If you’ve spent any time Googling pictures of atopic dermatitis in adults, you’ve probably seen the same three or four images. Red, angry-looking elbows. A child’s weeping cheeks. Maybe a close-up of a crusty hand. But here’s the thing—eczema in adulthood is a shape-shifter. It doesn't always play by the rules we see in textbooks. Honestly, it’s frustrating. You might be staring at a patch of skin on your ankle that looks more like a leathery lizard scale than a "rash," and the internet tells you that’s not what atopic dermatitis (AD) is supposed to look like. It is.
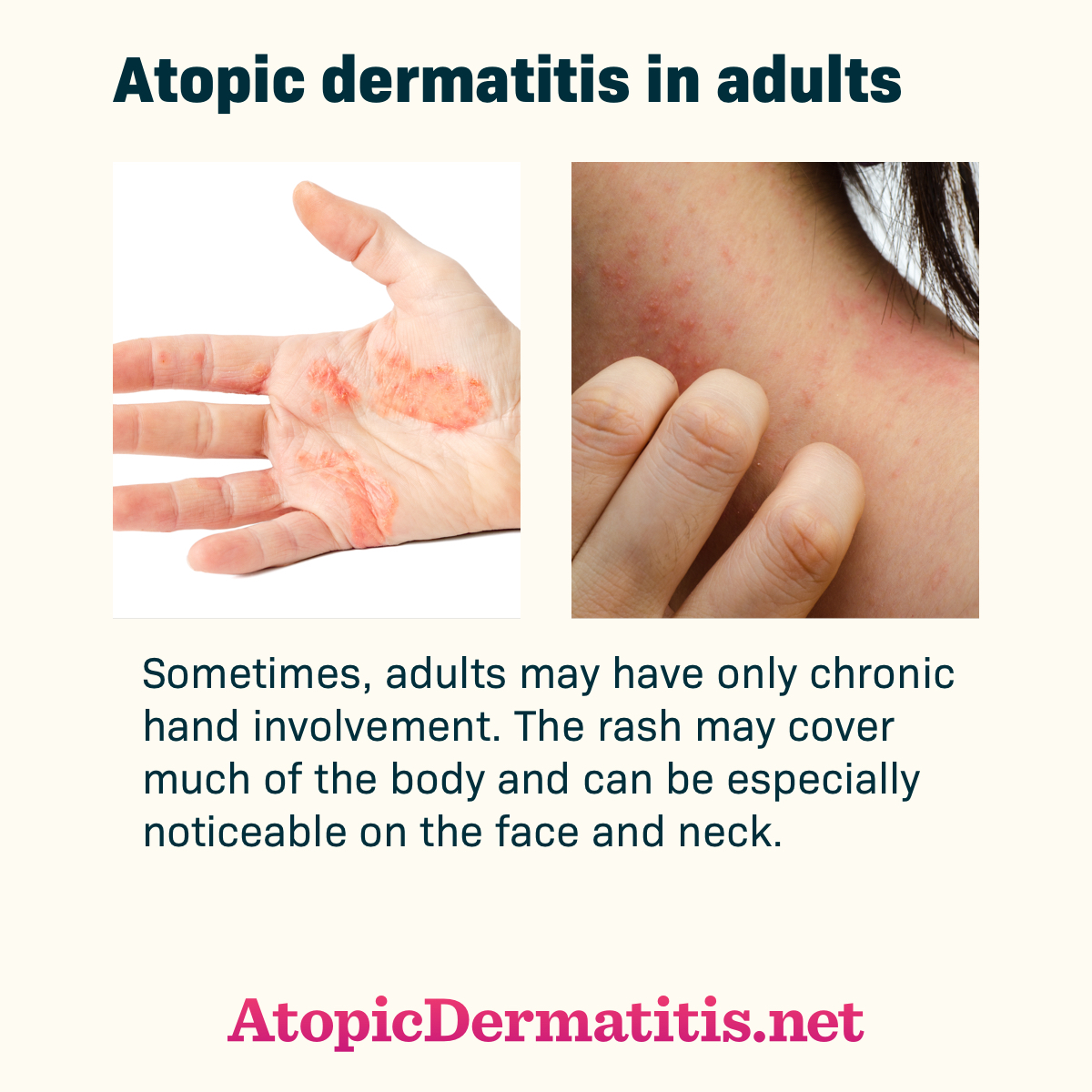
Adult AD is a different beast than the childhood version. While kids usually get it in the "crooks and nooks"—the elbows and behind the knees—adults often find it surfacing on their eyelids, their hands, or even their nipples. It’s localized, stubborn, and sometimes looks like nothing more than chronically dry skin until it suddenly flares into a burning, stinging mess.
