Ever wonder why a drug that works perfectly on a lab mouse fails miserably when it hits human clinical trials? It happens more than you’d think. Honestly, it's one of the biggest bottlenecks in modern medicine. For decades, we’ve relied on animal models as the "gold standard," but let’s be real: humans aren’t 70-kilogram rats. This massive gap in biological accuracy is exactly why NIH human-based research technologies are suddenly the hottest topic in the halls of the National Institutes of Health.
It’s about New Approach Methodologies, or NAMs.
These aren't just fancy computer simulations. We are talking about living, breathing (sort of) human tissue engineered in a lab. The goal is simple but incredibly difficult. Scientists want to mimic human physiology so closely that we can predict a drug’s side effects before a single person ever swallows a pill.
The End of the "Mouse Model" Monopoly?
Don't get me wrong, animal research has saved countless lives. But the failure rate in drug development is staggering—nearly 90% of drugs that pass animal tests fail in humans. That’s a lot of wasted time and billions of dollars down the drain. Because of this, the NIH has been pivoting. Hard.
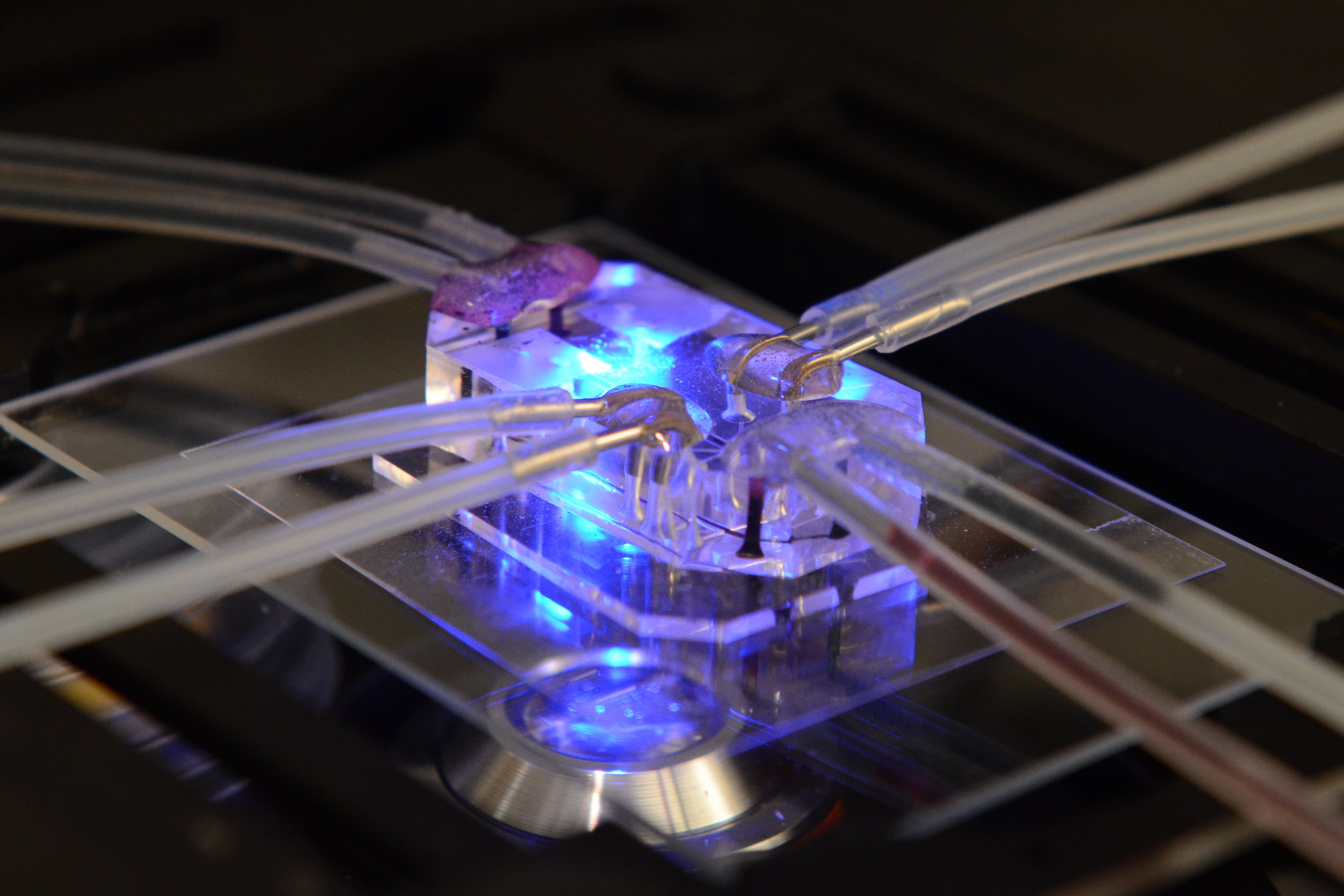
They’ve funneled massive amounts of funding into the National Center for Advancing Translational Sciences (NCATS). This is where the magic happens. They are looking at things like Organs-on-Chips. Imagine a translucent slide, about the size of a USB stick, lined with living human cells. These chips have microfluidic channels that mimic blood flow and mechanical tension. If you want to see how a new lung medication works, you use a Lung-on-a-Chip that actually "breathes" by expanding and contracting.
It's wild.
Dr. Francis Collins, the former NIH Director, was a huge proponent of this. He often spoke about how these chips could eventually replace many forms of animal testing. It’s not just an animal welfare issue; it’s a data issue. Human chips give human data.
High-Tech Tools You’ve Probably Never Heard Of
While chips get all the glory, there’s a whole suite of NIH human-based research technologies that are quietly revolutionizing the lab.
👉 See also: What Does DM Mean in a Cough Syrup: The Truth About Dextromethorphan
