You’re hunched over your phone at 2:00 AM. The screen is too bright, your skin is itching like crazy, and you’re frantically scrolling through pictures of rash on skin trying to find a match. It’s frustrating. One photo looks like a mild heat rash, while the next one—which looks identical to yours—claims it’s a rare autoimmune disorder. Honestly, self-diagnosing via Google Images is a nightmare. Most people get it wrong because skin doesn't follow a script.
Skin is the largest organ you’ve got. It reacts to everything. Stress, laundry detergent, that weird plant you brushed against in the park, or even a virus. But here’s the kicker: the same rash can look totally different on pale skin versus deep skin tones. On lighter skin, inflammation usually looks bright red or pink. On darker skin, that same "red" rash might show up as purple, grayish, or dark brown. This is why those generic medical stock photos often fail you. They don't account for the nuance of human biology.
Why your search for pictures of rash on skin is failing you
The internet is a literal dumping ground for low-quality medical images. You'll see a blurry photo of a red bump and the caption says "Eczema," but it could easily be a bug bite or a staph infection. Doctors call this "morphology." They aren't just looking at the color; they’re looking at the border, the texture, and the distribution. Is it "linear" (in a line)? Is it "annular" (ring-shaped)?
Take Pityriasis rosea, for example. It’s a common skin condition that starts with a single "herald patch." If you just look at a random photo of a scaly circle, you might think you have ringworm. You’ll go buy antifungal cream, slather it on for two weeks, and absolutely nothing will happen. Why? Because Pityriasis rosea is likely viral, not fungal. Ringworm needs an antifungal; the other just needs time. This is the danger of relying solely on a visual match without understanding the "behavior" of the rash.
The color trap in dermatology
Most medical textbooks were historically written using examples on Caucasian skin. This created a massive gap in care. If you're looking for the "classic" red ring of Lyme disease (erythema migrans) on brown skin, you might miss it because it looks more like a bruised, dusky patch.
Dr. Jenna Lester, a dermatologist at UCSF, has spent years highlighting this exact issue. She founded the Skin of Color Program to address the fact that many physicians aren't even trained to recognize common rashes on diverse skin tones. When you're searching for pictures of rash on skin, you have to be specific. Search for your specific skin tone plus the symptoms. It’s a game changer for accuracy.
📖 Related: Why Poetry About Bipolar Disorder Hits Different
Identifying the "Big Three" common culprits
Usually, when someone is digging through image galleries, they’re dealing with one of three things: Eczema, Psoriasis, or Contact Dermatitis.
Eczema (Atopic Dermatitis) is the "itch that rashes." It’s not just a rash; it’s a barrier problem. Your skin is "leaky." It loses moisture and lets irritants in. In pictures, it often looks like dry, thickened, or scaly patches. In babies, it’s usually on the cheeks. In adults, it hides in the crooks of elbows and behind knees. It’s rarely just one bump. It’s a neighborhood of irritation.
Psoriasis is a different beast. This is an immune system overreaction that speeds up cell turnover. Instead of skin cells shedding every month, they pile up in days. This creates "plaques." These are thick, silvery scales that feel "stuck" to the skin. If you peel one off, it might bleed—a specific sign doctors call the Auspitz sign. You won't find that in a blurry JPEG.
Contact Dermatitis is basically your skin saying, "I hate this." It could be the nickel in your belt buckle or the fragrance in your new soap. It shows up exactly where the "offender" touched you. If you have a rash in a perfect circle around your wrist, it's probably your watch strap, not a mysterious disease.
When "Red Bumps" mean something else
Sometimes it isn't a "rash" in the traditional sense. Heat rash (miliaria) happens when sweat ducts get plugged. It looks like tiny clear bubbles or red pinpricks. It’s common in humid weather. Then there’s Shingles. Shingles is distinctive because it follows a nerve path. It won't cross the midline of your body. If you have a painful, blistering rash that stays on only the left side of your ribcage, stop looking at pictures and go to the doctor. That’s a hallmark sign.