The Visual Reality of "The Itch That Rashes"
Most people think the rash comes first. You see a red spot, then you itch it. With atopic dermatitis, it’s actually the opposite. Dr. Jonathan Silverberg, a prominent dermatologist at George Washington University, often highlights that AD is "the itch that rashes." You feel a deep, bone-deep tickle or burn. You scratch. Then the visual evidence appears.
In adults, this often manifests as lichenification. That's a fancy medical term for skin that has become thick and leathery because of constant rubbing. If you look at pictures of atopic dermatitis in adults who have lived with it for decades, you’ll notice the skin lines are exaggerated. It looks like a topographical map. It’s not just "redness"; it’s a structural change in the epidermis.
The color isn't a constant either. On lighter skin tones, yes, it’s pink or bright red. But on skin of color, AD often looks purple, grayish, or even dark brown. This leads to massive underdiagnosis. If a doctor is only looking for "redness" and doesn't see it, they might dismiss a severe case of atopic dermatitis as simple hyperpigmentation or a fungal infection. It’s a huge gap in medical training that’s only recently being addressed with more diverse clinical databases.
Eyelids and Hands: The Adult Hotspots
Adults are way more likely to have "hand dermatitis" than children. It makes sense. We wash our dishes, we use harsh cleaning chemicals, and we deal with occupational triggers. A "flare" here might not look like a rash at all; it might look like deep, painful cracks (fissures) on the fingertips that bleed when you try to pick up a coin.
Then there are the eyelids. Eyelid dermatitis is a nightmare. The skin there is the thinnest on your entire body. When AD hits the eyes, it looks like premature aging—lots of fine lines, swelling, and a sort of "crepey" texture. It’s often mistaken for an allergy to makeup, but frequently, it’s just the systemic immune response of atopic dermatitis picking the most sensitive spot to boil over.
👉 See also: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
Why Your "Rash" Might Look Different Today
Atopic dermatitis isn't a static image. It’s a movie. It has phases.
The acute phase is what most people recognize. This is the "weeping" stage. The skin is blistered, red, and literally leaks fluid (serum). It’s messy. If you see pictures of atopic dermatitis in adults where the skin looks "wet," that’s an acute flare. It's often at high risk for a Staph infection because the skin barrier is completely compromised.
Then there’s the subacute phase. The weeping stops. The skin becomes flaky and scaly. It feels tight.
Finally, you have the chronic phase. This is the leathery, thickened state mentioned earlier. An adult can have all three phases happening on different parts of their body at the same time. You might have a weeping patch on your neck and a leathery patch on your wrist. It’s exhausting to manage because what works for the "wet" rash might irritate the "dry" leathery one.
Misdiagnosis: When It’s Not Actually Atopic Dermatitis
Just because it looks like the pictures doesn't mean it is. One of the most common "look-alikes" is psoriasis. Even experts sometimes struggle to tell them apart without a biopsy.
- Psoriasis usually has very well-defined borders. It’s like a continent on a map.
- Atopic dermatitis is more "fuzzy." It fades into the surrounding skin.
- Psoriasis scales are typically silvery-white (micaceous). AD scales are usually more yellowish or clear.
Another one is nummular eczema. These are coin-shaped spots. They look exactly like ringworm. I can't tell you how many people spend weeks putting antifungal cream on a "ringworm" spot only for it to do nothing because it was actually a localized flare of atopic dermatitis. If it doesn't clear up with an over-the-counter antifungal, stop using it. You’re likely just drying out an already thirsty patch of skin.
