You’re sitting on the couch, half-watching a Netflix documentary, and you glance down at your wrist. Your watch says 74. Or maybe 82. Suddenly, you’re wondering if that’s okay. Most of us go through our lives without thinking about our hearts until a piece of plastic and glass tells us to worry. But honestly, the question of what pulse rate is normal isn’t as straightforward as a single number on a screen.
Heart rate is basically just a measurement of how many times your heart beats in a minute. Simple, right? Except it’s not. It’s a shifting, breathing metric that reacts to the coffee you drank three hours ago, that annoying email from your boss, and even how hydrated you are. The American Heart Association (AHA) generally says a normal resting heart rate for adults is between 60 and 100 beats per minute (bpm). But if you’re an athlete, you might sit at 45. If you’re stressed, you might be at 105.
The 60 to 100 Range is Kind of Arbitrary
Let’s be real. The "60 to 100" range is a wide net. It’s designed to catch the majority of the population, but it doesn't always account for individual health. Many cardiologists, including those at the Mayo Clinic, have noted that a resting heart rate on the lower end—usually under 80 bpm—is often a sign of better cardiovascular fitness and more efficient heart function.
If your heart is strong, it pumps more blood with every squeeze. It doesn't have to work as hard. That’s why a marathon runner might have a resting pulse of 40 bpm and feel perfectly fine, while a sedentary person with that same number might feel dizzy or faint. This is called bradycardia. It sounds scary, but it’s often just a sign of a very "athletic" heart. On the flip side, if you're consistently sitting at 95 or 100 while watching TV, your heart is working a lot harder than it probably needs to.
What Pulse Rate Is Normal When You Aren’t Just Sitting There?
The moment you stand up, your heart rate changes. This is normal. Your body has to fight gravity to get blood up to your brain. If we’re talking about "active" heart rates, the math changes completely.
For exercise, experts usually point to the formula of 220 minus your age to find your maximum heart rate. If you’re 40, your max is roughly 180. During moderate-intensity exercise, you want to be at about 50% to 70% of that max. For a 40-year-old, that’s roughly 90 to 126 bpm. It’s a range. Not a rule.
✨ Don't miss: Is there a cure to the black plague? What medicine actually does today
There is a condition called POTS (Postural Orthostatic Tachycardia Syndrome) that has gained a lot of attention recently, especially in the wake of long-COVID discussions. People with POTS see their heart rate jump by 30 bpm or more just by standing up. For them, "normal" is a moving target that causes significant physical distress. It highlights the fact that context matters more than the raw data on your watch.
Why Your Morning Coffee Matters More Than You Think
We need to talk about variables. Your pulse isn't a static setting like the cruise control on a car. It’s more like the gas pedal.
- Caffeine and Nicotine: These are stimulants. They kick your nervous system into gear. If you’ve just had a double espresso, don’t expect your heart rate to be at its "normal" baseline.
- Dehydration: When you’re low on fluids, your blood volume drops. Your heart has to beat faster to move what’s left around your body. It’s a mechanical response to a lack of fuel.
- Temperature: If it’s 95 degrees outside and humid, your heart is working overtime to pump blood to your skin to cool you down.
- Emotions: Anxiety is a physical event. A panic attack can send a pulse from 70 to 130 in seconds. The heart is fine; the brain is just sending a "false alarm" signal.
The Age Factor: From Infants to Seniors
A newborn’s heart rate is incredibly fast, often between 100 and 160 bpm. It’s wild to think about, but their little systems are burning through energy at a massive rate. As we age, these numbers settle down. By the time a child is 10, they usually fall into that adult range of 60 to 100.
Interestingly, as we get into our 70s and 80s, the heart's "max" capacity tends to decrease. The electrical pathways in the heart can slightly degrade or slow down. This is why many seniors might find their pulse sits a bit lower, or why they might feel winded more easily during exertion—the heart simply can't "rev" as high as it used to.
When Should You Actually Be Concerned?
A lot of people obsess over "ectopic beats"—that feeling where your heart "skips" or "flips." Usually, these are PVCs (Premature Ventricular Contractions). Most of the time, they are harmless. They happen to everyone, but we only notice them when we’re stressed or lying still in bed.
