If you’ve ever stood in the middle of a room wondering why you walked in there, you’ve felt that tiny flicker of dread. For most of us, it’s just a "senior moment" or being distracted by a smartphone. But for millions, that flicker turns into a permanent fog. Scientists have been chasing the answer to why does Alzheimer happen for over a century now, and honestly? The answer is a lot more complicated than just "getting old." It’s a biological train wreck that starts decades before the first car key goes missing.
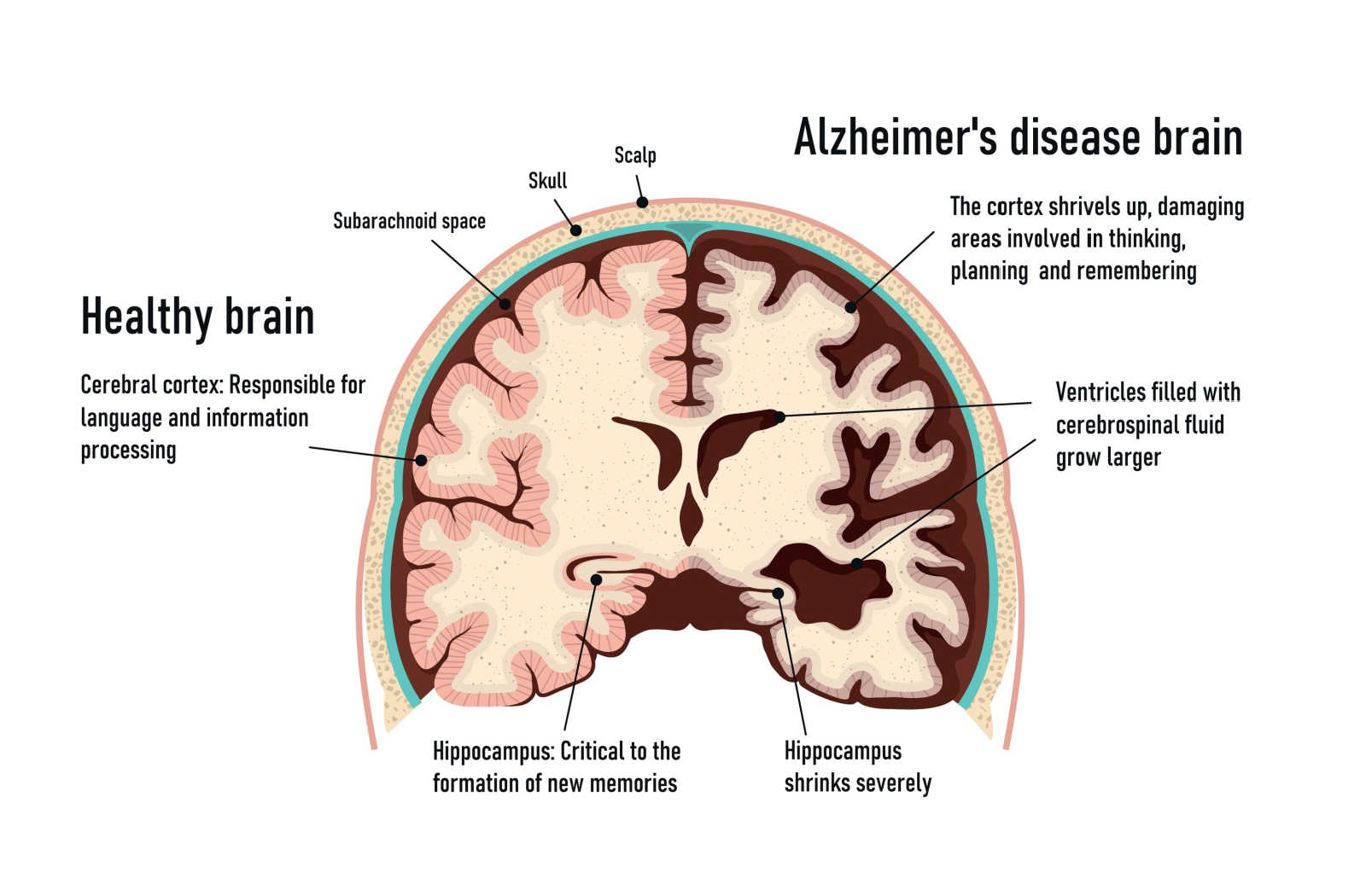
Alzheimer’s isn't a normal part of aging. It’s a specific, aggressive disease. It eats away at the brain’s architecture, starting in the hippocampus—the part responsible for forming new memories. You’ve probably heard of plaques and tangles. Those are the villains in the traditional story. But lately, the medical community is starting to realize these might just be the crime scene evidence, not the actual killer.
