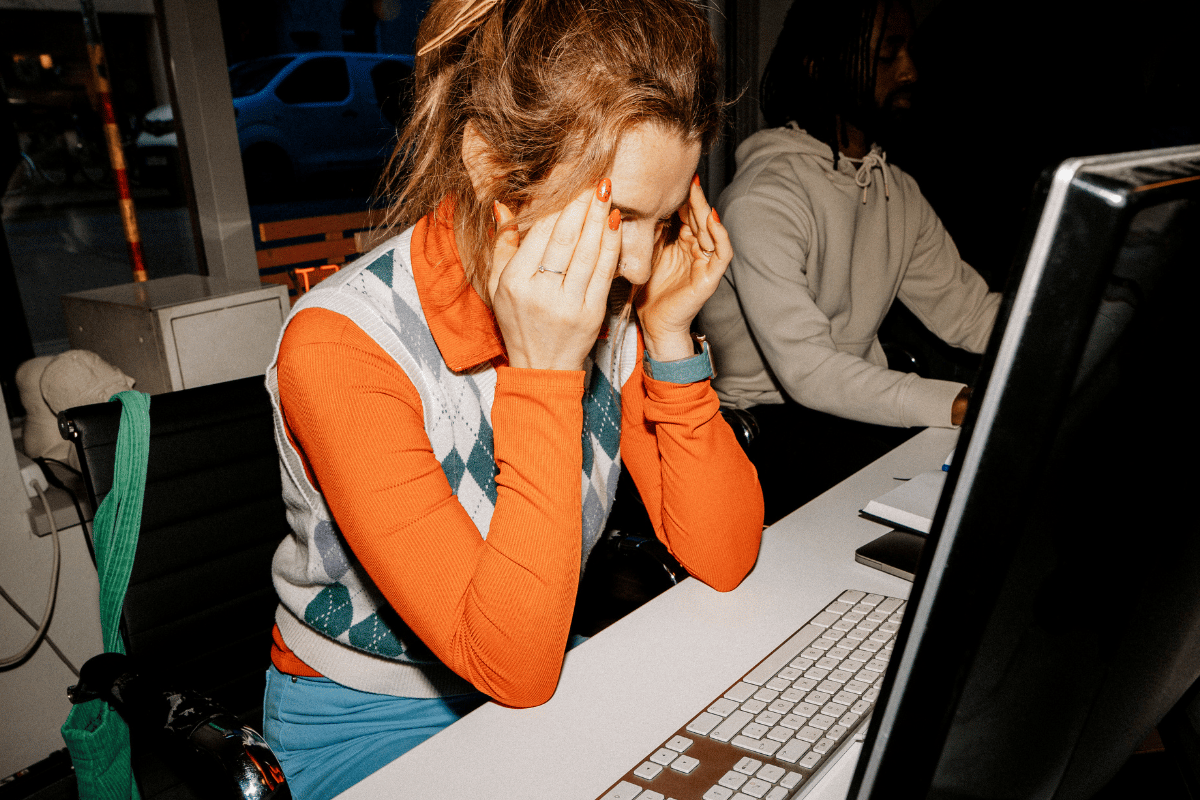
You’re tired. Not just "stayed up too late watching Netflix" tired, but a heavy, bone-deep exhaustion that doesn't go away after an extra-large latte or a ten-hour Sunday snooze. You might blame your job. Or your kids. Or the fact that you’re just getting older. But honestly, it’s often something much more mechanical happening inside your veins. When we talk about symptoms of low iron, people usually think of a pale Victorian waif fainting onto a sofa. In reality, it’s much crunchier and weirder than that.
Iron is the primary engine behind hemoglobin. Hemoglobin is the protein in your red blood cells that carries oxygen from your lungs to the rest of your body. If you don't have enough iron, your lungs are doing the work, but the delivery truck is empty. Your heart has to pump harder to move that oxygen-depleted blood around. It’s a systemic bottleneck.
The Subtle Warning Signs of Low Iron
Most people miss the early stages. It starts as a slight dip in productivity or a bit of irritability. You might find yourself out of breath walking up a flight of stairs that you used to breeze through. This happens because your muscles are literally starving for oxygen.
One of the most bizarre symptoms of low iron is pica. This is a medical term for craving things that aren't food. We aren't talking about a craving for pickles; we're talking about an intense, overwhelming urge to chew on ice, dirt, clay, or even paper. If you find yourself raiding the freezer specifically to crunch on the frost buildup, your body is screaming for minerals. It sounds fake, but it’s a documented neurological response to iron deficiency.
Then there’s the "spoon nail." Doctors call it koilonychia. Your fingernails become thin and brittle. Eventually, they might even curve inward, creating a little dip deep enough to hold a drop of liquid. It’s a slow-motion physical change that most people ignore by applying more nail strengthener, when they should be checking their ferritin levels.
Why Your Legs Won't Stay Still at Night
Have you ever been laying in bed, finally ready to sleep, but your legs feel like they have electric current running through them? Restless Legs Syndrome (RLS) is frequently tied to how the brain processes dopamine, and iron is a crucial cofactor in dopamine production. Research from the Johns Hopkins Center for Restless Legs has shown that even if your blood count is "normal," low iron stores in the brain can trigger that miserable, jittery crawling sensation. It’s not just in your head. It’s in your iron-starved nerves.
