You’ve probably heard it a thousand times since grade school. Sixty to one hundred. That’s the "magic" range everyone points to when you ask what should be pulse rate. If you’re sitting on the couch and your fitness tracker buzzes with a 72, you feel fine. You're "normal." But honestly, that range is a bit like saying a "normal" shoe size is between a 5 and a 13. It’s technically true for the vast majority of the population, but it doesn't tell you if the shoe actually fits your foot.
Your heart isn't a metronome. It’s a reactive, living pump that responds to everything from that third cup of coffee to the stressful email you just got from your boss. When we talk about pulse rate, we're really talking about your heart’s efficiency.
The Basics of the 60 to 100 Range
The American Heart Association maintains that a resting heart rate for adults typically falls between 60 and 100 beats per minute (BPM). If you’re at 65, great. If you’re at 95, you’re still "in range," but doctors might start squinting at your charts. Why the gap? Because a pulse of 95 while sitting perfectly still is a lot of work for a muscle that never gets a day off. Think about it this way: a car idling at 3,000 RPMs is "running," but it's burning way more fuel than it needs to.
Research, including the landmark Copenhagen City Heart Study, has suggested that people with resting heart rates on the higher end of that "normal" scale—specifically above 80 BPM—might actually face higher risks of cardiovascular issues compared to those in the 50s or 60s. So, while 90 is "fine" by the textbook, it might not be optimal for long-term health.
Why "Low" Isn't Always Scary
Then there are the outliers. You’ve got the marathon runners and the cyclists whose hearts are so powerful they only need to beat 40 times a minute to move the same amount of blood that takes a sedentary person 80 beats. This is called bradycardia. In a fit athlete, it's a badge of honor. In an elderly person feeling dizzy, it’s a medical red flag.
Context is everything. You can't just look at the number in a vacuum. If your pulse is 48 but you feel energetic and sharp, your heart is likely just very efficient. But if you’re hitting 48 and feeling like you’re about to faint every time you stand up, your "what should be pulse rate" answer is "higher than it is right now."
Factors That Mess With Your Numbers
Life happens. Your pulse rate isn't a static setting like the clock on your microwave. It’s fluid.
Temperature and Humidity
When the air gets hot and sticky, your heart has to work harder. It pumps more blood to the surface of your skin to help heat escape. You might see your resting pulse jump by 5 or 10 beats just because the AC is broken. It’s a temporary spike, but it's real.
Dehydration
This is a big one people miss. When you’re dehydrated, the total volume of blood in your body actually drops. To keep your blood pressure stable and get oxygen to your brain, your heart has to beat faster. It’s compensating for the lack of fluid. If you notice your heart racing for no reason, go drink a glass of water before you panic.
📖 Related: Why the 45 degree angle bench is the missing link for your upper chest
Emotions and Stress
The "fight or flight" response is a cliché for a reason. Stress triggers adrenaline and cortisol. These hormones tell your heart to gear up for a fight. Even if that "fight" is just an annoying person in traffic, your body doesn't know the difference. Your pulse will climb.
Medications
Beta-blockers, often prescribed for high blood pressure, are designed to slow the heart down. On the flip side, some asthma inhalers or decongestants can send your pulse soaring. Always check the labels.
How to Actually Measure It
Don’t trust a single reading from your watch after you just walked up a flight of stairs. That’s not your resting heart rate; that’s your "I just did something" rate.
To find out what your pulse rate should be at rest, you need to be truly at rest. The best time is the very second you wake up, before you even sit up to reach for your phone. Lay there. Breathe normally.
- Use your index and middle fingers (not your thumb, it has its own pulse!).
- Place them on the thumb side of your wrist or the side of your neck.
- Count the beats for 30 seconds and multiply by two. Or 15 seconds and multiply by four.
If you use a wearable like an Apple Watch or a Garmin, look at the "Resting Heart Rate" trend over a week, not the "Current Heart Rate" while you're talking or moving. Trends matter way more than snapshots.
When Should You Actually Worry?
We spend a lot of time obsessing over numbers, but the body usually tells you when something is wrong through symptoms, not just digits.
