non-negotiable. It means working in 20-minute chunks followed by 5 minutes of closing your eyes in a dark room. Not scrolling TikTok. Actual darkness.
2. Cognitive Rehabilitation
This isn't just "brain games" on your phone. Real cognitive rehab involves working with an occupational therapist to build external systems. If your internal hard drive is glitchy, you need a massive external hard drive.
- Use a physical paper planner (screens can be overstimulating).
- Set "deadbolt" routines—checking the stove, the locks, and the wallet in the same order every time you leave.
3. Screen Your History
If you're seeking an ADHD diagnosis as an adult, you must bring up your physical history. Did you have a car accident? Did you play contact sports? Did you have a bad fall as a toddler? A neuropsychological evaluation is the gold standard here. It’s a grueling 4-to-6-hour battery of tests that can actually distinguish between developmental ADHD and acquired brain injury by looking at specific patterns of memory and processing speed.
The Role of Inflammation
One thing people rarely talk about is the long-tail inflammation. A TBI sets off an immune response in the brain. The microglia—the brain's janitors—go into overdrive. In some people, they stay in "attack mode" long after the injury has healed. This chronic neuro-inflammation can mimic the brain fog and distractibility of ADHD for years.
This is why some people find more relief through anti-inflammatory diets or specific supplements like Omega-3s and Magnesium than they do through traditional stimulants. It’s about calming the "storm" in the brain rather than just trying to rev up the engine.
🔗 Read more: Workouts to Grow Booty: Why Your Current Glute Routine Is Probably Failing You
Actionable Steps for Recovery and Management
Stop trying to distinguish which "label" fits you perfectly and start treating the symptoms you actually have. The brain is plastic; it can reroute.
- Audit your sleep immediately. Neither an ADHD brain nor a TBI brain can function on six hours of sleep. If you have sleep apnea (common after TBI), get a CPAP. Your focus will never improve if your brain is oxygen-starved at night.
- Prioritize "Pacing." This is a TBI recovery technique. If you have a big meeting at 2 PM, you must do absolutely nothing at 1 PM. Save your cognitive "tokens" for when you need them most.
- Track your triggers. Use a simple notebook to log when your "ADHD" feels worst. Is it after looking at a screen for two hours? Is it in a loud grocery store? TBI-related focus issues are usually tied to sensory overload, whereas ADHD focus issues are tied to boredom or lack of interest.
- Consult a Neuro-Ophthalmologist. Many people with lingering TBI symptoms actually have "convergence insufficiency"—their eyes don't track together properly. This makes reading and focusing feel like a Herculean task, mimicking the avoidance behaviors of ADHD.
- Consider Vestibular Therapy. If your balance is even slightly off, your brain is using 30% of its power just to keep you upright. That leaves only 70% for your work. Fix the balance, and you "unlock" more focus.
Living with the overlap of traumatic brain injury and ADHD is exhausting. It's like navigating a world built for people with fiber-optic internet when you're running on a dial-up connection. But once you stop blaming your "lack of willpower" and start acknowledging the physical reality of your brain’s wiring, things get easier. You stop fighting the fog and start learning how to walk through it.
Verify your injury history, simplify your environment, and give your brain the literal space it needs to process the world.