You finally got your blood pressure under control. The numbers on the monitor look great, your doctor is happy, and you feel like you're winning. Then it starts. A tiny tickle. A dry, persistent, "hack-hack-hack" that won't go away no matter how much water you chug or how many honey lozenges you suck on. It’s frustrating. It’s embarrassing in quiet meetings. And honestly, it’s one of the most common reasons people ditch their heart meds. If you're wondering why does acei cause cough, you aren't alone—about 5% to 20% of people taking these drugs end up dealing with this exact same scratchy nightmare.
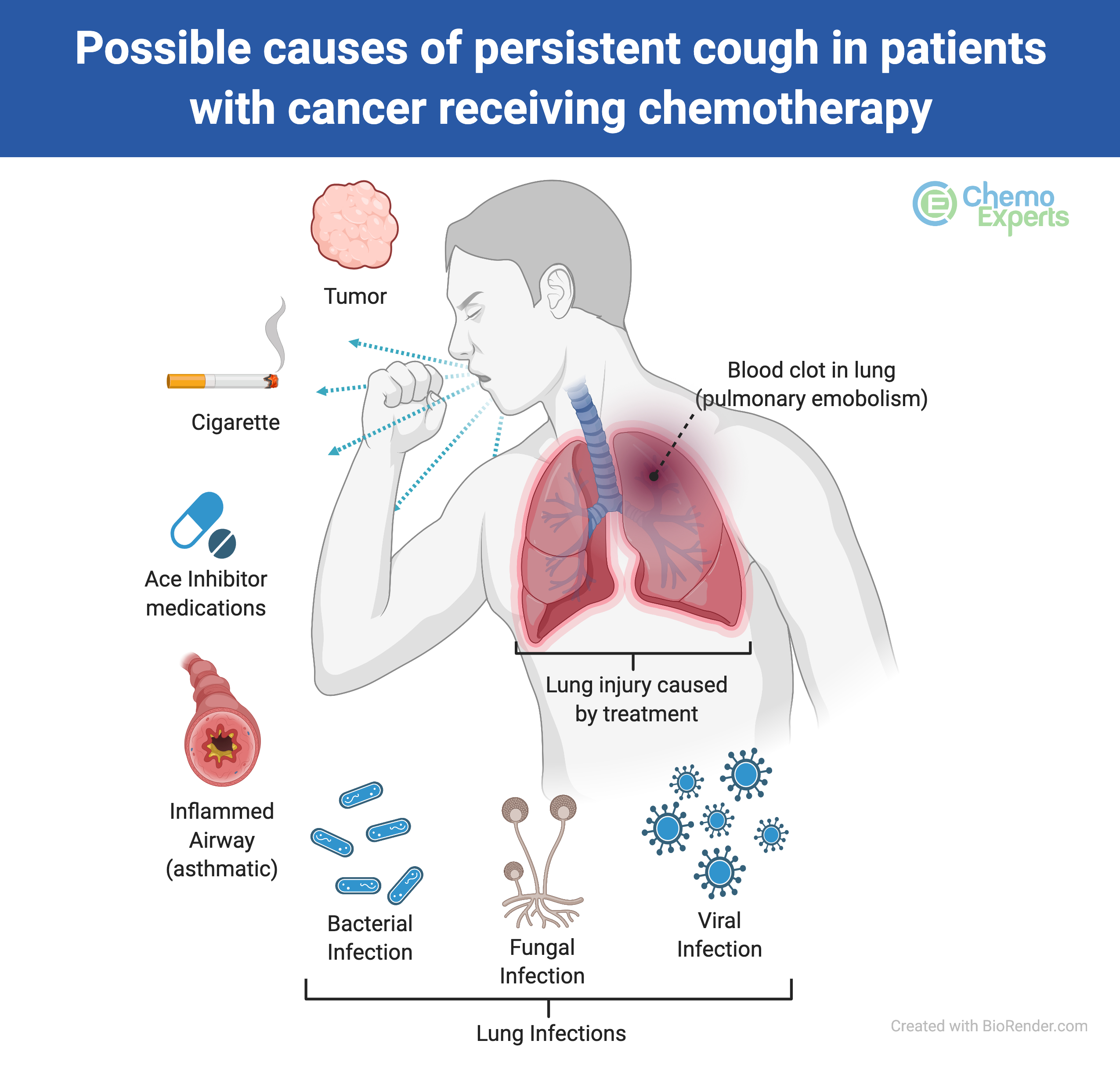
It’s not a cold. It’s not allergies. It is a very specific side effect of drugs like Lisinopril, Enalapril, or Ramipril.
The Science of the "Pril" Hack
To understand why this happens, we have to look at what ACE inhibitors actually do. Their day job is blocking an enzyme called Angiotensin-Converting Enzyme. Usually, this enzyme breaks down a little protein in your body called bradykinin. When you take an ACE inhibitor, that breakdown process stops. Bradykinin starts to build up. It’s like a sink where the drain is plugged; eventually, the water is going to overflow.
Where does it overflow? Right into your lungs and upper airways.
