You’re sitting in that small, sterile exam room. The nurse wraps a velcro cuff around your arm, pumps it up until it pinches, and then lets the air hiss out. You hear a couple of numbers—maybe 134 over 86—and they move on to the next thing. But what does that actually mean for your heart? Knowing what’s a good blood pressure reading isn’t just about memorizing two numbers; it’s about understanding the pressure your blood exerts against your artery walls every single time your heart beats. It’s basically the plumbing of your body, and if the pressure stays too high for too long, the pipes start to give way.
The Magic Number: 120/80 and Why it Matters
For decades, the gold standard has been 120/80 mmHg. If you’re at or below this, you’re usually in the clear. But here is where it gets kinda tricky. The American Heart Association (AHA) and the American College of Cardiology updated their guidelines a few years back, and they got a lot stricter. They did this because research, like the landmark SPRINT trial (Systolic Blood Pressure Intervention Trial), showed that bringing that top number down even further could significantly lower the risk of heart attacks and strokes.
So, what’s a good blood pressure reading today? Most experts want to see you under 120/80 mmHg.
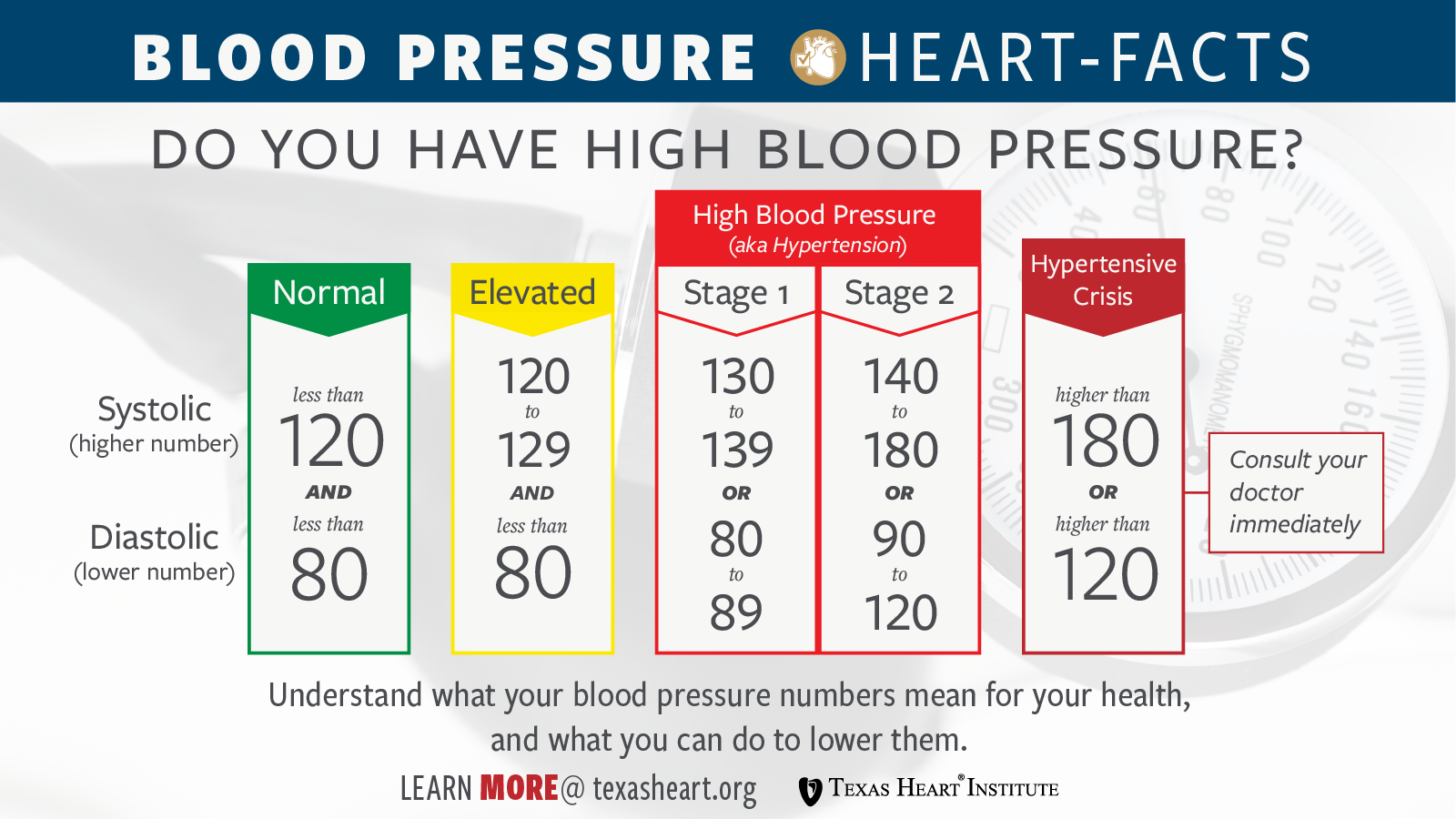
If that top number, the systolic pressure, creeps up to 120–129 while your bottom number stays under 80, you aren’t "hypertensive" yet, but you’re in the "Elevated" category. This is basically a yellow light. It’s your body’s way of saying, "Hey, maybe cut back on the salt and start taking the stairs." It is not a crisis, but it is a signal.
