Everyone talks about high blood pressure. It’s the "silent killer," the boogeyman of the doctor's office. But what happens when that bottom number—the diastolic pressure—is sitting in the 40s or 50s? You feel like a ghost. Honestly, it's exhausting. You stand up, the room spins, and you’re suddenly gripping the kitchen counter just to stay upright. If you've ever wondered how can you raise diastolic blood pressure without sending your top number into the stratosphere, you're not alone, and it’s actually a pretty tricky needle to thread.
Diastolic pressure represents the force in your arteries when your heart is resting between beats. Think of it like the "baseline" tension in your pipes. When that baseline drops too low—a condition doctors call isolated diastolic hypotension (IDH)—your organs, especially your heart, might not be getting the oxygen-rich blood they need during those crucial resting moments.
What’s Actually Happening When Diastolic Pressure Dips?
Most people focus on the systolic (top) number because it’s the one linked to strokes and heart attacks. But the diastolic number is when the coronary arteries actually fill with blood. If the pressure is too low, the heart is essentially "starving" between beats.
Standard medical guidelines usually define a healthy reading around 120/80 mmHg. If your bottom number is consistently under 60 mmHg, you’re in the low zone. Interestingly, many people who struggle with this are actually older adults who have stiff arteries, or younger people with specific autonomic issues like POTS (Postural Orthostatic Tachycardia Syndrome). It’s not just about "being fit." Sometimes, your body’s plumbing just isn't holding the pressure it should.
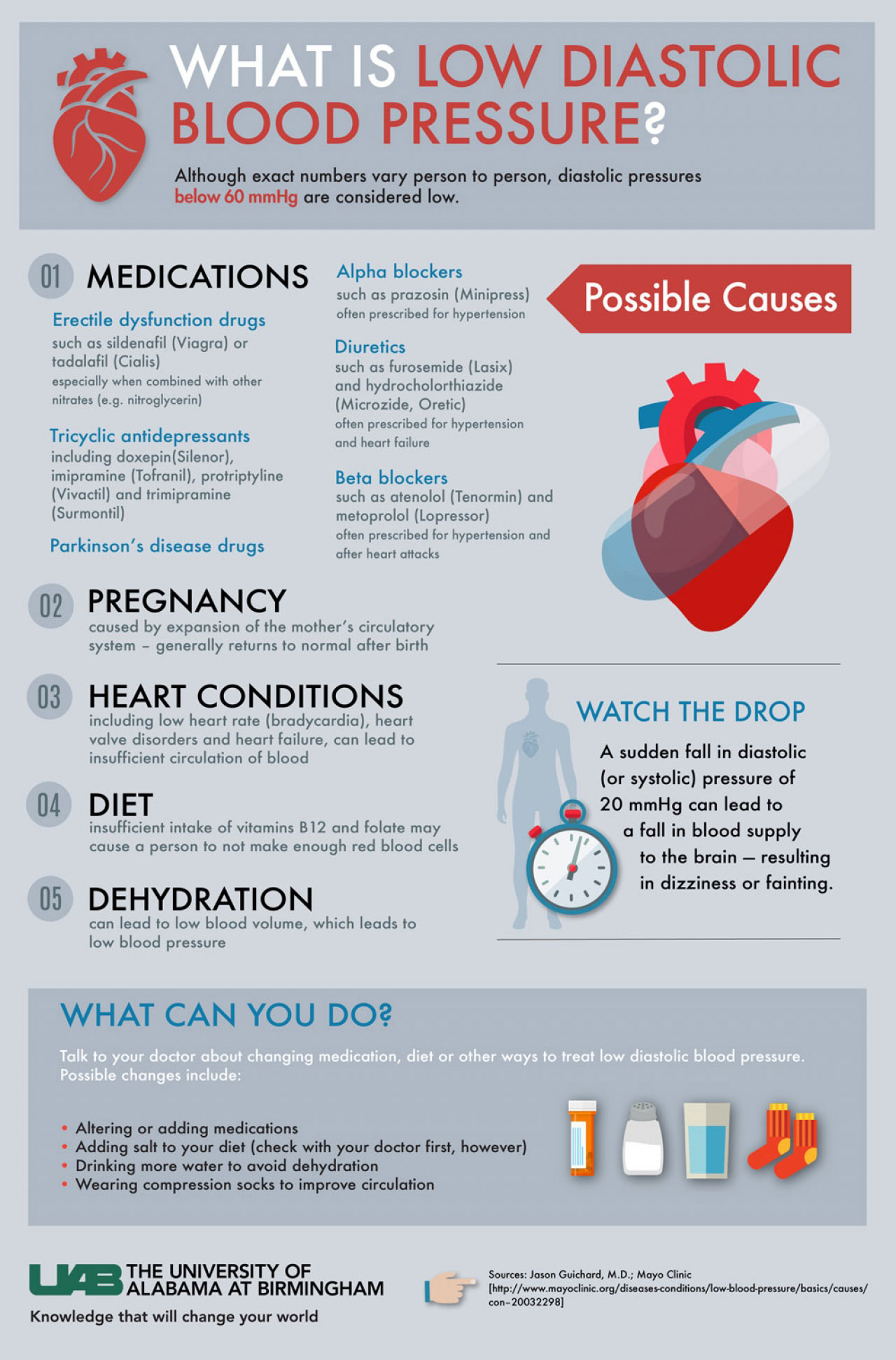
Why does it happen? Aging is the big one. As we get older, our arteries lose their "bounce." They get stiff. Instead of snapping back and maintaining pressure between beats, they stay rigid. Other times, it’s medication. You might be taking a diuretic for your systolic pressure that’s absolutely tanking your diastolic pressure as a side effect. It’s a delicate balance.
