Finding a smudge of light pink on the toilet paper can be a real "wait, what?" moment. It’s not quite blood, but it’s definitely not your usual clear or white discharge. Honestly, most people freak out a little bit when it happens. You start scrolling through forums, wondering if it's a weird period, an infection, or something you need to call the doctor about immediately.
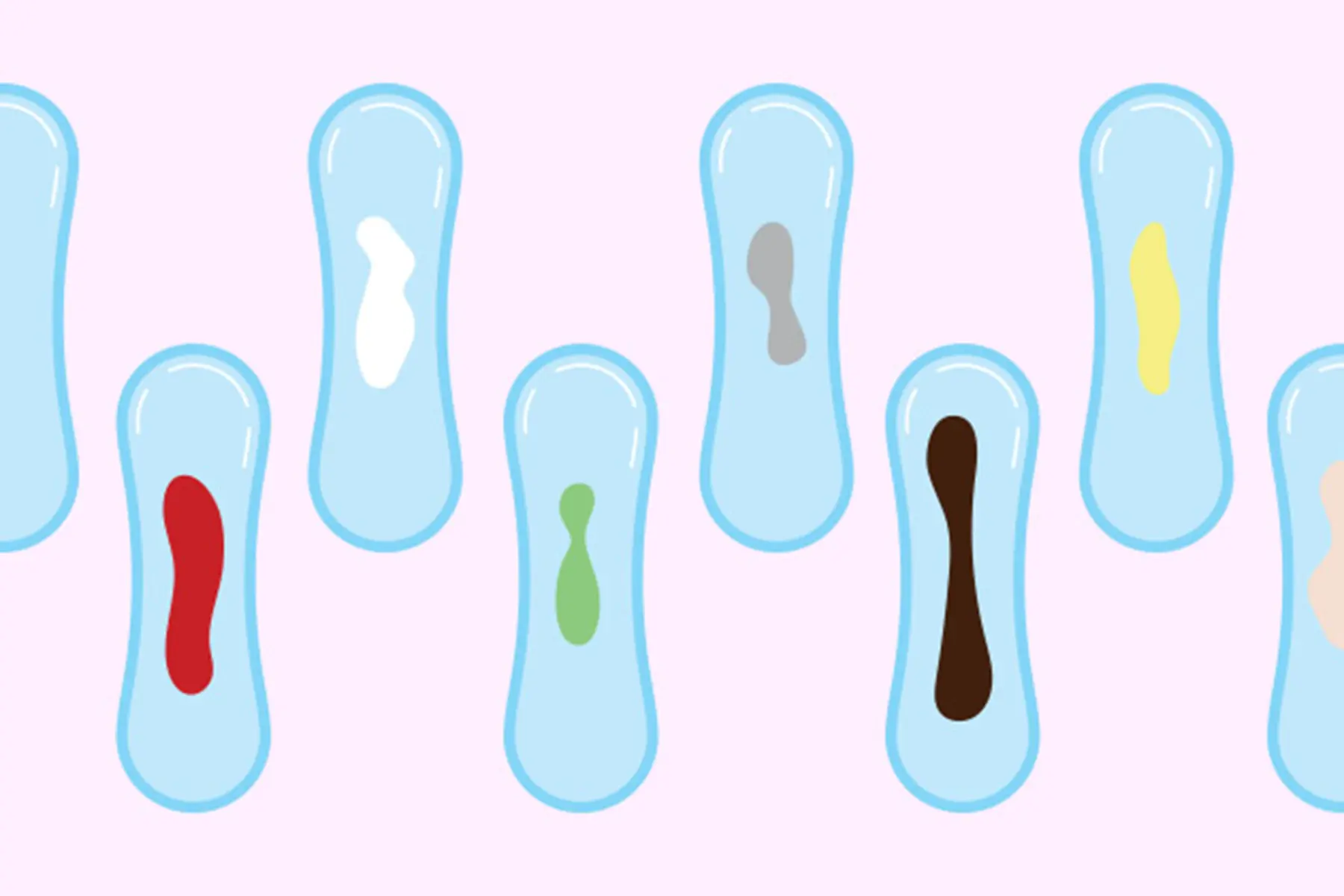
Basically, light pink discharge is just cervical mucus or vaginal fluid mixed with a tiny amount of fresh blood. That's it. The "pink" part happens because the blood is diluted. It hasn't had time to oxidize and turn that crusty brown color we usually see at the end of a period.
But why is it happening right now? That's the real question.
The Most Likely Culprits Behind Why Do I Have Light Pink Discharge
If you’re mid-cycle, you might be looking at ovulation spotting. When your follicle ruptures to release an egg, it can cause a brief drop in estrogen or a tiny bit of physical trauma to the follicle itself. This leads to a day or two of light pink discharge. It’s actually a sign of fertility for many. Some people even track this as part of their "fertility window" alongside basal body temperature.
Then there’s the stuff that happens after a long night. Or a short one. Post-coital spotting is incredibly common. The tissues of the cervix and vagina are delicate. If things get a little too vigorous, or if there isn’t enough lubrication, you end up with micro-tears. These tiny scratches bleed just a smidge. Mix that with your natural lubrication, and boom—you’ve got pink discharge.
Hormones are usually the puppet masters here.
If you just started a new birth control pill, or perhaps you got the Nexplanon arm implant or an IUD, your uterine lining is likely a bit unstable. Doctors call this "breakthrough bleeding." It's annoying. It's frustrating. But it’s usually just your body recalibrating to the new synthetic hormone levels. According to the American College of Obstetricians and Gynecologists (ACOG), this is the number one reason people stop using their birth control, even though it usually settles down after three to six months.