👉 See also: Why Bloodletting & Miraculous Cures Still Haunt Modern Medicine
The problem with AI and "Doctor Google"
We’re seeing a surge in AI-powered skin scanners. You take a photo, and the app tells you what it is. It sounds cool. In reality, a 2020 study published in The Lancet Digital Health found that these algorithms often struggle with rare conditions and darker skin tones. They are only as good as the data they were fed. If the AI was trained on 10,000 photos of white people with sunburns, it's going to be pretty useless for a Black man with sarcoidosis.
Also, photos are 2D. Rashes are 3D. A dermatologist uses a tool called a dermatoscope. It’s basically a fancy magnifying glass with a polarized light that lets them see under the top layer of skin. Your iPhone camera can't do that. It can't feel the "induration" (hardness) of a lesion. It can't see the "wickham striae" (tiny white lines) that suggest Lichen Planus.
Real-world example: The "Maskne" craze
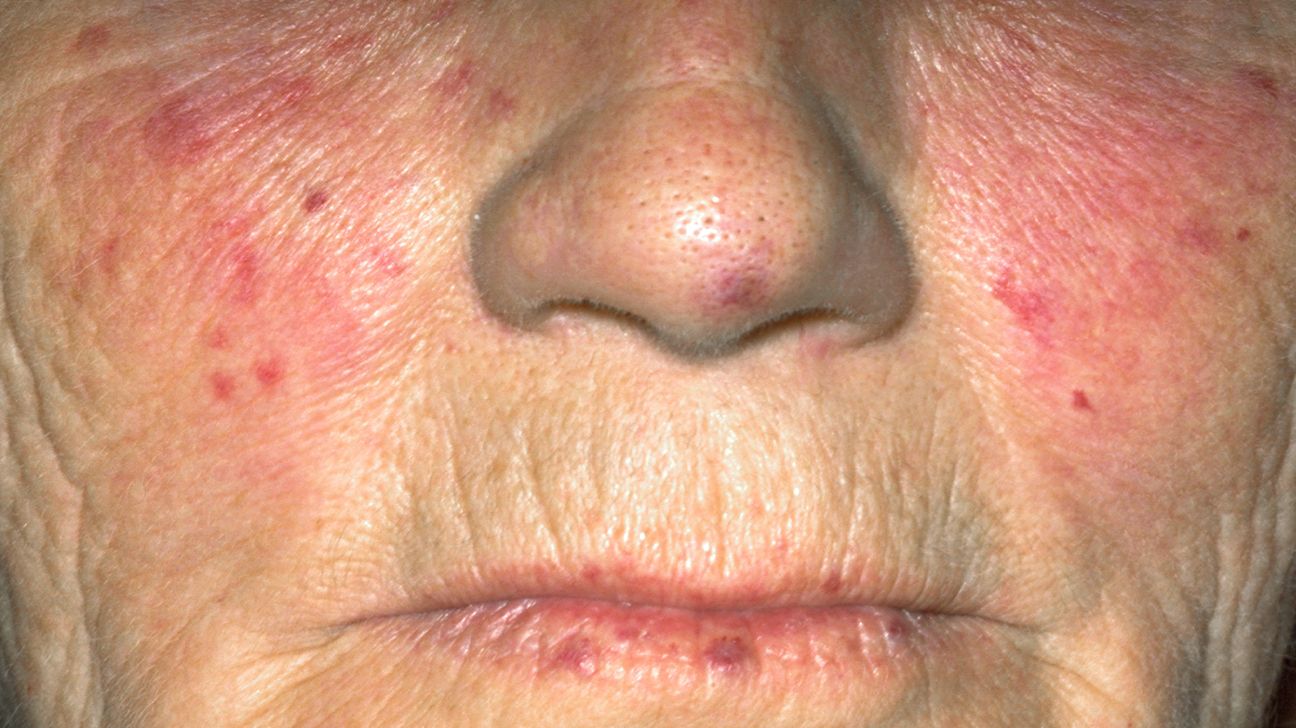
A few years ago, everyone was searching for pictures of rash on skin around the mouth. Most people thought they had acne from wearing masks. They used harsh salicylic acid and made it ten times worse. Why? Because many of them actually had Perioral Dermatitis. It looks like acne—red bumps, some pus—but it’s actually a form of rosacea/dermatitis. Using acne meds on it is like putting gasoline on a fire. This is why context matters more than a visual match.
