You’re sitting in the doctor’s office. The cuff squeezes your arm tight, then releases with that familiar hiss. The nurse rattles off two numbers, maybe 125 over 95. Most of the time, we obsess over that first number—the systolic. It's the big one. The loud one. But then you realize that second number, the diastolic, is creeping up into the 90s or even higher. It feels weird. Why is the bottom number high when the top one seems mostly fine?
It's actually called isolated diastolic hypertension (IDH).
Honestly, a lot of people just ignore it. They think as long as the top number isn't 160, they’re in the clear. But that's a mistake. That bottom number represents the pressure in your arteries when your heart is resting between beats. If that pressure stays high, your blood vessels never get a break. It's like keeping a garden hose turned on full blast even when you aren't watering the plants; eventually, something is going to leak or burst.
What is actually happening when the bottom blood pressure number is high?
Blood pressure is a measurement of force. The top number (systolic) is the "work" phase—when your heart pumps. The bottom number (diastolic) is the "rest" phase. When you ask why bottom blood pressure number is high, you're really asking why your vascular system is staying tense even when the pump is off.
Usually, this happens because the smaller arteries in your body, the arterioles, have become stiff or narrow. They aren't relaxing. This creates a sort of "backlog" of pressure. Imagine a traffic jam where the cars at the front won't move even when the light turns green. The pressure builds up all the way down the line.
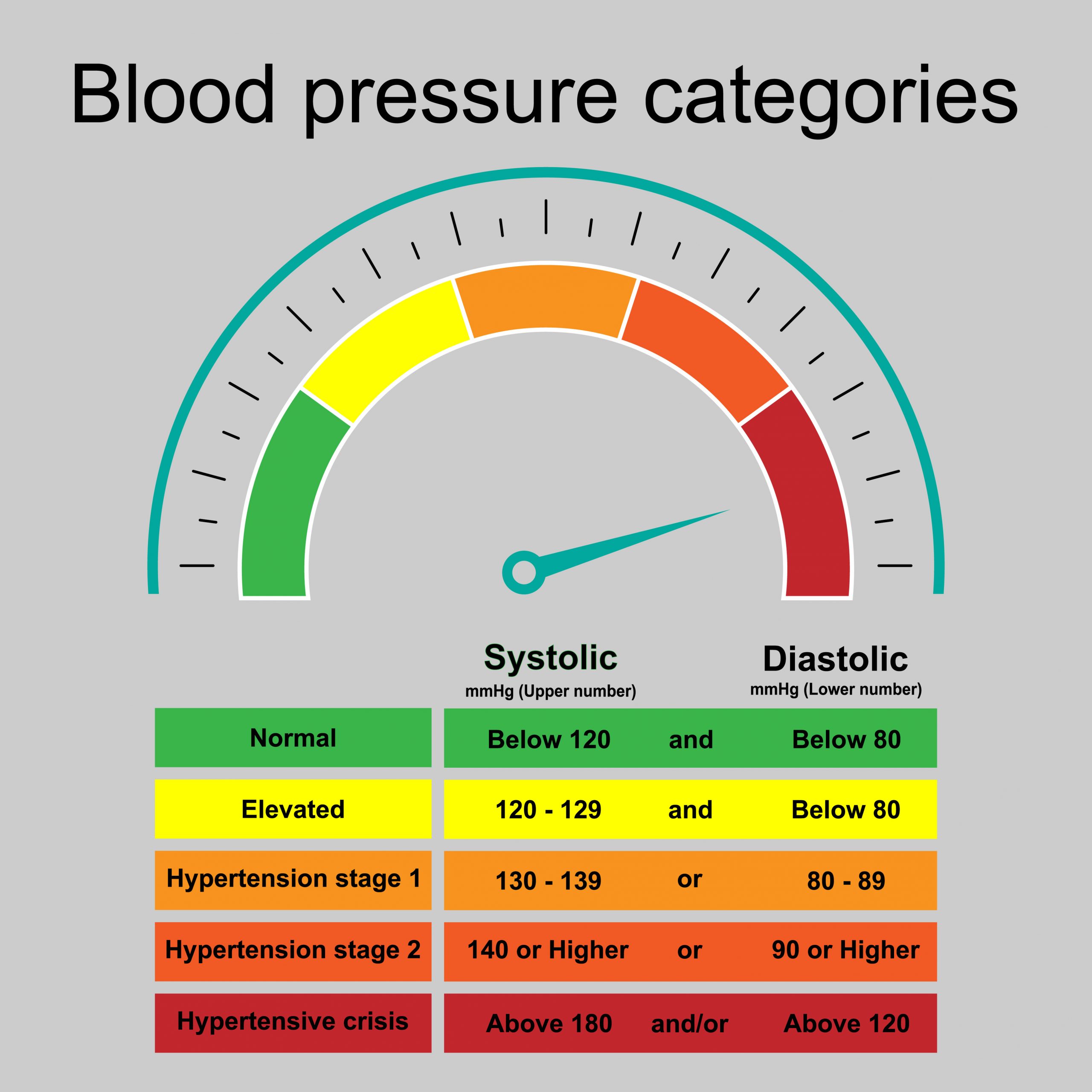
According to the American College of Cardiology and the American Heart Association, a "normal" diastolic reading should be under 80 mmHg. If you’re consistently hitting 80 to 89, you’re in Stage 1 hypertension territory. Once you cross 90, you’re in Stage 2. It’s a bit of a wake-up call. Interestingly, IDH is actually more common in younger adults—specifically those under 50—than in the elderly. While older adults tend to struggle with high systolic pressure due to stiffening of the large aorta, younger people often have "tight" peripheral vessels that drive that bottom number up.
The lifestyle culprits you already know (but might be ignoring)
We have to talk about salt. I know, it’s boring. But sodium is a chemical magnet for water. When you eat a bag of salty chips or a frozen dinner, that sodium pulls water into your bloodstream. More fluid in the same size "pipes" means higher pressure. If your kidneys can't flush it out fast enough, your diastolic pressure is the first thing to react.
✨ Don't miss: Why Do Women Fake Orgasms? The Uncomfortable Truth Most People Ignore