Tachycardia is the medical term for a heart rate over 100 BPM at rest. If you’re just sitting there watching TV and your heart is hammering at 110, that’s a problem. It could be an underlying thyroid issue, an arrhythmia like AFib, or just extreme anxiety.
Conversely, if you aren't an elite athlete and your heart rate is consistently dipping into the 40s, you might not be getting enough oxygenated blood to your organs.
👉 See also: The Truth Behind RFK Autism Destroys Families Claims and the Science of Neurodiversity
The Red Flags:
- Palpitations (feeling like your heart is skipping a beat or "flopping").
- Shortness of breath when doing minor tasks.
- Chest pain or tightness.
- Fainting spells (syncope).
If your pulse is "off" and you have any of those, stop Googling and go see a professional.
Age and Your Pulse
Your "what should be pulse rate" targets change as you grow. Newborns have incredibly fast hearts, sometimes up to 150 BPM. As kids grow, their hearts get bigger and stronger, and the rate slows down. By the time you hit adulthood, it levels off.
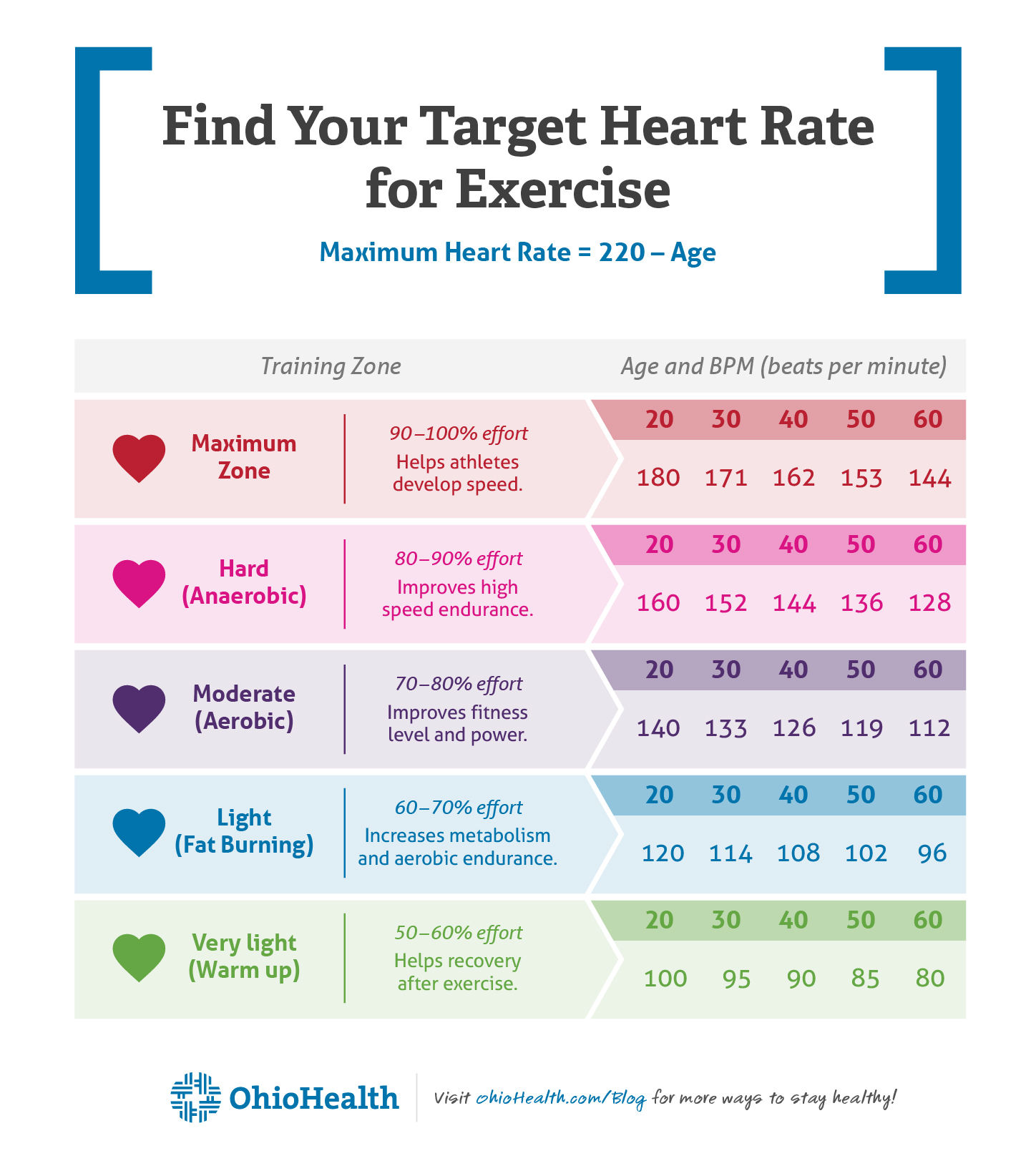
Interestingly, while resting heart rate stays somewhat stable as you age, your maximum heart rate drops. The old formula $(220 - \text{age})$ is a rough estimate for how fast your heart can safely go during intense exercise. So a 20-year-old can hit 200 BPM during a sprint, but a 60-year-old shouldn't really be pushing past 160.
