You’re sitting in that crinkly paper-covered chair, the cuff tightens until your arm pulses, and the nurse rattles off two numbers. Maybe it’s 122 over 78. They nod, move on, and you’re left wondering: wait, is that actually okay? Most of us grew up hearing that 120/80 is the gold standard, the holy grail of cardiovascular health. But honestly, the "normal" goalpost has moved, and what’s good blood pressure for a 25-year-old athlete isn’t necessarily the same target for an 80-year-old grandmother. It’s complicated.
Actually, it's more than complicated—it’s vital. High blood pressure, or hypertension, is famously called the "silent killer" because it doesn’t usually give you a headache or make you feel dizzy until things are already going south.
💡 You might also like: Eating Your Way to Wholeness: Why Your Relationship With Food Is the Missing Piece
The New Math of Your Heart
The American Heart Association (AHA) and the American College of Cardiology fundamentally changed the game a few years back. They dropped the threshold. Suddenly, millions of people who thought they were "pre-hypertensive" were officially in the high blood pressure club.
What’s good blood pressure today?
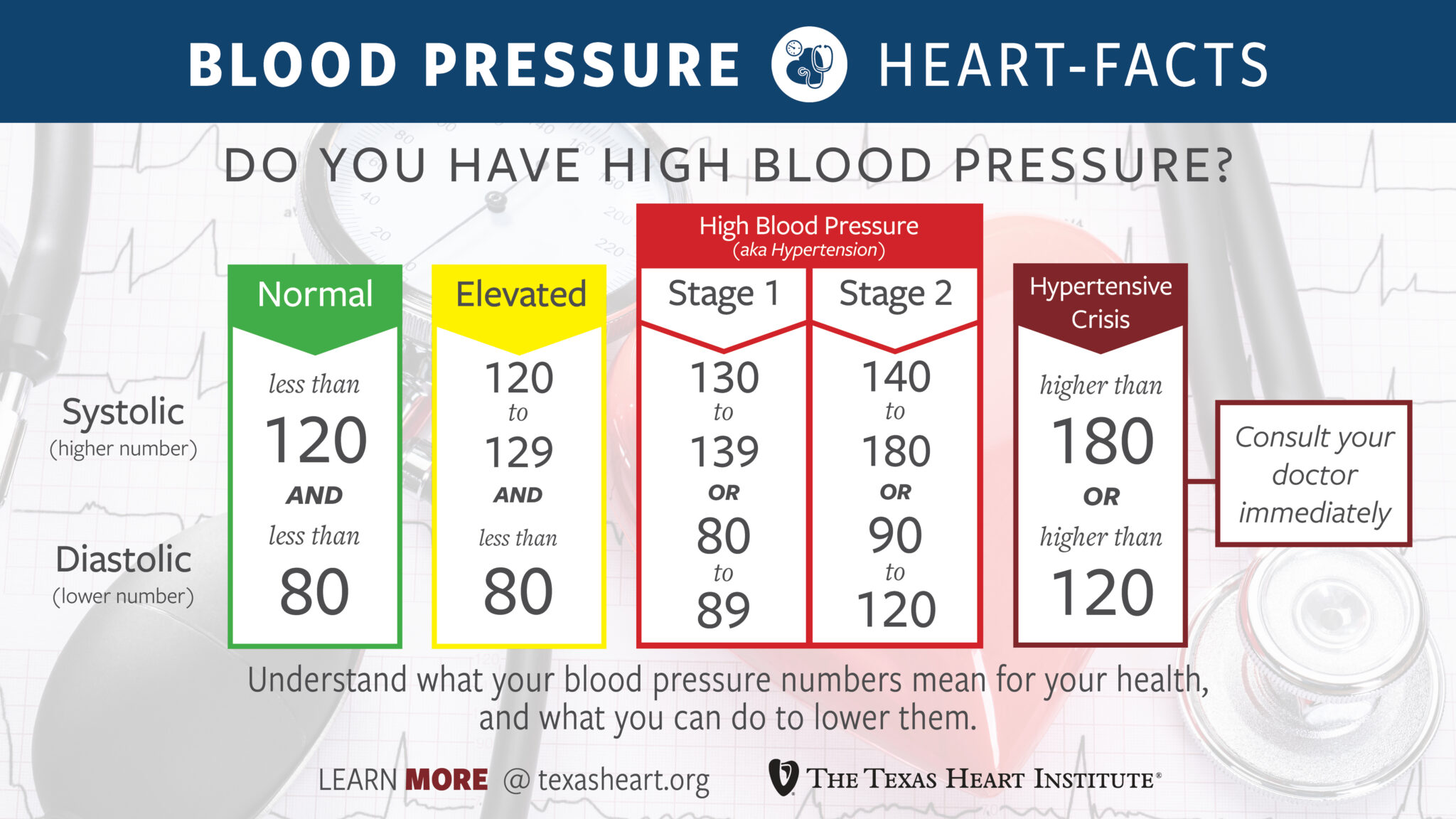
According to current guidelines, "Normal" is strictly less than 120/80 mmHg. If that top number (systolic) hits 120 to 129 while your bottom number (diastolic) stays under 80, you’re officially in the "Elevated" category. This isn't just medical pedantry. It’s a warning shot. Research, including the landmark SPRINT trial (Systolic Blood Pressure Intervention Trial), showed that bringing that top number down to 120 rather than stopping at 140 significantly reduced the risk of heart attacks and death.