Take organoids. These are tiny, 3D clusters of cells grown from human stem cells. They aren't "mini-organs" in the sense that they could be transplanted, but they possess the same genetic blueprint and structural organization as a full-sized human organ. If you’re studying microcephaly or Alzheimer’s, you can grow a "brain organoid." Researchers like Dr. Alysson Muotri at UCSD have used these to study how the Zika virus attacks human neural cells—something you just can't see the same way in a rodent.
Then there’s in silico modeling. Basically, high-level math.
We’re getting better at using "virtual humans." These are complex algorithms fed by decades of clinical data. The NIH’s Big Data to Knowledge (BD2K) initiative was a precursor to this, pushing the boundaries of how we use computer power to simulate drug interactions. It's about predicting toxicity. If the computer says a compound will fry a human liver, why bother testing it on a mouse?
Why This Shift Matters for Your Health
You might be thinking, "Cool science, but how does this help me?"
Well, think about personalized medicine. Usually, doctors prescribe a drug based on what works for the "average" person. But nobody is average. We all have different genetics. With NIH human-based research technologies, specifically induced pluripotent stem cells (iPSCs), scientists can take a bit of your skin or blood, turn those cells into stem cells, and then grow your heart cells on a chip.
They can test five different blood pressure meds on your cells to see which one works best before you ever take a dose. No more trial and error. No more "let's see if this gives you a rash and check back in a month." It's medicine tailored to your actual DNA.
The Big Hurdles: It’s Not All Smooth Sailing
It would be dishonest to say this is all perfect. It’s not. Not yet.
✨ Don't miss: Creatine Explained: What Most People Get Wrong About the World's Most Popular Supplement
The biggest challenge is complexity. A Liver-on-a-Chip is great, but your liver doesn’t live in a vacuum. It talks to your gut. It talks to your brain. It filters your blood. Creating a "Body-on-a-Chip"—where multiple organ systems are linked together—is the "Holy Grail" of the NIH’s Common Fund programs. They're working on it, but the plumbing is a nightmare. Keeping different cell types alive in a shared fluid system is like trying to keep a tropical fish and a desert lizard in the same tank.
