If you’ve ever found yourself squinting at an anatomical diagram or frantically googling during a late-night health rabbit hole, you aren’t alone. Honestly, it's kinda wild how much we still don't talk about basic female anatomy. The Skene’s glands are often called the "female prostate," yet most people—including some doctors—can't point to them on a map.
So, where is the Skene gland located? Basically, you’ll find them on the anterior (front) wall of the vagina, right around the lower end of the urethra. Think of the urethra as the tube where pee comes out. The Skene’s glands sit like tiny, twin sentinels on either side of that opening. They aren't huge. In fact, they’re microscopic in some people and slightly larger in others. This variation is why they were "discovered," then ignored, then rediscovered by medical science over the last few centuries.
But there is so much more to it than just a coordinate on a body map.
Mapping the Skene's Glands: Precision Matters
To get technical for a second, the Skene’s glands (also known as the paraurethral glands) are part of a complex network of tissues. They drain into the vestibule, which is the smooth area between the labia minora. If you were to look closely at the urethral opening (the meatus), you might see two tiny pinprick holes. Those are the ducts.
They aren't just floating there. They are embedded in the urethral sponge, a tissue that fills with blood during arousal. This is why the location matters so much for sexual health. When someone talks about the "G-spot," they are essentially talking about the area where the Skene’s glands and the urethral sponge sit. Dr. Alexander Skene, the Scottish gynecologist who "officially" described them in 1880, probably didn't realize he was poking at one of the most debated topics in human pleasure.
Medical history is funny like that. It took until 2002 for the Federative International Committee on Anatomical Terminology to officially rename them the "female prostate." That's a big deal. It acknowledges that these glands share the same embryonic origin as the male prostate.
Why the "Female Prostate" Label Changes Everything
Calling it a prostate isn't just a gimmick. It’s biology. These glands produce Prostate-Specific Antigen (PSA) and prostatic acid phosphatase. If you’ve ever had a lab test and saw "PSA" on it, you likely thought that was only for men. Nope.