But let's be real. If you’re 75 years old and your doctor tries to force your pressure down to 110, you might feel like absolute garbage. You might get dizzy when you stand up and fall. This is where the nuance comes in. For older adults, many geriatricians argue for a slightly more relaxed target—maybe 130/80—to avoid the risks of fainting or kidney stress.
Why those two numbers even exist
Think of your circulatory system like the plumbing in an old house. The systolic pressure (the top number) is the force when the heart is actively pumping. It's the peak of the wave. The diastolic pressure (the bottom number) is the pressure in your pipes when the heart is resting between beats.
Both matter. But for a long time, we obsessed over the bottom number. Now, especially for folks over 50, we know the top number is a way better predictor of stroke and heart disease. As we age, our arteries get stiff. They don’t "bounce" like they used to. This stiffness drives the systolic pressure up while the diastolic might even go down, creating a wide gap called pulse pressure.
The White Coat and the Kitchen Table
Ever noticed your heart racing the second you walk into a doctor’s office? That’s "White Coat Hypertension." Your blood pressure spikes because you’re stressed, maybe you’re running late, or you’re worried about what the doctor will say.
This is why a single reading at the clinic is basically useless for a long-term diagnosis.
To really know what’s good blood pressure for your body, you need home monitoring. Dr. Paul Whelton, a lead author of the AHA guidelines, has often emphasized that home readings are frequently more accurate predictors of future health than clinic readings.
How to actually check it right
Don’t just slap the cuff on over a sweater while you’re checking your email.
✨ Don't miss: Finding pictures of tapeworms in human poop: What you're actually seeing
- Sit still for five minutes first. No talking. No scrolling TikTok.
- Feet flat on the floor. Don’t cross your legs; it can bump your systolic reading by 5 to 10 points.
- Support your arm at heart level.
- Empty your bladder. Seriously—a full bladder can add 10 points to your reading.
If you get a 145/90 reading once, don’t panic. Take it again in two minutes. Record it. It’s the average over a week that tells the real story.
The Lifestyle Myth vs. Reality
We’ve all heard it: eat less salt, go for a walk. It sounds like a cliché because it’s boring, but the data is pretty staggering. The DASH diet (Dietary Approaches to Stop Hypertension) isn't just a trend; it's a clinically proven intervention that can drop your systolic pressure by 11 points. That’s as powerful as some medications.
Potassium is the secret weapon here. Most people obsess over cutting sodium, but they forget to increase potassium. Potassium helps your body flush out sodium and eases the tension in your blood vessel walls. Think bananas, sure, but also avocados, spinach, and white beans.
And then there's alcohol. This is a tough one for many to hear. While a glass of red wine was once touted as "heart healthy," more recent large-scale studies suggest that even moderate drinking can creep those numbers up. If you’re struggling to get your pressure under control, the nightly IPA might be the culprit.
When Meds Become the Move
There’s a weird stigma about blood pressure medication. People feel like they’ve failed if they can't "lifestyle" their way out of a 150/95 reading.
Genetics are a beast. You can be a vegan marathon runner and still have high blood pressure because your kidneys or your blood vessels are just wired that way. Medications like ACE inhibitors, ARBs, or calcium channel blockers aren't "cheating." They are tools to prevent your brain from having a bleed or your kidneys from scarring.
Surprising things that spike your pressure
- Sleep Apnea: If you snore and wake up tired, your blood pressure might be soaring at night when it’s supposed to be dipping. This is a huge, often ignored cause of "resistant" hypertension.
- NSAIDs: Taking Advil or Aleve every day for back pain? These can raise blood pressure and mess with your meds.
- Decongestants: That Sudafed for your cold works by constricting blood vessels—including the ones that aren't in your nose.
- Licorice: Real black licorice (containing glycyrrhizic acid) can actually cause a dangerous spike in pressure.
Looking Beyond the Numbers
What’s good blood pressure is ultimately about "end-organ damage." Doctors don't just care about the numbers; they care about what those numbers are doing to your eyes, your heart muscle, and your brain.
A person with a reading of 135/85 who also has diabetes or chronic kidney disease is at much higher risk than a "healthy" person with the same reading. This is why treatment is now based on a 10-year cardiovascular risk score, not just a static chart on a wall.
📖 Related: The Hip Thrust Machine for Home: Why Your Glutes Probably Need One
Actionable Steps for Better Numbers
If you’re staring at a high reading and feeling the weight of it, don’t spiral. Precision matters more than perfection.
- Buy a validated home monitor. Check ValidateBP.org to make sure the device you’re buying is actually accurate. Many cheap pharmacy-aisle monitors are notoriously finicky.
- The 2-2-2 Rule. Take two readings in the morning and two in the evening for a week. Average them out. This is your "true" baseline.
- Watch the "Salty Six." The AHA identifies bread, cold cuts, pizza, poultry, soup, and sandwiches as the primary hidden sources of sodium in the American diet. It’s rarely the salt shaker; it’s the processed stuff.
- Breathwork. It sounds "woo-woo," but slow, deep breathing for just 5 to 10 minutes a day can physiologically lower your heart rate and settle your nervous system, which in turn lowers the pressure on your vessel walls.
- Get a blood panel. Check your kidney function and your electrolytes. Sometimes high blood pressure is a symptom of something else, like a thyroid issue or an adrenal gland tumor (though that's rare).
Understanding what’s good blood pressure requires looking at your whole life—your age, your stress, your sleep, and your DNA. It isn't a "set it and forget it" metric. It’s a moving target that requires you to be an active participant in your own longevity. Stop chasing 120/80 as a perfectionist goal and start viewing it as a conversation between you and your cardiovascular system.