The Link Between Pulse and Longevity
There's a fascinating, slightly morbid theory in biology called the "Heartbeat Hypothesis." The idea is that every mammal has a finite number of heartbeats in a lifetime—roughly 2.5 billion for humans. While it's not a hard-and-fast law, the data does show that mammals with slower heart rates (like whales and elephants) tend to live much longer than those with rapid pulses (like shrews or hummingbirds).
Lowering your resting heart rate through cardiovascular exercise is essentially "saving" beats for later. When you strengthen your heart muscle, it becomes more efficient. It pumps more blood per "stroke," allowing it to rest longer between beats.
Actionable Steps to Optimize Your Rate
If you’ve checked your pulse and realized it’s a bit higher than you’d like—say, consistently in the 80s or 90s—you aren't stuck there. You can train your heart to slow down.
Interval Training
You don't need to run for hours. Short bursts of high-intensity movement followed by rest periods teach your heart how to recover quickly. The faster your heart rate drops back to normal after exercise, the healthier your cardiovascular system is.
✨ Don't miss: Medicine Ball Set With Rack: What Your Home Gym Is Actually Missing
Magnesium and Potassium
These electrolytes are vital for the electrical signals that tell your heart to beat. If you're low on them, you might experience "skipped" beats or a racing pulse. Spinach, bananas, and avocados are your friends here.
Sleep Hygiene
Your heart rate drops to its lowest point during deep sleep. If you’re only getting four or five hours of restless shut-eye, your heart never gets its recovery period. This keeps your baseline "resting" rate higher during the day because your body is essentially in a state of low-level chronic stress.
Vagus Nerve Stimulation
Simple breathing exercises, specifically those where your exhale is longer than your inhale, stimulate the vagus nerve. This nerve acts as a brake for your heart. Try the 4-7-8 technique: inhale for 4, hold for 7, exhale for 8. You can actually watch your pulse drop on a monitor in real-time doing this.
Reality Check
Honestly, don't get too caught up in being "perfect." If you had a rough night, your pulse will be up. If you're fighting off a cold, your pulse will be up. It's a dashboard light, not the whole engine.
The goal isn't to hit a specific number because a TikTok influencer said so. The goal is to know your baseline so well that you notice when it changes. A sudden, unexplained jump in your average resting heart rate over three or four days is often the first sign that you're getting sick, even before you feel a sniffle.
Next Steps for Better Heart Health
Start by tracking your resting pulse for five consecutive days. Use the manual method first thing in the morning to get an accurate baseline. If your average is consistently above 85 BPM and you aren't currently active, incorporate 20 minutes of zone 2 cardio—walking at a pace where you can still hold a conversation—three times a week.
Check your caffeine and nicotine intake. Both are direct stimulants that can artificially inflate your pulse for hours. If you're seeing numbers that worry you, keep a simple log of your pulse alongside what you ate or how you felt that day to bring to your next physical. This gives your doctor actual data to work with rather than just a single, potentially anxious reading in a cold exam room.