✨ Don't miss: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
What Your Tongue is Trying to Tell You
Take a look in the mirror. A healthy tongue is usually bumpy and pink. If yours looks strangely smooth, pale, or feels swollen and sore, that’s a red flag. This is called glossitis. When iron levels drop, so do levels of myoglobin, a protein in red blood cells that supports muscle health—including the muscles of the tongue.
It can even change how you eat. Some people notice that spicy foods suddenly sting more, or they develop cracks at the corners of the mouth (angular cheilitis). It’s uncomfortable. It’s annoying. And it’s almost always a sign that your internal iron stores—the ferritin—are running on fumes.
The Cold Hand Mystery
We all know that person who always has cold hands. Maybe that person is you. While poor circulation can be caused by many things, iron deficiency is a prime suspect. Without enough hemoglobin to carry heat-regulating oxygen to your extremities, your body prioritizes your core organs. Your fingers and toes are the first to lose out. If you’re wearing a sweater in a 75-degree room, it might not be the thermostat; it might be your blood.
The Gap Between "Normal" and "Optimal"
Here is where it gets frustrating. You go to the doctor, they run a CBC (Complete Blood Count), and they tell you you’re "fine" because you aren't anemic yet. But there is a massive difference between iron deficiency and iron deficiency anemia.
- Iron Deficiency: Your storage (ferritin) is low. You feel like garbage.
- Iron Deficiency Anemia: Your storage is gone AND your red blood cell count has dropped.
You can experience severe symptoms of low iron long before you technically become "anemic." Many labs list a "normal" ferritin range as anything from 15 to 150 ng/mL. However, many hematologists, like those at the Iron Disorders Institute, suggest that people start feeling symptoms when ferritin drops below 30 or even 50. If your doctor only checks your hemoglobin and skips the ferritin test, they are missing half the story.
🔗 Read more: Medicine Ball Set With Rack: What Your Home Gym Is Actually Missing
The Brain Fog Factor
Lack of iron doesn't just make your body tired; it makes your brain sluggish. Iron is involved in the synthesis of neurotransmitters. When it's low, you might experience "brain fog," a lack of focus, or even symptoms that mimic depression and anxiety. It’s hard to feel mentally sharp when your brain cells are oxygen-starved. You aren't lazy. You're chemically disadvantaged.
Who Is Actually at Risk?
It isn't just people who don't eat meat. While vegetarians and vegans have to be more mindful of "non-heme" iron absorption, plenty of omnivores struggle too.
- Women with heavy cycles: This is the number one cause. If you lose more blood every month than your diet can replace, you’re in a permanent deficit.
- Frequent blood donors: You’re doing a great thing, but you're literally giving away your iron.
- Endurance athletes: "Foot-strike hemolysis" is a real thing. The physical impact of running can actually break down red blood cells in the feet. Plus, you lose iron through sweat.
- People with gut issues: If you have Celiac disease, Crohn’s, or even just take a lot of antacids (PPIs), your stomach might not be acidic enough to break down and absorb iron properly.
Real Steps to Fix Your Iron Levels
Stop buying the first cheap supplement you see at the drugstore. Most of them are ferrous sulfate, which is notorious for causing stomach pain and constipation. Many people quit taking their iron because the side effects are worse than the fatigue.
Get the right tests. Ask for a full iron panel. This includes Serum Iron, Total Iron Binding Capacity (TIBC), and most importantly, Ferritin. Don't settle for just a hemoglobin check.
Heme vs. Non-Heme. Iron from animal sources (heme) is absorbed much more efficiently than iron from plants (non-heme). If you’re plant-based, you need to eat significantly more iron-rich foods to get the same result. Think lentils, spinach, and fortified cereals.
💡 You might also like: Trump Says Don't Take Tylenol: Why This Medical Advice Is Stirring Controversy
The Vitamin C trick. This is non-negotiable for non-heme iron. If you’re eating spinach or taking a pill, pair it with a glass of orange juice or some bell peppers. Vitamin C helps your gut pull that iron in.
Avoid the blockers. Coffee and tea contain tannins and polyphenols that bind to iron and prevent it from being absorbed. If you take your iron supplement with your morning latte, you’re basically flushing the money down the toilet. Wait at least an hour between caffeine and iron.
Consider the formulation. If standard pills hurt your stomach, look into "Liquid Iron" (like Floradix) or "Heme Iron" supplements. They tend to be much gentler on the digestive tract.
Moving Forward With Intention
Managing the symptoms of low iron isn't a weekend project. It takes months to rebuild ferritin stores. If you start a supplement today, you might not feel "great" for six to eight weeks. That’s the reality of how our bodies regenerate red blood cells.
Start by tracking your energy levels alongside your diet for two weeks. If you notice the "pica" cravings or the restless legs, stop guessing and get the bloodwork. If you find your ferritin is low, work with a professional to find a dose that doesn't upset your stomach. Be consistent. Iron deficiency is one of the most common nutritional deficiencies in the world, but it’s also one of the most treatable once you stop dismissing your exhaustion as "just life."
Check your latest lab results. If your ferritin is under 30 ng/mL, it's time to have a direct conversation with your GP or a hematologist about a supplementation plan that actually works for your lifestyle.