Honestly, most of the health world is obsessed with lowering blood pressure. We hear about salt being the enemy and HIIT workouts being the savior every single day. But for a specific group of people, the problem is the exact opposite. You stand up too fast, the room starts spinning, and suddenly you’re gripping the nearest bookshelf just to stay upright. If you've ever felt like your brain is operating through a fog or your energy levels are permanently stuck in the basement, you’re likely hunting for what to do to get blood pressure up without making yourself unhealthy in other ways.
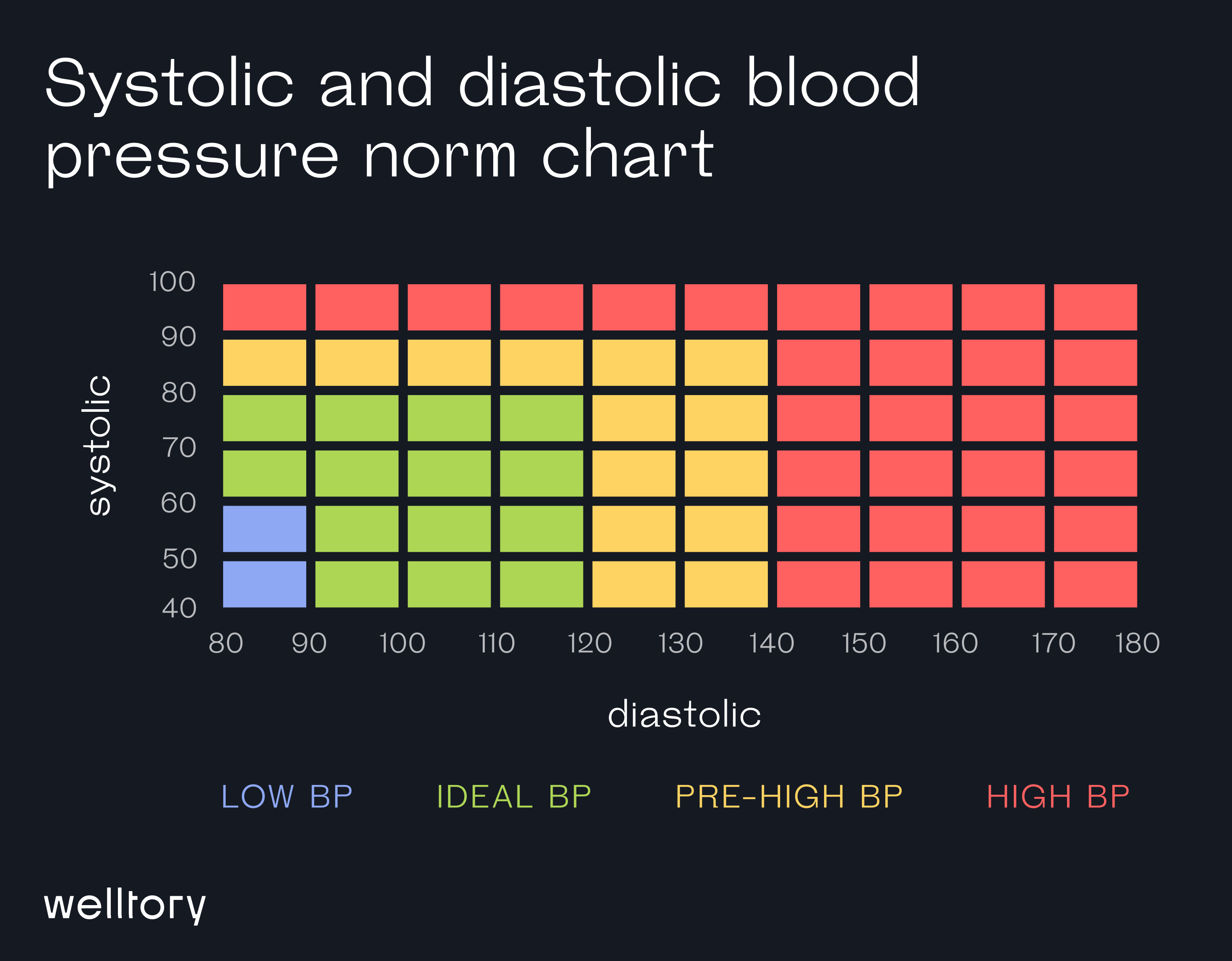
Low blood pressure, or hypotension, isn't always a "good" problem to have. While a reading of $90/60$ mmHg is technically the cutoff, the numbers matter way less than how you actually feel. If you're asymptomatic, doctors usually don't care. But if you're fatigued, dizzy, or fainting? That’s a different story entirely.
📖 Related: Express Care Sikeston MO: What Most People Get Wrong About Urgent Care
The salt "taboo" and why it matters now
Forget everything you’ve heard about low-sodium diets for a second. If your pressure is bottoming out, salt is actually your best friend. Sodium holds onto water in your bloodstream. More water means more blood volume. More blood volume means higher pressure. It’s basic physics.