The Protein Problem: Amyloid and Tau
Most doctors will tell you that the "Big Two" are amyloid-beta and tau. Think of amyloid-beta as a sticky trash that builds up outside the brain cells (neurons). In a healthy brain, your glymphatic system—basically the brain’s nightly cleaning crew—flushes this stuff out while you sleep. But for some reason, in people with Alzheimer's, the trash doesn't get picked up. It clumps together into plaques. These plaques sit between neurons and block the signals. It's like having a bunch of gum stuck in a circuit board.
Then there’s tau. This one is different. Tau is a protein that normally lives inside the neurons. It acts like railroad ties, keeping the internal transport system of the cell straight and functional. When why does Alzheimer happen becomes the central question, tau is often the smoking gun. In a diseased brain, the tau collapses into twisted "tangles." Once those ties break, the tracks fall apart. The cell can no longer transport nutrients or communicate. It starves. It dies.
Is it just the plaques? Probably not. We know this because some people die with brains full of amyloid plaques but never showed a single sign of dementia while they were alive. This is the "Cognitive Reserve" theory. It suggests that some brains are just better at "rewiring" around the damage.
The Inflammation Theory: The Brain on Fire
Recently, the focus has shifted. A lot of researchers, like those at the Harvard-led McCance Center for Brain Health, are looking at neuroinflammation. Your brain has its own immune system, primarily made of cells called microglia. Usually, microglia are the good guys. They gobble up debris and protect the brain from infections.
But in Alzheimer’s, they go haywire.
🔗 Read more: In the Veins of the Drowning: The Dark Reality of Saltwater vs Freshwater
They see the amyloid plaques and treat them like a permanent infection. They stay "on" all the time, pumping out inflammatory chemicals. Instead of cleaning the house, they end up burning it down. This chronic inflammation might be the real reason the neurons eventually give up the ghost. It's a vicious cycle: plaques cause inflammation, inflammation damages cells, and damaged cells create more debris that triggers more inflammation.
Is It "Type 3 Diabetes"?
This is where things get really interesting and a bit controversial. Some researchers, including Dr. Suzanne de la Monte at Brown University, have started calling Alzheimer’s "Type 3 Diabetes." Why? Because the brain is a massive energy hog. Even though it's only about 2% of your body weight, it consumes about 20% of your energy. That energy comes from glucose.
In many Alzheimer’s patients, the brain loses its ability to process glucose efficiently. It becomes insulin resistant. When the brain can't get the fuel it needs, neurons start to flicker out. It’s like a city experiencing a rolling blackout. This explains why people with Type 2 diabetes are at a significantly higher risk for dementia. If the "power grid" is failing, the memories go dark.
The Role of Genetics (And It’s Not Just One Gene)
"Is it in my genes?" That’s the first thing everyone asks.
The answer is: sometimes.
There are two types of Alzheimer's. The "Early Onset" version is rare—less than 5% of cases—and is usually tied to specific mutations in three genes: APP, PSEN1, and PSEN2. If you have these, you’re almost guaranteed to get the disease, often in your 40s or 50s. It’s a heavy burden.