Bradykinin is a vasodilator, which is great for lowering blood pressure, but it’s also a pro-inflammatory substance. When it accumulates in the respiratory tract, it sensitizes your cough receptors. Basically, it makes your throat "hypersensitive." Even a tiny puff of air or a speck of dust that you’d normally ignore suddenly feels like a massive irritation. Your brain gets the signal that something is wrong, and it triggers the cough reflex to clear the "blockage" that isn't actually there.
💡 You might also like: That Weird Feeling in Knee No Pain: What Your Body Is Actually Trying to Tell You
But wait, there’s more. It’s not just bradykinin. Research published in journals like The Lancet and Chest suggests that Substance P and prostaglandins also play a role. These chemicals pool up because the ACE enzyme isn't there to sweep them away. They irritate the sensory C-fibers in your airway. It’s a chemical soup that your lungs simply hate.
Identifying the ACE Inhibitor Cough
How do you know it's the medicine and not just a lingering flu? The ACE inhibitor cough has a few "tells."
First off, it’s dry. You aren't hacking up anything gross or green. It’s just... air. Most people describe it as a persistent tickle or a "scratchy" sensation at the back of the throat. It also tends to get worse when you lie down at night, which can lead to some pretty miserable insomnia.
Timing is another big clue, though it's a tricky one. While many people start coughing within the first week or two of starting their prescription, for others, it takes months. You could be on Lisinopril for six months with zero issues, and then suddenly—wham—the cough starts. This delay often leads patients (and sometimes even doctors) to think it's something else entirely, like new-onset asthma or GERD.
📖 Related: Does Birth Control Pill Expire? What You Need to Know Before Taking an Old Pack
Interestingly, women are statistically more likely to develop this side effect than men. We don't fully know why, though some researchers suspect it has to do with hormonal influences on how bradykinin is processed in the body. Chinese heritage also seems to be a significant risk factor, with some studies showing a much higher incidence in East Asian populations compared to Caucasians.
Is it dangerous?
Generally, no. It’s a nuisance side effect, not a sign that your lungs are failing. However, it’s a massive quality-of-life issue. If you can't sleep or speak a full sentence without hacking, "not dangerous" doesn't mean much.
The one thing you must watch out for is angioedema. This is a much rarer but very serious side effect of ACE inhibitors where your lips, tongue, or throat swell up. If you have a cough plus any swelling in your face or trouble breathing, that’s an ER visit, not a "wait and see" situation.
Why Some People Get It and Others Don't
Genetic lottery. That’s the short answer.
👉 See also: X Ray on Hand: What Your Doctor is Actually Looking For
Specifically, variations in the genes that code for the bradykinin B2 receptor or the ACE enzyme itself determine how much "buildup" your system can handle before it triggers a reflex. Some people have high levels of other enzymes that can step in and break down bradykinin when ACE is occupied. Others don't have that backup system. If your "backup cleaners" are slow, you’re the one who ends up coughing.
Switching Gears: What are the Alternatives?
If the cough is driving you crazy, don't just stop your meds cold turkey. That can cause your blood pressure to spike dangerously. Talk to your cardiologist or GP about switching to an ARB (Angiotensin II Receptor Blocker).
ARBs, like Losartan or Valsartan, work on the same system but at a different point in the chain. They block the receptors for Angiotensin II rather than stopping the production of the enzyme itself. The best part? They don’t mess with bradykinin. This is why ARBs are often called "ACE inhibitors without the cough."
Studies have shown that switching to an ARB resolves the cough in the vast majority of patients, usually within one to four weeks.
Myths About the ACEI Cough
- "I can just use cough syrup." Nope. Standard over-the-counter antitussives (like dextromethorphan) usually do absolutely nothing for an ACEI-induced cough because the mechanism isn't viral or bacterial. It’s chemical.
- "It will go away if I keep taking it." Rarely. While your body adjusts to many side effects, the ACEI cough tends to persist as long as the drug is in your system.
- "It’s an allergic reaction." Not exactly. It’s a pharmacological side effect. You aren't "allergic" to the drug in the traditional sense; the drug is just doing its job so well that it causes a secondary chemical imbalance in your throat.
Actionable Steps for Management
If you suspect your medication is the culprit, here is exactly how to handle it:
- Track the timing. Start a small log. When did the cough start? Is it worse after your morning dose? Does it happen at night? This data helps your doctor rule out things like acid reflux.
- Don't DIY your dosage. Never cut your pills in half or skip days to try and "lessen" the cough. Blood pressure needs consistency.
- Ask about the "Washout Period." If you switch meds, be aware it can take a few weeks for the bradykinin levels to normalize. Don't expect the cough to vanish five minutes after your first dose of a new drug.
- Hydration and Humidity. While they won't cure the underlying chemical cause, using a humidifier at night can soothe the irritated membranes and make the "tickle" less intense while you work on a medication change.
- Iron Supplements? Some small-scale clinical trials have suggested that iron supplementation might help reduce the severity of ACEI cough by suppressing nitric oxide generation, but this is something you must discuss with a doctor first, as too much iron is toxic.
The bottom line is that you don't have to "just live with it." Modern medicine has plenty of alternatives that protect your heart without making you sound like a lifelong smoker. If you've been asking why does acei cause cough, the answer lies in the complex chemistry of your inflammatory signals. Now that you know the "why," you can have a much more productive conversation with your healthcare provider about finding a treatment plan that actually lets you breathe easy.