Then there’s the weight factor. It isn't just about the scale. It's about inflammation. Adipose tissue (fat), especially around the belly, isn't just sitting there; it's metabolically active. It releases chemicals that tell your nervous system to stay in "fight or flight" mode. This keeps your blood vessels constricted.
Alcohol is another big one. People think a drink relaxes them. Maybe it does for twenty minutes. But as your liver processes alcohol, it creates a rebound effect that tightens your arteries. If you’re drinking every night, your bottom number basically never gets a chance to drop back to its baseline.
Surprising reasons why bottom blood pressure number is high
Sometimes it’s not just the salt or the lack of gym time. There are metabolic "glitches" that keep the pressure up.
- Hypothyroidism: This is a sneaky one. When your thyroid is sluggish, your heart beats less forcefully, but your blood vessels actually get stiffer to compensate. This paradoxically pushes the diastolic number up while keeping the systolic number normal.
- Sleep Apnea: If you snore or wake up feeling like a zombie, your oxygen levels are likely dropping at night. Every time you stop breathing, your brain panics and sends a surge of adrenaline to wake you up. That adrenaline spike clamps down on your blood vessels. Even during the day, your body stays "primed" for that stress, keeping the bottom number high.
- Secondary Hyperaldosteronism: This is a mouthful, but it basically means your adrenal glands are pumping out too much of a hormone called aldosterone. This hormone tells your kidneys to hold onto salt and dump potassium. It’s a very common cause of "resistant" high diastolic pressure that doesn't respond well to standard diet changes.
The stress and "sympathetic" overdrive connection
We live in a world that is constantly "on." Your nervous system has two main gears: the sympathetic (fight or flight) and the parasympathetic (rest and digest). If you are constantly stressed, caffeinated, and underslept, you are stuck in sympathetic overdrive.
Your body thinks it’s being chased by a predator. It constricts the blood vessels in your gut and skin to send blood to your muscles. When this happens 24/7, your diastolic pressure never finds the "floor." It stays elevated because the command to "relax" never comes from the brain. It’s a physical manifestation of a lifestyle that doesn't have enough downtime.
Does a high bottom number actually matter?
For a long time, doctors focused almost exclusively on the top number. They figured the systolic pressure was the best predictor of strokes and heart attacks. And for older people, that’s mostly true. But recent data, including a massive study published in the New England Journal of Medicine involving over 1.3 million people, showed that both numbers independently predict cardiovascular risk.