How Can You Raise Diastolic Blood Pressure Without Overdoing It?
The biggest challenge is that most things that raise the bottom number also raise the top one. You don't want to fix your 55 diastolic reading only to end up with a 160 systolic reading. That’s dangerous.
✨ Don't miss: Finding the Right Care at Texas Children's Pediatrics Baytown Without the Stress
Salt is your first lever. But don't just dump table salt on everything. You need to be strategic. Increasing sodium intake expands your total blood volume. More fluid in the pipes equals more pressure. A study published in the Journal of the American College of Cardiology suggests that for those with symptomatic low pressure, increasing daily sodium to about 3,000–5,000 mg can help, provided you don't have underlying kidney issues.
Hydration is the second lever. It’s boring, but it works. If you’re dehydrated, your blood volume drops, and your diastolic pressure is the first thing to go. You should be drinking enough that your urine is pale yellow. If it’s dark, your pressure is going to stay low.
The Power of Compression
If you want to know how can you raise diastolic blood pressure instantly, look at your legs. Gravity is your enemy here. When you stand, blood pools in your lower extremities. This is why many people with low diastolic pressure feel dizzy when they get out of bed.
Graduated compression stockings (20-30 mmHg) are a literal lifesaver. By squeezing the veins in your calves and thighs, they force blood back up toward the heart, maintaining that baseline pressure. It’s not glamorous, and they’re a pain to put on, but the physiological shift is measurable within minutes. Some specialized clinics even recommend abdominal binders, which do the same thing for the blood that pools in your gut.
Adjusting Your Daily Habits
Small tweaks to how you move and eat can shift the needle more than you’d think.
🔗 Read more: Finding the Healthiest Cranberry Juice to Drink: What Most People Get Wrong
- Eat smaller, frequent meals. Big meals require a lot of blood flow to the digestive system. This "borrows" blood from the rest of the body, causing a post-meal dip in pressure.
- Watch the caffeine. While a cup of coffee can provide a temporary spike, it’s also a diuretic. If you don't follow it with water, you’ll end up lower than where you started.
- Cross your legs. If you're sitting and feel a bit "faded," crossing your legs at the knees can actually help push blood back toward your torso.
Understanding the Role of Medications
Sometimes, the answer to how can you raise diastolic blood pressure is actually stopping something. Many people are over-medicated. Beta-blockers, calcium channel blockers, and especially alpha-blockers used for prostate issues can crush diastolic pressure.
If you’re on blood pressure meds and your diastolic is hitting 50, you need a serious chat with your cardiologist. They might switch you to a different class of drug or adjust the timing. For example, taking meds at night instead of the morning can sometimes stabilize those daytime lows. In rare, severe cases, doctors might prescribe Fludrocortisone or Midodrine. These aren't "daily vitamins"—they are serious medications that help the body retain salt or constrict blood vessels.
Is It Your Heart or Your Nervous System?
It’s worth noting that low diastolic pressure can be a "canary in the coal mine" for other issues. An echocardiogram can check if your heart valves are leaking. A condition called aortic regurgitation—where the valve doesn't close properly—allows blood to leak backward into the heart, which causes the diastolic pressure to plummet because the "pipes" aren't holding the seal.
On the other hand, it could be your autonomic nervous system. This is the system that tells your blood vessels to constrict when you stand up. If that system is sluggish (common in diabetes or Parkinson’s), your pressure will stay low regardless of how much salt you eat. This is why a "tilt table test" is often used to see how your body reacts to gravity in a controlled setting.
Actionable Steps to Stabilize Your Numbers
You can’t fix this overnight, but you can manage it. Start by tracking your numbers at the same time every day. Use a high-quality upper-arm cuff—wrist monitors are notoriously finicky for low-pressure readings.
💡 You might also like: Finding a Hybrid Athlete Training Program PDF That Actually Works Without Burning You Out
First, increase your fluid intake by at least 20 ounces a day. Add an electrolyte powder if you’re active.
Second, look at your footwear and leg support. If you're standing all day, compression isn't optional; it's a requirement.
Third, do "muscle pumping" exercises before you get out of bed. Flex your calves, clench your fists, and move your ankles in circles for 60 seconds before you stand up. This "primes the pump" and prevents that sudden diastolic drop.
Fourth, audit your supplements. High doses of vitamin B3 (niacin) or certain herbal teas like hibiscus can lower blood pressure. You might be inadvertently tanking your own numbers with your "healthy" routine.
Raising diastolic pressure is a slow game of volume management and vascular support. It’s about making your circulatory system "tighter" and fuller. If you’ve made these changes and still feel like you're walking through a fog, it's time for a formal workup to ensure your heart valves are doing their job correctly. Focus on the basics: salt, water, and squeeze.