You’re staring at the bathroom tiles, wondering if that shrimp taco was really worth this misery. It’s a familiar, frantic desperation. When your stomach starts doing backflips and the cold sweats kick in, the first instinct is to grab literally anything that might stop the carnage. But honestly? Most people reach for the wrong thing. Knowing what to take if you have food poisoning isn't just about stopping the symptoms; it's about making sure you don't accidentally trap the bacteria inside your system for longer than necessary.
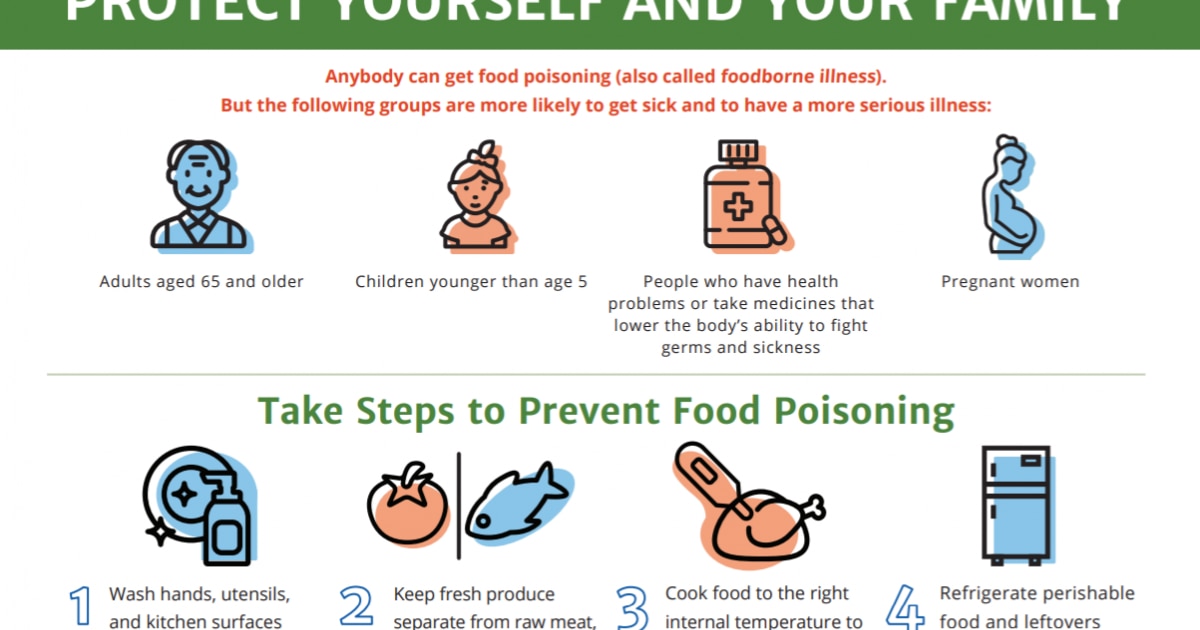
It’s brutal. One minute you’re enjoying dinner, and the next, your body is staging a full-scale evacuation. Most foodborne illnesses are caused by common culprits like Salmonella, E. coli, Listeria, or the infamous Norovirus. According to data from the Centers for Disease Control and Prevention (CDC), about 48 million people get sick from contaminated food every year in the United States alone. That’s 1 in 6 people. You aren't alone, even if you feel like you're dying on your bathroom floor right now.
The Big Mistake: Anti-Diarrheals
Here is the thing nobody wants to hear: diarrhea is actually your body’s way of "flushing the pipes." When you have food poisoning, your intestines are trying to get rid of toxins or pathogens as fast as possible. If you immediately take something like loperamide (brand name Imodium), you’re essentially putting a cork in a volcano.
It stops the flow, sure. But it also keeps the shigella or C. diff or whatever nasty bug you ate inside your colon for an extra 24 to 48 hours. That can lead to more severe inflammation or even something dangerous like toxic megacolon. Dr. Frank Esper, an infectious disease specialist at Cleveland Clinic, often points out that while these meds are great for "runner's trots" or nervous stomachs, they can be risky when an actual infection is present. If you see blood in your stool or have a high fever, stay far away from the Imodium.
If you absolutely must take something because you have to get on a plane or attend a funeral (though, please, stay home), bismuth subsalicylate (Pepto-Bismol) is usually a slightly safer bet. It has mild antibacterial properties and doesn't paralyze your gut quite as aggressively as loperamide.
What to Take for Rehydration (The Real MVP)
Dehydration is what actually lands people in the ER. It isn't the bacteria; it's the loss of fluids. But chugging plain water isn't always the answer. When you’re vomiting, you aren't just losing water; you’re losing potassium, sodium, and chloride.
🔗 Read more: Baldwin Building Rochester Minnesota: What Most People Get Wrong
Skip the sugary sports drinks if you can. They are often too high in sugar, which can actually draw more water into the gut and make diarrhea worse. It's a cruel irony. Instead, look for Oral Rehydration Salts (ORS). The World Health Organization (WHO) has a specific formula that is basically a "magic" ratio of salt and sugar that helps the small intestine absorb water more efficiently via the sodium-glucose cotransport mechanism.