However, there are red flags. If your pulse is consistently over 100 bpm at rest (tachycardia) and you feel short of breath or have chest pain, that's not something to ignore. Similarly, if your pulse is under 60 and you feel like you might pass out, your heart might not be circulating enough oxygenated blood.
Dr. Leslie Cho from the Cleveland Clinic emphasizes that "normal" is a trend, not a moment. One high reading doesn't mean you have heart disease. A month of high readings might mean you need to look at your stress, your thyroid, or your fitness levels.
Measuring It Properly (Stop Using Your Thumb)
If you want to know what pulse rate is normal for you, you have to measure it correctly. Don't use your thumb—it has its own pulse that can confuse the count. Use your index and middle fingers on your wrist (radial pulse) or the side of your neck (carotid pulse).
Count the beats for 30 seconds and multiply by two. Or 15 seconds and multiply by four. Do this first thing in the morning, before you get out of bed, and before you check your phone. The "morning's first news scroll" is a great way to spike your pulse before you've even brushed your teeth. This baseline is your true resting heart rate.
The Wearable Trap
We are living in an era of over-monitoring. Apple Watches, Garmins, and Oura rings provide a constant stream of data. This is a double-edged sword. While it’s great for catching things like Atrial Fibrillation (AFib), it also leads to "health anxiety."
Sometimes these sensors glitch. A loose watch band can misread a pulse, showing a terrifyingly high or low number that isn't real. If your watch says your heart rate is 210 while you're brushing your teeth, but you feel completely fine, it’s probably the watch, not your heart. Always check your pulse manually if the digital reading seems insane.
Nuance in the Numbers
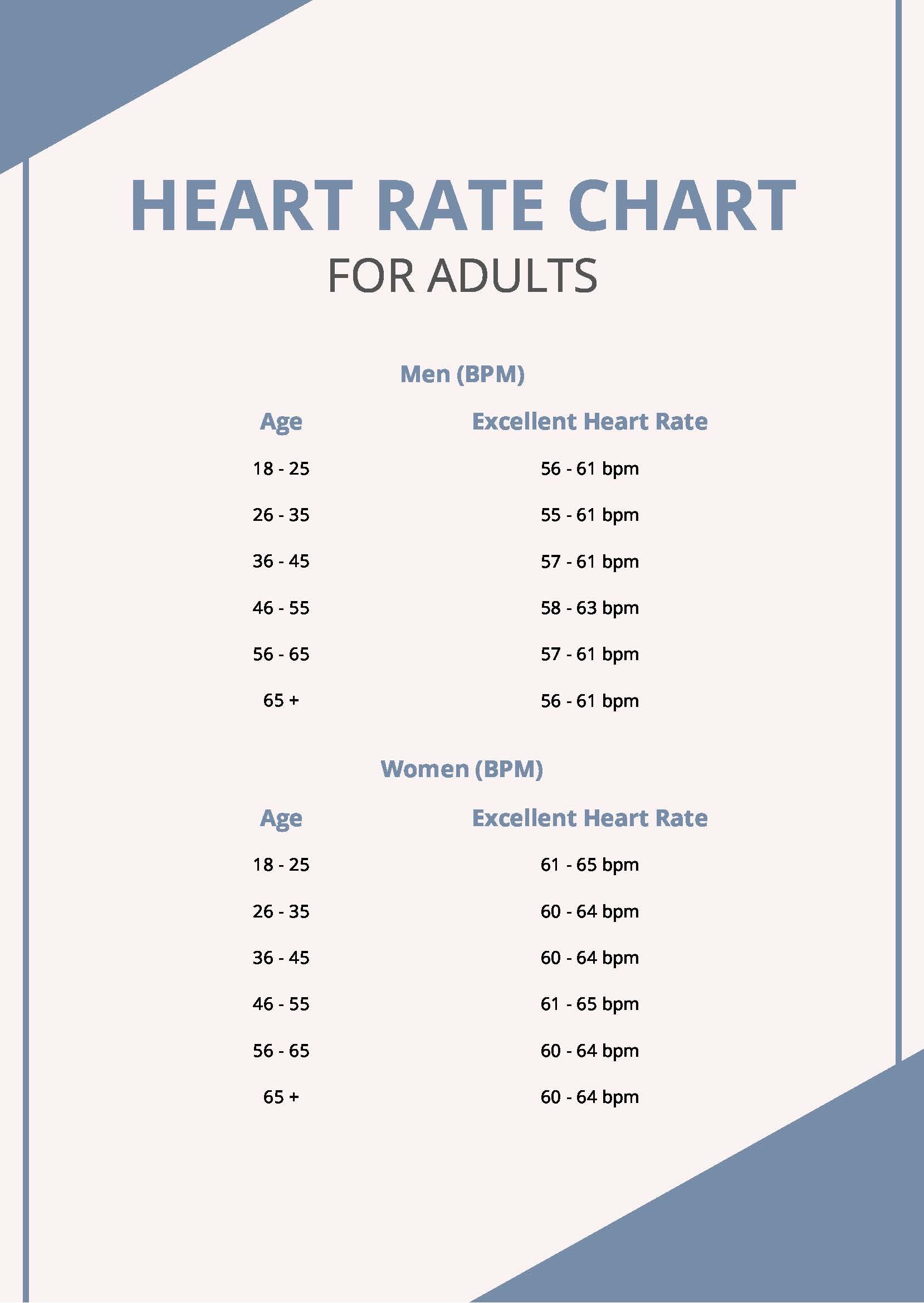
There is also a gender component. On average, women tend to have slightly higher resting heart rates than men. This is largely due to the size of the heart; smaller hearts pump less blood per beat and need to beat a bit faster to compensate. It’s a perfectly normal physiological difference.
👉 See also: How Long Norovirus Lasts: The Reality of Dealing with the Stomach Bug
Then there are medications. Beta-blockers, often prescribed for blood pressure or anxiety, are designed specifically to slow the heart down. If you’re on a beta-blocker, your "normal" might be 55 bpm, and that’s exactly where your doctor wants you. Conversely, some asthma inhalers or decongestants can send your pulse racing.
Actionable Steps for Heart Health
Instead of just watching the number, focus on the variables you can control. Improving your "normal" pulse rate is usually a long game of lifestyle tweaks rather than a quick fix.