✨ Don't miss: That Time a Doctor With Measles Treating Kids Sparked a Massive Health Crisis
The Role of the Microbiome (It’s Not Just "Dry Skin")
We used to think AD was just a "leaky" skin barrier. You lose water (Transepidermal Water Loss, or TEWL), the skin gets dry, it cracks. Simple. But new research into the skin's microbiome shows it’s way more complex.
About 90% of adults with atopic dermatitis have Staphylococcus aureus bacteria colonizing their skin, compared to only about 5% of people without the condition. This bacteria isn't necessarily causing an "infection" in the traditional sense, but it’s sending signals to your immune system to stay in a state of high alert. This is why some pictures of atopic dermatitis in adults look slightly "golden" or have a yellowish crust—that’s often the Staph talking.
Beyond the Surface: The Emotional Toll of the Visual
Let’s be real for a second. Living with visible AD as an adult is a mental health tax. When your face is flaring, or your hands look like you’ve been working in a briar patch, people notice. They ask if you’re "burned" or if it’s "contagious." It isn't, but the stigma is real.
Studies, like those published in the British Journal of Dermatology, have shown a direct correlation between the severity of the visual rash and the risk of anxiety and depression. It’s not just "vanity." It’s a systemic inflammatory condition that affects your sleep (due to the itch) and your social confidence. When you look at pictures of atopic dermatitis in adults, you aren't just seeing a skin condition; you’re seeing a person who likely hasn't had a full night’s sleep in a week.
Actionable Steps for Management
If you’re looking at your skin and it matches these descriptions, stop the DIY "hacks." Vinegar soaks or "drying out" the rash usually backfires. Hard.
The "Soak and Smear" Technique
This is the gold standard. Take a lukewarm bath (not hot!) for 10 minutes. Pat dry very gently—don't rub. While the skin is still slightly damp, apply your medicated cream (steroid or calcineurin inhibitor) and then immediately "seal" it with a thick, plain ointment like Vaseline or Aquaphor. This traps the moisture and the medicine in the skin.
🔗 Read more: Dr. Sharon Vila Wright: What You Should Know About the Houston OB-GYN
Identify Your "Hidden" Triggers
Adults often have triggers that kids don't.
- Stress: Cortisol spikes can trigger a flare within hours.
- Fragrance: It’s in everything. Laundry detergent, dryer sheets, that "natural" essential oil soap. Switch to "fragrance-free" (not just "unscented," which can contain masking fragrances).
- Nickel: High-nickel foods (like chocolate or soy) or jewelry can exacerbate AD in some adults.
Modern Treatments are Different Now
We aren't just stuck with steroid creams anymore. If you see pictures of severe atopic dermatitis in adults, know that many of those people are now finding relief with biologics like Dupixent (dupilumab) or JAK inhibitors. These target the specific "cytokines" (the signaling proteins) in the immune system that cause the itch and inflammation, rather than just nuking the whole immune system with prednisone.
Summary of Realities
Atopic dermatitis in adults is a chronic, relapsing condition. It’s not a lack of hygiene. It’s not just "dry skin." It’s an overactive immune system showing up on your largest organ.
If your skin looks like the descriptions here—thick, leathery, intensely itchy, or weeping—the most important move is to see a dermatologist who specializes in AD. They can help you distinguish between a simple allergy and a chronic systemic condition.
What to do next:
- Audit your shower: Switch to a non-soap cleanser. Anything that "lathers" too much is probably stripping your lipids.
- Check your nails: Keep them short. You will scratch in your sleep. Shorter nails do less damage.
- Document your flares: Take your own "pictures of atopic dermatitis" over a month. Note what you ate, the weather, and your stress levels. It helps your doctor more than a single snapshot ever could.
- Cotton is king: Swap synthetic fabrics for 100% cotton or silk. Your skin needs to breathe, and heat is a major itch trigger.
Stop waiting for it to "clear up on its own." Adult atopic dermatitis usually needs a proactive, multi-pronged strategy to get under control. Once you manage the inflammation from the inside out, those "topographical map" lines on your skin can actually start to soften and fade. You aren't stuck with the "lizard skin" forever.