- Pedialyte or store-brand equivalents are great for adults, not just kids.
- Hydralyte or Liquid I.V. (though watch the sugar content on some flavors).
- Homemade ORS: In a pinch, mix six level teaspoons of sugar and a half teaspoon of salt into one liter of clean water. It tastes kind of like sweat, but it works.
Drink in tiny sips. Like, teaspoon-sized sips. If you gulp a whole glass of water, your irritated stomach lining will likely just reject it immediately. Patience is a virtue you probably don't have right now, but you need it.
Natural Remedies That Actually Work
Ginger is legit. There’s a reason your mom gave you ginger ale, though the modern stuff barely has any real ginger in it. Research published in the journal Foods confirms that gingerols and shogaols in ginger can speed up gastric emptying and reduce the "heave" reflex. If you can handle it, steep fresh ginger in hot water.
Activated charcoal is a controversial one. Some swear by it for "soaking up" toxins. While it is used in hospitals for specific types of poisoning (like drug overdoses), the evidence for it helping with a standard case of Salmonella is a bit thin. It won't hurt most people, but it will turn your stool black, which can be terrifying if you aren't expecting it.
When Do You Need Antibiotics?
Most food poisoning is viral (hello, Norovirus) or clears up on its own before an antibiotic would even kick in. Taking Cipro or Z-Paks for a viral infection just kills off your "good" gut bacteria and leaves the door open for C. difficile to move in and cause a whole new world of pain.
💡 You might also like: How to Use Kegel Balls: What Most People Get Wrong About Pelvic Floor Training
However, if you have a confirmed case of Campylobacter or a severe parasitic infection like Giardia, a doctor might prescribe something. The Mayo Clinic generally advises seeing a professional if:
- Your fever is over 102°F (39°C).
- You have bloody stools (this is a major red flag).
- You can't keep any liquids down for more than 12 hours.
- You show signs of severe dehydration, like dark urine or extreme dizziness.
Probiotics: Timing is Everything
Don't bother taking probiotics while you’re actively vomiting. It’s a waste of money. They’ll be gone before they can do anything. The time for probiotics is the "recovery phase."
Once the worst is over, your gut microbiome is a ghost town. This is when Saccharomyces boulardii (a beneficial yeast) or Lactobacillus rhamnosus GG can help. Studies suggest these specific strains can shorten the duration of post-infectious diarrhea by about a day. It helps reset the balance so you don't end up with "post-infectious IBS," which is a real thing that can linger for months.
What to Eat (and When to Start)
The old BRAT diet (Bananas, Rice, Applesauce, Toast) is a bit outdated, but the core logic holds up. You want low-fiber, bland foods. Why? Because fiber is hard to digest. Your gut is currently like a raw, sunburned patch of skin. You wouldn't scrub a sunburn with a loofah, so don't scrub your gut with kale or whole-grain bread right now.
Wait until you feel a genuine "spark" of hunger. That’s your body signaling that the stomach lining has repaired itself enough to handle hydrochloric acid again. Start with saltine crackers or a little bit of plain white rice. Avoid dairy like the plague. Even if you aren't lactose intolerant, food poisoning often causes a temporary deficiency in the enzyme lactase. Drinking milk right after food poisoning is a fast track to more bloating and gas.
📖 Related: Fruits that are good to lose weight: What you’re actually missing
Surprising Culprits: It’s Not Always the Meat
When we think about what to take if you have food poisoning, we usually blame the undercooked burger. But keep an eye on your produce. Leafy greens, sprouts, and even pre-cut melons are frequent flyers on the FDA recall lists. In fact, raw flour and unwashed lettuce cause just as many outbreaks as chicken these days.
If you suspect your illness came from a specific restaurant or product, keep the packaging or the receipt. It sounds litigious, but it’s actually for public health. Local health departments rely on these reports to spot outbreaks before they kill someone vulnerable, like an elderly person or a child.
Immediate Action Plan
If you’re currently in the thick of it, here is your roadmap:
- Stop Eating: Give your digestive system a total break for at least a few hours.
- The Sip Test: Take one teaspoon of an oral rehydration solution every 5 to 10 minutes. If it stays down for an hour, move up to two tablespoons.
- Check Your Temp: If you’re running a high fever or seeing blood, call a doctor. Don't "tough it out."
- Acetaminophen over NSAIDs: If you have a headache or body aches, reach for Tylenol (acetaminophen). Ibuprofen or Aspirin can be very hard on an already irritated stomach lining.
- Rest: Your immune system is doing a lot of heavy lifting. Don't try to work through this.
The goal isn't just to stop the bathroom trips; it's to support your body while it does the dirty work of cleaning itself out. Stay hydrated, stay near a toilet, and give it time. Most cases resolve within 24 to 48 hours. If you're still miserable after day three, it's time to get a stool sample done to see exactly what you're dealing with.