🔗 Read more: How Do You Know You Have High Cortisol? The Signs Your Body Is Actually Sending You
Research published in the Journal of Sexual Medicine has shown that the Skene’s glands can actually vary significantly in size and function from person to person. For some, they are highly active; for others, they are barely there. This might explain why some women experience "female ejaculation" (squirting) and others don't. The fluid produced by these glands is chemically very similar to the fluid produced by the male prostate.
It’s about volume and pressure.
When stimulated, the Skene’s glands can swell. If you’re wondering where is the Skene gland located during arousal, it actually moves slightly. The tissue engorges, making the area firmer and more prominent against the vaginal wall. It’s a dynamic part of the body, not a static landmark.
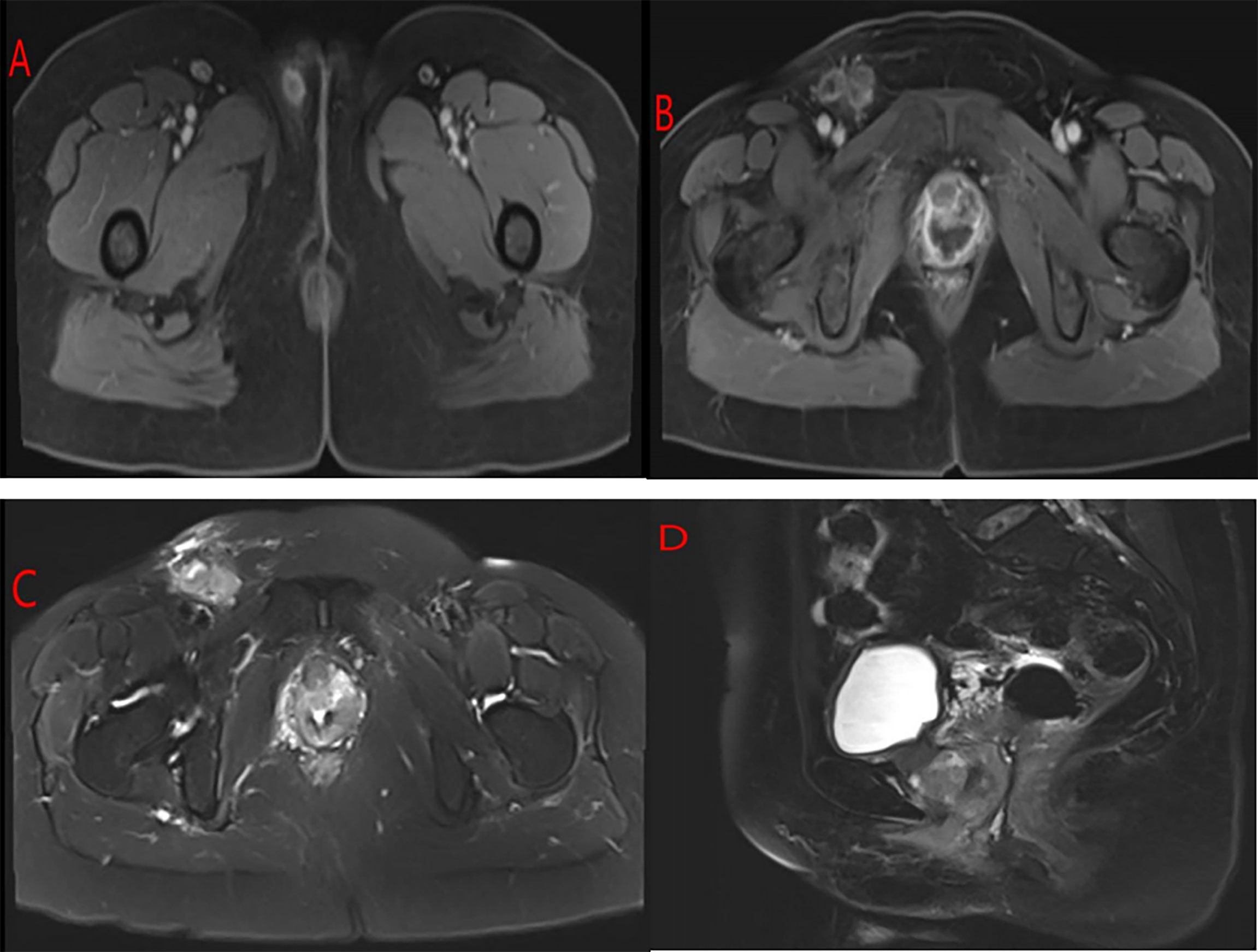
The Problems Nobody Mentions: Skenitis and Cysts
Most people only care about these glands when something goes wrong. And when things go wrong, it's usually painful.
Skenitis is basically an infection or inflammation of these glands. Because of where they sit, it’s often mistaken for a Urinary Tract Infection (UTI). You get that burning sensation, the urgency, the "I feel like I have to pee but I can't" vibe. But if your urine culture comes back clean and you’re still hurting? It might be your Skene’s glands.
Bacteria like E. coli, or even STIs like gonorrhea and chlamydia, can migrate into those tiny ducts. Because the ducts are so small, they can get "plugged."
💡 You might also like: High Protein Vegan Breakfasts: Why Most People Fail and How to Actually Get It Right
This leads to Skene gland cysts.
A cyst here feels like a firm, sometimes tender lump right near the opening of the vagina. It can make walking, sitting, or sex feel like a nightmare. If a cyst becomes infected, it turns into an abscess. Honestly, if you feel a lump in that specific "where is the Skene gland located" zone, don't just wait for it to go away. Doctors often have to drain these or, in chronic cases, surgically remove (excise) the gland entirely.
More Than Just Anatomy: The Pleasure Connection
Let’s talk about the G-spot again. It’s controversial. Some researchers, like Dr. Helen O'Connell—a pioneer in urology—argue that the "G-spot" isn't a single spot at all. Instead, it’s a confluence of the internal clitoris, the urethra, and the Skene’s glands working together.