✨ Don't miss: Fruits that are good to lose weight: What you’re actually missing
Implantation Bleeding vs. The Start of a Period
This is where the Google searches get frantic.
A lot of people want to know if that pink smudge is implantation bleeding. This happens when a fertilized egg attaches to the lining of the uterus, usually about 6 to 12 days after conception. It's lighter than a period. It doesn't last long. It rarely involves heavy cramping.
However—and this is a big "however"—implantation bleeding is actually less common than the internet makes it out to be. A study published in Human Reproduction found that most women do not experience bleeding during early pregnancy. If you do, it’s often just a tiny bit of spotting. If it's pink and happens a few days before your expected period, it could be implantation, but you won't know for sure until you take a test.
Wait a few days. Testing too early just leads to "evaporation line" paranoia.
When It’s Not Just "One of Those Things"
Sometimes, the reasons are a bit more clinical.
Cervical ectropion sounds scary, but it’s basically just when the cells from inside the cervical canal grow on the outside of the cervix. These cells are much more sensitive and prone to bleeding. It’s very common in people taking estrogen-based birth control or those who are pregnant. If your doctor does a Pap smear and says your cervix looks "friable," this is what they mean. It bleeds if you so much as look at it funny.
🔗 Read more: Resistance Bands Workout: Why Your Gym Memberships Are Feeling Extra Expensive Lately
Then we have Pelvic Inflammatory Disease (PID) or certain STIs like Chlamydia or Gonorrhea.
Usually, if it’s an infection, the light pink discharge won't be the only symptom. You’ll probably notice:
- An odor that seems "off" or fishy.
- Pelvic pain that feels like a dull, heavy ache.
- Burning when you pee.
- Pain during deep penetration.
If you have those symptoms along with the pink tint, get a swab. It’s better to clear it up with antibiotics now than to let it linger and potentially cause scarring in your fallopian tubes.
Perimenopause: The Unpredictable Shift
If you’re in your late 30s or 40s, why do i have light pink discharge might be a sign of the "big change" starting its slow engine. Perimenopause makes your cycles go haywire. Your estrogen levels don't drop in a straight line; they rollercoaster. This can lead to your uterine lining shedding in bits and pieces rather than all at once. You might have pink spotting for three days, nothing for a week, and then a heavy period. It’s chaotic, but it’s a standard part of the transition.
The Role of Stress and Weight Changes
Your hypothalamus—the part of your brain that runs your hormonal show—is a sensitive little thing. If you are under extreme stress, like a death in the family or a massive project at work, your brain might decide that now is a terrible time to potentially be pregnant. It might delay ovulation or cause "estrogen breakthrough bleeding."
The same goes for sudden weight loss or intense "marathon-style" exercise. If your body fat drops too low, your hormone production stalls. You might see light pink spotting instead of a real period because your lining never got thick enough to truly shed.
💡 You might also like: Core Fitness Adjustable Dumbbell Weight Set: Why These Specific Weights Are Still Topping the Charts
Fibroids and Polyps
Non-cancerous growths like uterine fibroids or cervical polyps can also be the culprit. Polyps are like little skin tags hanging off the cervix or inside the uterus. They have a lot of blood vessels. If they get bumped—by a tampon, by sex, or even by a bowel movement—they can bleed just enough to turn your discharge pink.
Fibroids, on the other hand, are muscular growths in the uterine wall. While they usually cause heavy, "crime scene" style periods, they can also cause spotting between cycles because they distort the uterine lining.
How to Tell if You Should See a Doctor
Look, most of the time, this isn't an emergency. But there are red flags.
If the pink discharge turns into bright red blood that soaks a pad every hour, that’s not "spotting." That’s a hemorrhage, and you need to go to the ER or urgent care. Similarly, if you are post-menopausal—meaning you haven't had a period in over a year—and you see any pink discharge, call your gynecologist immediately. Post-menopausal bleeding is never "normal" and always needs to be checked to rule out endometrial cancer, even if it's just a tiny pink smudge.
Also, keep an eye on the timing. Is it always after sex? Always on day 14 of your cycle? Keeping a log on an app like Clue or Flo can help your doctor figure out the pattern.
Actionable Steps To Take Now
Instead of spiraling, take these concrete steps to figure out what's going on:
- Take a pregnancy test: If you’ve had unprotected sex in the last month, this is step one. It eliminates the "is it implantation?" guesswork.
- Check your calendar: Pinpoint exactly where you are in your cycle. If you are 14 days after the start of your last period, it’s likely ovulation. If you are 2 days away from your period, it’s just the "pre-game" spotting.
- Hydrate and Lubricate: If the spotting happens after sex, try using a high-quality, pH-balanced lubricant. If the spotting stops, you've found your answer: it was just friction.
- Monitor for 48 hours: In many cases, light pink discharge is a "one and done" event. If it disappears within two days and you feel fine otherwise, it’s usually just a hormonal hiccup.
- Schedule a "Well-Woman" Exam: If the spotting is persistent (happening every month) or accompanied by pain, get a pelvic exam. Ask for a transvaginal ultrasound if the doctor suspects polyps or fibroids.
Bottom line: Light pink discharge is usually just a signal that your hormone levels are shifting or your delicate tissues took a minor hit. It’s a "yellow light" from your body—a signal to slow down and pay attention, but rarely a reason to panic.
Next Steps for Your Health:
If you're currently experiencing this and also have a fever or sharp one-sided pelvic pain, seek medical attention to rule out an ectopic pregnancy or acute infection. Otherwise, start a cycle log today to track the frequency of the spotting. This data is the most valuable tool you can give your healthcare provider during your next check-up.