There’s also the regulatory side. The FDA has been the gatekeeper for decades. Until recently, the law basically required animal testing for drug approval. However, the FDA Modernization Act 2.0, signed into law in late 2022, changed the game. It officially allows the FDA to consider data from these human-based technologies instead of animal trials. That was a massive win for proponents of these technologies.
The Money Trail
If you want to see where the NIH is headed, look at the budget. The HEAL Initiative (Helping to End Addiction Long-term) uses these human-based models to find non-addictive pain killers. They are using human sensory neurons on chips to see how pain signals move. This is way more accurate than watching a mouse flick its tail.
The NIH also pours money into the Tissue Chip for Drug Screening program. They’ve partnered with NASA—yes, the space people—to send these chips to the International Space Station. Why? Because human cells age faster in microgravity. It’s a shortcut to studying aging and bone loss that would take years on Earth.
Real Talk: Is This the End of Animal Testing?
Probably not. At least not tomorrow.
Scientists like Dr. Margaret Hamburg, former FDA Commissioner, have pointed out that while these technologies are incredible, they can’t yet replicate the full immune response or the complex endocrine system of a living being. We still need to see how a drug affects the "whole" organism. But the trend is clear. We are moving away from the "all-animal" model and toward a "human-first" approach.
The focus of NIH human-based research technologies is to reduce, refine, and eventually replace. It’s a slow transition, but it’s happening.
🔗 Read more: Blackhead Removal Tools: What You’re Probably Doing Wrong and How to Fix It
What You Can Do With This Information
If you’re a student, a patient, or just someone who likes knowing how their tax dollars are spent, here’s how to stay ahead of the curve:
Check the Clinical Trials
When you look at new treatments, especially for rare diseases or cancers, look for "patient-derived" models. If a company is using organoids to screen their drugs, they are likely using more modern, accurate data.
Follow the NCATS Feed
The National Center for Advancing Translational Sciences is the hub for this stuff. They post updates on tissue chip breakthroughs and new funding for "human-on-a-chip" projects. It’s the best place to see what’s actually hitting the market next.
Understand the "NAMs" Acronym
If you’re reading medical news, look for the term New Approach Methodologies. This is the official umbrella term for these technologies. When a drug company says they are using NAMs, it means they are trying to bypass the traditional, often flawed, animal-only route.
Support Open Data Initiatives
One of the NIH’s biggest pushes is for "Open Science." These human models generate mountains of data. Supporting policies that require researchers to share this data means we find cures faster. The "Human Cell Atlas" is a great example of a global project the NIH supports that acts as a Google Maps for the human body.
The shift toward NIH human-based research technologies isn't just about being "nicer" to animals. It’s about being smarter about human biology. We are finally building tools that reflect the complexity of our own bodies, and that is a massive win for everyone.
Actionable Steps for Navigating the Future of Medicine
- Educate yourself on the FDA Modernization Act 2.0: Knowing that animal testing is no longer the sole legal requirement helps you understand why biotech startups are pivoting to "human-on-a-chip" tech.
- Look for "In Vitro" and "In Silico" in research papers: If you are researching a specific condition on PubMed, these terms will lead you to the most cutting-edge human-based studies.
- Ask your doctor about "Personalized Screening": While still early, some specialized clinics are starting to use human-derived cells for oncology treatments to see which chemotherapy works best for a specific patient's tumor.
- Monitor the NIH "Common Fund" website: This is where the big-ticket, high-risk/high-reward technologies get their start. It’s a preview of medicine 10 years from now.
The move toward human-centric research is a fundamental shift in the scientific method. By prioritizing human biology through chips, organoids, and advanced AI, the NIH is ensuring that the next generation of medicines is safer, cheaper, and—most importantly—actually works for us.