Most people with hypotension find that adding a little extra high-quality sea salt to their meals—or even drinking a glass of water with a pinch of salt and a squeeze of lemon—can provide an almost immediate lift. You aren't looking to develop a processed food habit, but you do need that electrolyte balance to shift. According to the Mayo Clinic, increasing sodium intake is a standard first-line recommendation for orthostatic hypotension, which is that specific "head rush" you get when changing positions.
Don't just dump table salt on everything, though. Try adding olives, pickles, or salted nuts to your day. It’s about consistent intake rather than one massive salt bomb that just leaves you feeling bloated and thirsty.
Hydration is about volume, not just thirst
You’ve heard it a million times: drink more water. But for someone trying to figure out what to do to get blood pressure up, water is literally the fuel for your circulatory system. When you’re dehydrated, your blood volume drops. When blood volume drops, your heart has to work harder to push a smaller amount of liquid through your pipes.
It's a struggle.
Try to aim for a consistent sipping schedule. If you chug a liter of water and then don't drink for four hours, your kidneys will just flush most of it out. You want a steady stream. Interestingly, some studies, including research published in the journal Circulation, suggest that drinking about $500$ ml (roughly two cups) of plain water can acutely raise systolic blood pressure in older adults with autonomic failure by more than $30$ mmHg. That is a massive jump just from a glass of water.
📖 Related: Female Lungs Back View: What Anatomical Models Often Get Wrong
The role of compression gear
It sounds like something your grandmother would wear, but compression stockings are actually a secret weapon. They prevent blood from pooling in your legs. When you stand up, gravity tries to yank your blood toward your feet. If your veins aren't snappy enough to push it back up, your brain loses out on oxygen.
That’s why you feel dizzy.
Modern compression socks actually look like normal athletic gear now. You want "gradient" compression, usually starting around $15-20$ mmHg or $20-30$ mmHg if your doctor okays it. By squeezing the legs, these garments help the "skeletal muscle pump" return blood to the heart. It’s an external fix for an internal sluggishness.
Changing how you move and eat
Ever noticed how you feel worse after a huge Thanksgiving-style meal? There’s a reason for that. It’s called postprandial hypotension. When you eat a massive, carb-heavy meal, your body sends a huge percentage of its blood supply to your digestive tract to handle the load. This leaves the rest of your body—including your brain—scrambling for what's left.
- Switch to smaller, more frequent meals. Instead of three big ones, try five small ones.
- Cut back on highly refined carbohydrates like white bread and sugary cereals, which can cause a sharper drop in pressure after eating.
- Keep a snack nearby that has a bit of protein and salt.
Move slowly. Seriously. If you’re lying in bed, sit up first. Wait thirty seconds. Then swing your legs over the side. Wait another thirty seconds. Then stand up. It gives your baroreceptors—the little sensors in your neck and heart that monitor pressure—a chance to wake up and do their job.
When it’s more than just a head rush
Sometimes, knowing what to do to get blood pressure up requires a trip to the pharmacy or a specialist. If lifestyle changes like salt, water, and socks don't work, there are medications like Fludrocortisone or Midodrine. Fludrocortisone helps your kidneys hang onto sodium, while Midodrine works by narrowing the blood vessels to keep pressure higher.
But meds are the last resort.
You also need to look at what you’re already taking. A lot of people don't realize that certain antidepressants, anti-anxiety meds, or even some OTC painkillers can inadvertently lower blood pressure. It’s worth doing a "medicine cabinet audit" with a professional.
Why your "normal" might be low
Some people are just built this way. Athletes often have lower resting blood pressure because their hearts are incredibly efficient. That’s fine. The problem arises when the low pressure interferes with your quality of life. If you're constantly cold, tired, and feeling like you're about to faint, your "normal" isn't healthy for you.
Actionable steps for immediate relief
If you're feeling a dip right now, don't just sit there. There are physical maneuvers that can help.
- Leg crossing: If you're standing and feel dizzy, cross your legs in a scissor fashion and squeeze your thigh muscles. This pushes blood upward.
- The "Whole Body Squeeze": Clench your fists and tense your arm muscles. It creates a temporary spike in peripheral resistance.
- Elevate the head of your bed: Using a few bricks or a foam wedge to raise the head of your bed by about $10$ to $20$ degrees can actually help your body adjust to the "upright" position while you sleep, making that first step out of bed in the morning less jarring.
Licorice root is another interesting one. Real licorice (not the strawberry candy) contains glycyrrhizic acid, which can raise blood pressure by affecting how the kidneys handle cortisol. It’s potent stuff, though, so you shouldn't mess with it without talking to a doctor, especially if you have any history of kidney issues.
Summary of next steps
Start tracking your symptoms alongside your salt and water intake. Often, the "brain fog" people attribute to stress or lack of sleep is actually just a mild case of low blood pressure.
What to do next:
- Increase daily fluid intake to at least $2-3$ liters unless told otherwise by a doctor.
- Add an extra half-teaspoon of salt to your food throughout the day and observe if the "dizzy spells" decrease.
- Purchase a pair of $15-20$ mmHg compression socks to wear during the day, especially if you stand for long periods.
- Schedule a "poor man's tilt table test" at home: Measure your blood pressure while lying down, then again after standing for three minutes. If the systolic (top number) drops by $20$ points or the diastolic (bottom number) drops by $10$, you have a clear clinical indicator to show your doctor.