1. Prioritize Sleep Hygiene
Sleep deprivation puts your body in a state of sympathetic nervous system dominance. Basically, you’re in "fight or flight" mode all day. This keeps your resting pulse higher than it should be. Aim for consistency over duration—going to bed at the same time is often more impactful than just getting a random eight hours.
2. Hydrate Like It’s Your Job
Most people are walking around slightly dehydrated. Your blood becomes thicker, your heart works harder. Drinking enough water is the easiest way to lower a slightly elevated resting heart rate.
3. Interval Training
You don't need to run a marathon. Short bursts of higher-intensity movement followed by rest (HIIT) teach your heart how to recover quickly. The "recovery rate"—how fast your pulse returns to normal after exercise—is actually a better predictor of heart health than the resting pulse itself.
4. Breathwork and Vagus Nerve Stimulation
You can manually "hack" your heart rate. Slow, deep exhalations stimulate the vagus nerve, which tells your heart to slow down. If you're feeling your pulse thumping in your chest, try the 4-7-8 breathing technique (inhale for 4, hold for 7, exhale for 8). It works almost instantly to bring the numbers down.
5. Audit Your Supplements
Many "pre-workout" powders or weight loss supplements are loaded with massive amounts of caffeine and other stimulants like yohimbine. These can cause your heart rate to stay elevated for hours. If you're concerned about your pulse, check your labels.
Understanding what pulse rate is normal requires looking at the whole person, not just the wrist. If you are active, eating reasonably well, and managing your stress, your heart is likely doing exactly what it needs to do. Your "normal" is a personal baseline. Track it over time, look for trends rather than spikes, and use the data as a tool for curiosity rather than a reason for panic.
If your resting rate changes significantly over the course of a week without a clear cause—like illness or a change in exercise—that is the time to call your doctor. Otherwise, take a deep breath. Your heart has likely got this handled.
Next Steps for Your Health:
- Establish your baseline: Measure your pulse manually for three consecutive mornings before getting out of bed.
- Check your medications: Look for "tachycardia" or "increased heart rate" as side effects on any prescriptions or over-the-counter meds you take regularly.
- Test your recovery: After a brisk walk, time how long it takes for your pulse to drop back below 100 bpm; a drop of 15-20 beats in the first minute is a great sign of cardiovascular health.
- Manual verification: If your wearable device gives a reading that makes you anxious, immediately take a manual 30-second count to verify accuracy before reacting.