💡 You might also like: Whooping Cough Symptoms: Why It’s Way More Than Just a Bad Cold
The "Late Onset" version, which is what most people deal with, is much more "sorta-maybe." The biggest genetic risk factor here is the APOE-e4 gene. If you have one copy from a parent, your risk increases. If you have two? The risk is significantly higher. But—and this is a huge "but"—having the gene doesn't mean you'll definitely get it. It just means your brain is less efficient at clearing out that amyloid "trash" we talked about earlier.
The Surprising Impact of Lifestyle and Environment
We used to think the brain was a sealed vault. We now know it's incredibly sensitive to how we treat the rest of our body. Vascular health is brain health. If your heart is struggling to pump blood, or if your arteries are stiff from high blood pressure, your brain isn't getting enough oxygen.
Sleep is another huge factor. During deep sleep, the brain's "trash disposal" system (the glymphatic system) is ten times more active than when you’re awake. If you’re chronically sleep-deprived, you’re essentially letting metabolic waste pile up in your skull.
Then there’s the "use it or lose it" factor. People with higher levels of education or those who stay socially active tend to develop symptoms later. It's not that their brains don't have the plaques; it's that they have more "backup routes" for information to travel.
Factors That Might Trigger the Cascade:
- Chronic Stress: High cortisol levels are toxic to the hippocampus over long periods.
- Hearing Loss: This one is wild. Untreated hearing loss is one of the biggest modifiable risk factors. When the brain has to work too hard to decode sound, it has less "processing power" for memory. Or, the lack of input causes parts of the brain to atrophy.
- Gum Disease: No joke. Porphyromonas gingivalis, the bacteria behind gingivitis, has been found in the brains of Alzheimer’s patients. It may trigger that "brain on fire" inflammation.
Why Do We Still Not Have a Cure?
It's frustrating. We’ve spent billions. We’ve had hundreds of failed drug trials. For a long time, we were "Amyloid-Centric." We developed drugs that cleared the plaques perfectly. The scans looked great! But the patients didn't get better.
This taught us a brutal lesson: by the time someone has enough memory loss to go to a doctor, the damage is already done. The neurons are gone. You can’t fix a house that has already burned down just by clearing away the charred wood.
📖 Related: Why Do Women Fake Orgasms? The Uncomfortable Truth Most People Ignore
The new frontier is Prevention and Early Detection. We are looking at blood tests that can spot the disease 20 years before you forget where you parked. If we can intervene while the "fire" is just a tiny spark, we have a chance.
What You Can Actually Do Today
Waiting for a magic pill isn't a great strategy. Since we know why does Alzheimer happen involves a mix of blood flow, inflammation, and protein buildup, we can attack those fronts right now.
1. Fix Your Sleep Architecture
Stop treating sleep like a luxury. You need 7-8 hours to let your brain "wash" itself. If you snore, get checked for sleep apnea. Apnea starves the brain of oxygen and is a massive driver of cognitive decline.
2. The "MIND" Diet
It’s basically Mediterranean meets DASH. Lots of leafy greens, berries, nuts, and olive oil. Most importantly? Cut the ultra-processed sugars. If your brain is becoming "insulin resistant," the last thing it needs is a flood of high-fructose corn syrup.
3. Get Moving (Even a Little)
Exercise is the only thing we know of that actually boosts Brain-Derived Neurotrophic Factor (BDNF). Think of BDNF as Miracle-Gro for your neurons. It helps them repair and grow new connections.
4. Protect Your Ears
If you can't hear the conversation at a party, get a hearing aid. It’s not about vanity; it’s about keeping your brain’s input channels open. Social isolation is a fast track to cognitive decline.
5. Manage Your Blood Pressure
What's good for the heart is good for the head. Mid-life high blood pressure is one of the strongest predictors of late-life dementia. Keep those "pipes" clear so the brain stays oxygenated.
The reality of Alzheimer’s is that it’s rarely one single thing. It’s a "perfect storm" of genetics, lifestyle, and a bit of bad luck. But understanding the "why" gives us the power to change the "when." By focusing on brain health in our 30s, 40s, and 50s, we aren't just living longer—we're living better. The goal isn't just to add years to life, but life to those years.