🔗 Read more: That Weird Feeling in Knee No Pain: What Your Body Is Actually Trying to Tell You
If your bottom number is high, you are at an increased risk for:
- Aneurysms: Constant pressure wears down the artery walls until they bulge.
- Kidney Damage: The kidneys are basically bundles of tiny, delicate blood vessels. High diastolic pressure "bruises" them over time.
- Heart Failure: The heart has to push harder against that resting pressure to get blood moving. Over years, the heart muscle gets thick and stiff—a condition called left ventricular hypertrophy.
It’s a slow-motion problem. It doesn't hurt. You can't "feel" a diastolic of 95. That’s why they call it the silent killer. You just go about your day while your organs are slowly being tenderized by excess pressure.
Identifying the "White Coat" effect
Before you panic, check how you’re measuring it. A lot of people get a high reading because they just walked into a clinic, they're worried about the results, and the nurse is talking to them while the cuff is inflating. That’s not a real reading.
To get a real answer on why bottom blood pressure number is high, you need home monitoring. Sit quietly for five minutes. No phone. No TV. Feet flat on the floor. Don’t cross your legs. Take three readings and average them. If it’s still high at home, in your "zen" space, then you have a real physiological issue to address.
Real-world shifts to bring the number down
You don't always need a prescription pill right away, though sometimes they are literal lifesavers. But you can move the needle yourself with some very specific, non-vague changes.
The Potassium Pivot
Most people focus on cutting salt. That’s only half the battle. You need to increase potassium. Potassium acts as a natural vasodilator; it literally tells the smooth muscles in your arteries to "let go." Avocados, spinach, and beans are better for this than bananas, honestly. If you can get your potassium-to-sodium ratio right, your diastolic pressure often drops within weeks.
💡 You might also like: Does Birth Control Pill Expire? What You Need to Know Before Taking an Old Pack
Magnesium for the Win
Magnesium is the body's natural calcium channel blocker. It helps the heart and the vessels relax. Most modern diets are deficient in it because our soil is depleted. Taking a high-quality magnesium glycinate or malate supplement can sometimes drop that bottom number by several points just by allowing the vascular walls to stop "clamping."
Zone 2 Cardio
You don't need to do sprints. In fact, high-intensity intervals can sometimes spike pressure too much if you aren't ready. "Zone 2" is steady-state exercise where you can still hold a conversation but you're definitely working. Think brisk walking or light cycling. This type of exercise improves "vascular compliance"—basically, it makes your pipes more elastic. Elastic pipes handle pressure better than rigid ones.
When should you actually worry?
If your bottom number is consistently over 100, that’s a "don't pass go" situation. You need to see a professional. Also, look out for "pitting edema"—which is just a fancy way of saying your ankles stay indented when you poke them. This means the pressure is so high it's forcing fluid out of your blood vessels and into your tissues.
If you have a high bottom number and you also have headaches, blurred vision, or a weird "thumping" sound in your ears (pulsatile tinnitus), your body is screaming at you. These are signs that the pressure is affecting your neurological system.
Actionable steps to take right now
Stop guessing. If you’ve seen that the bottom blood pressure number is high, follow this protocol for the next 14 days:
- Buy a validated arm cuff monitor. Avoid the wrist ones; they are notoriously finicky and often wrong.
- Track your "Salt-Stress-Sleep" cycle. Write down if you had a high-sodium meal, a bad night's sleep, or a huge deadline. You’ll likely see a direct correlation with your diastolic spikes.
- Cut out the "hidden" salts. It’s not the salt shaker; it’s the bread, the salad dressings, and the "healthy" deli turkey. Read the labels. Aim for under 1,500mg of sodium a day for two weeks.
- Check your meds. Are you taking ibuprofen (Advil/Motrin) daily for aches? NSAIDs are notorious for raising diastolic blood pressure because they mess with kidney blood flow. Switch to something else if you can.
- Get a basic blood panel. Ask your doctor specifically to check your TSH (thyroid) and your electrolytes. If your potassium is on the low end of "normal," that might be your smoking gun.
High diastolic pressure is a fixable problem, but it’s a stubborn one. It requires looking at how you live, how you breathe, and how you fuel your body. It’s not just a number on a screen; it’s the literal tension your body is holding onto. Let it go.