When you apply pressure to the front wall of the vagina, you are indirectly compressing the Skene’s glands. For many, this is the key to a specific type of orgasm. For others, it just feels like they need to go to the bathroom. Both are totally normal responses because of how close the bladder and urethra are to the glands.
It’s all about the nerves. The pudendal nerve branches out through this entire region. When the Skene’s glands are stimulated, it triggers a cascade of neurological signals that can lead to intense pelvic contractions.
Finding Them Yourself (A Quick Guide)
If you want to find them, you’ve gotta be comfortable with a bit of self-exploration.
📖 Related: Finding the Right Care at Texas Children's Pediatrics Baytown Without the Stress
- Get a mirror. You need to see the urethral opening, which is just above the vaginal opening.
- Look for the "eyes." On either side of the urethra, you might see two tiny depressions. Those are the ducts.
- Feel the "front wall." If you insert a finger into the vagina with your palm facing up (toward your belly button), the Skene’s glands are located just an inch or two inside, behind the pubic bone.
- Note the texture. This area usually feels slightly ridged or "bumpy" compared to the smoother back wall of the vagina.
It isn't always easy. Some people have Skene’s glands that are deeply recessed. Others have ducts that are virtually invisible to the naked eye. Variation is the rule here, not the exception.
The Diagnostic Gap
The real tragedy in women's health is how often Skene-related issues are misdiagnosed. If you go to a GP with pelvic pain, they check for a UTI. If that’s clear, they check for yeast. If that’s clear, they might check for BV.
Rarely does a standard pelvic exam involve "milking" the Skene’s glands to check for discharge or infection.
If you have chronic pressure in the front of the vagina or pain that feels "deep" but is located right near the entrance, you might need to specifically ask your gynecologist: "Can you check my paraurethral glands?"
Experts like Dr. Rachel Rubin, a urologist and sexual medicine specialist, often highlight how "invisible" these glands are in medical school curricula. We spend weeks on the male prostate but barely a mention of its female counterpart. This leaves patients feeling like they’re crazy when they have symptoms that don't fit the "standard" UTI mold.
Actionable Steps for Skene Gland Health
Knowing the answer to where is the Skene gland located is only the first step. You have to know how to take care of them. These aren't just passive structures; they are active, secreting organs.
- Hydration is non-negotiable. Because these glands are so close to the urinary tract, keeping things "flushed" helps prevent bacteria from settling in the ducts.
- Pee after sex. This isn't just for UTIs. The mechanical action of urinating can help clear the Skene’s ducts if they’ve been compressed or exposed to bacteria during activity.
- Gentle hygiene. Avoid harsh soaps. The vestibule area is incredibly sensitive. Use only water or a very mild, pH-balanced cleanser. If you irritate the urethral opening, you risk inflaming the Skene’s ducts.
- Track your symptoms. If you get "UTI symptoms" that only show up after sex or at certain points in your menstrual cycle, it might be hormonal Skenitis. The tissue in these glands is estrogen-sensitive. When estrogen drops (like right before your period or during menopause), the tissue can thin and become more prone to irritation.
- See a specialist. If you have a persistent lump or localized pain, skip the general practitioner and go straight to a urogynecologist. They are the ones who actually deal with the intersection of the urinary and reproductive systems.
The Skene’s glands are a testament to the fact that we are still learning about the human body. They represent pleasure, function, and sometimes a bit of a medical mystery. Whether you call them the female prostate or the paraurethral glands, they deserve a bit more respect—and definitely more than a passing mention in a biology textbook.
If you're dealing with unexplained pelvic discomfort or are simply curious about your body’s potential, start by paying attention to the "front wall." It’s a small area with a massive impact on your quality of life. Understanding your own anatomy is the most basic form of self-advocacy. Don't be afraid to use the right terms and ask the hard questions when you're in the exam room.