How to actually document your skin for a pro
If you're going to use your phone, stop just "looking." Start documenting. Doctors love data, not just "it's itchy."
- Take photos in natural light. Avoid the yellow bathroom light or the harsh camera flash. Go stand by a window.
- Use a "Reference Object." Put a coin or a ruler next to the rash. This helps the doctor see exactly how big it is.
- The "Spread Test." Take a wide shot of the whole limb, then a close-up. Seeing the "pattern" (is it symmetrical?) is a huge clue.
- Track the "Trigger." Did you eat strawberries? Change your laundry pods? Use a new "all-natural" serum? (By the way, "natural" doesn't mean "safe." Poison ivy is natural.)
Serious red flags (Stop scrolling, call a doctor)
There are times when pictures of rash on skin are a waste of time because you need an ER.
✨ Don't miss: What's a Good Resting Heart Rate? The Numbers Most People Get Wrong
- The Glass Test: If you press a clear glass against a purple or red rash and it doesn't fade (blanch), that's a medical emergency. It could be petechiae or purpura, which can indicate serious blood or ceiling-level infections like meningitis.
- Fever and Malaise: If you have a rash plus a high fever, your body is fighting something systemic.
- Blisters in the mouth or eyes: This can indicate Stevens-Johnson Syndrome (SJS), a severe reaction to medication. It's rare, but it's life-threatening.
- Rapid Spreading: If it's moving across your body while you watch it, get help.
Navigating the treatment maze
Once you've identified that your "rash" is likely something specific, don't just grab a random cream. Hydrocortisone is the "duct tape" of dermatology, but it's dangerous if used incorrectly. If you put a steroid (like hydrocortisone) on a fungal infection (like ringworm), it will actually feed the fungus. It makes the rash look better temporarily by reducing inflammation, but the fungus grows deeper. This is called "Tinea Incognito." It makes the eventual cure much harder.
Similarly, "natural" remedies like tea tree oil or apple cider vinegar are incredibly caustic. People often end up with a chemical burn on top of their original rash. Honestly, the best first step for a mystery itch is a bland emollient. Something like Vaseline or a fragrance-free cream like CeraVe. It protects the barrier without adding more "reactive" chemicals to the mix.
Actionable insights for your skin health
Instead of getting lost in a rabbit hole of terrifying medical images, take these concrete steps to actually solve the problem.
- Check your "Distribution": Is the rash only on sun-exposed areas? It might be photosensitivity or a "sun allergy." Is it only under your jewelry? It's likely a nickel allergy.
- The "Symmetry" Rule: Most internal issues (like a drug reaction or a virus) show up symmetrically on both sides of the body. If it's only on one arm, it's likely something you touched.
- Consult a Telederm: If you can't get to a clinic, dermatology is one of the best-suited fields for telemedicine. High-res photos sent to a board-certified dermatologist are 100x more valuable than a Google search.
- Stop Scrubbing: Whatever you do, don't try to "wash off" the rash. Most rashes are an inflammatory response, not "dirt." Scrubbing just breaks the skin barrier and invites a secondary staph infection.
- Use "Skin of Color" Resources: If you have non-white skin, use databases like VisualDx or the Skin of Color Society image galleries. They provide much more accurate representations of how diseases manifest on various melanin levels.
Skin issues are a puzzle. A photo is just one piece. The real answer lies in the combination of what it looks like, how it feels, and what your body was doing when it started. Stop panicking over the worst-case scenarios you see online; most skin issues are annoying but highly treatable once you stop guessing and start assessing.
Key Next Steps
- Sanitize your routine: Switch to a soap-free cleanser and a fragrance-free moisturizer for 7 days to see if the "rash" calms down.
- Perform a "Blanch Test": Press your finger firmly on the rash. If it turns white and then goes back to red, it's usually less urgent than a rash that stays dark red when pressed.
- Document the "Migration": Draw a circle around the edge of the rash with a ballpoint pen. If the redness moves outside that circle within 24 hours, you have an active "spreading" issue that needs a professional look.