Decoding the Two Numbers
The top number is the systolic pressure. It measures the force when your heart beats. The bottom number is the diastolic pressure, which measures the pressure in your arteries when your heart rests between beats.
Both matter.
🔗 Read more: That Time a Doctor With Measles Treating Kids Sparked a Massive Health Crisis
Sometimes people have what’s called "Isolated Systolic Hypertension," where only the top number is high. This is super common in older adults because arteries tend to stiffen as we age. When the arteries lose their "bounce," the pressure spikes every time the heart pumps blood through them. If you’re wondering why your doctor is obsessing over a 145/78 reading, that’s why. That 145 is hammering away at your blood vessels.
When the Numbers Turn Red: Stages of Hypertension
Honestly, the terminology can be confusing. Let’s break down the actual stages doctors use to diagnose high blood pressure.
Stage 1 Hypertension kicks in when your systolic is between 130–139 or your diastolic is between 80–89. At this point, a doctor might not put you on meds immediately, especially if your overall cardiovascular risk is low. They might suggest "therapeutic lifestyle changes"—which is just doctor-speak for eating better and moving more.
Stage 2 Hypertension is when you hit 140/90 or higher. This is usually the threshold where medication enters the conversation.
Then there is the scary one: Hypertensive Crisis. If your reading suddenly hits 180/120 or higher, stop reading this and call a doctor. Seriously. If you have chest pain, shortness of breath, or vision changes with a reading that high, it’s an emergency. Your organs are literally under too much pressure to function safely.
💡 You might also like: Dr. Sharon Vila Wright: What You Should Know About the Houston OB-GYN
The "White Coat" Factor and Home Monitoring
You’ve probably heard of "White Coat Hypertension." It’s real. Some people get so stressed out just being in a doctor’s office that their blood pressure spikes 20 points the second they see a stethoscope.
Because of this, a single reading in a clinic is rarely enough for a diagnosis.
Many cardiologists, like those at the Mayo Clinic, now push for home monitoring. But you can't just slap a cuff on over your sweater and expect it to be right. To get a real sense of what’s a good blood pressure reading for you, you need to be consistent. Sit still for five minutes before taking a measurement. Keep your feet flat on the floor. Don’t cross your legs. Don’t talk. Even a full bladder can artificially inflate your blood pressure by 10 to 15 points.
Salt, Stress, and the Silent Killer
High blood pressure is famously called the "silent killer" because it rarely has symptoms. You could be walking around with 160/100 and feel totally fine. You might even feel energetic. But inside, that pressure is creating tiny tears in your artery walls. Your body tries to fix these tears with plaque, which eventually leads to clogs.
Diet is a massive lever here. The DASH diet (Dietary Approaches to Stop Hypertension) isn't just a fad; it's one of the most researched eating plans in medical history. It focuses on potassium, calcium, and magnesium, which help blood vessels relax.
📖 Related: Why Meditation for Emotional Numbness is Harder (and Better) Than You Think
Potassium is the big one. It acts as a counterbalance to sodium. While sodium makes your body hold onto water (increasing blood volume and pressure), potassium helps your kidneys flush that extra salt out. Bananas are the classic example, but spinach, sweet potatoes, and beans actually pack more of a punch.
Age and Nuance: Is 120/80 Right for Everyone?
There is a bit of a debate in the medical community about whether elderly patients should be held to the same strict standards as 30-year-olds. Some doctors argue that if you’re 85, a slightly higher pressure—say 135/85—might actually be safer to prevent falls. If blood pressure is pushed too low with medication, older adults can get dizzy when they stand up (orthostatic hypotension), which leads to hip fractures.
Context is everything. Your "good" reading might be slightly different than your neighbor's depending on your history of diabetes, kidney disease, or heart failure.
Actionable Steps to Improve Your Numbers
If your numbers aren't where you want them to be, don't panic. Blood pressure is incredibly responsive to lifestyle changes.
- Buy a validated home monitor. Look for one that is "clinically validated." Brands like Omron are usually reliable, but check the ValidateBP.org list to be sure your model is accurate.
- Watch the "Salty Six." The AHA identifies bread, cold cuts, pizza, poultry, soup, and sandwiches as the biggest sources of hidden sodium in the American diet. You don't have to quit them, but being aware of the labels helps.
- The 150-minute rule. Aim for 150 minutes of moderate-intensity aerobic activity per week. This strengthens your heart so it can pump more blood with less effort, which naturally lowers the force on your arteries.
- Limit alcohol. This one is a bummer for some, but more than one or two drinks a day can directly raise blood pressure levels.
- Track your trends. One high reading is a fluke. A week of high readings is a pattern. Keep a log—either on paper or in an app—to show your doctor at your next visit.
Understanding what’s a good blood pressure reading is the first step in taking control of your long-term health. It’s not about being perfect; it’s about keeping those numbers in a range where your heart doesn't have to work harder than it should.