Hollywood has done us a massive disservice. You know the scene: a man suddenly gasps, clutches his chest with a "claws-out" grip, and collapses onto the floor in a heap. It’s dramatic. It’s unmistakable. It’s also, quite frankly, not how it usually happens in the real world. If you're waiting for that level of theatrics, you might miss the boat entirely.
When people ask what is the first sign of a heart attack, they are often looking for a single, definitive "aha!" moment. But the heart is a complex muscle, and it doesn't always scream. Sometimes, it just whispers.
Understanding this isn't just about trivia. It’s about survival. Every minute your heart muscle is deprived of oxygenated blood, the damage becomes more permanent. We’re talking about "time is muscle."
The Heavy Truth About That First Signal
So, let's get into it. What is the first sign of a heart attack for the average person? Statistically, the most common early indicator is chest discomfort. Notice I didn't say "pain."
Pain is a strong word. People often dismiss their symptoms because they don't feel like they're being stabbed. Instead, they describe a sensation of pressure. It’s like an elephant is sitting on their chest. Or a tight band is being squeezed around their ribs. Sometimes it’s just a weird, dull ache that won't go away no matter how much you stretch or change positions.
According to the American Heart Association, this discomfort often starts in the center of the chest. It might last for a few minutes, go away, and then come back with a vengeance. This "stuttering" pattern is a massive red flag.
Why we ignore it
We are experts at self-delusion. "It's just the spicy tacos I had for lunch," we tell ourselves. Heartburn and heart attacks share a lot of the same real estate in the chest. Because the nerves in the chest don't always give the brain a precise GPS coordinate of where the trouble is, your brain can easily mistake a blocked artery for an overactive stomach.
💡 You might also like: Medicine Ball Set With Rack: What Your Home Gym Is Actually Missing
But here’s the kicker: if you take an antacid and the "heartburn" doesn't budge after 15 minutes, you need to stop diagnosing yourself.
The Gender Gap in Symptoms
Women often experience that "first sign" very differently than men. This is where things get tricky and, honestly, a bit dangerous. While men usually get the classic chest pressure, women are more likely to report symptoms that seem totally unrelated to the heart.
I’ve talked to nurses who have seen women walk into the ER complaining of nothing but extreme, crushing fatigue. They feel like they’ve run a marathon when they’ve only walked to the mailbox.
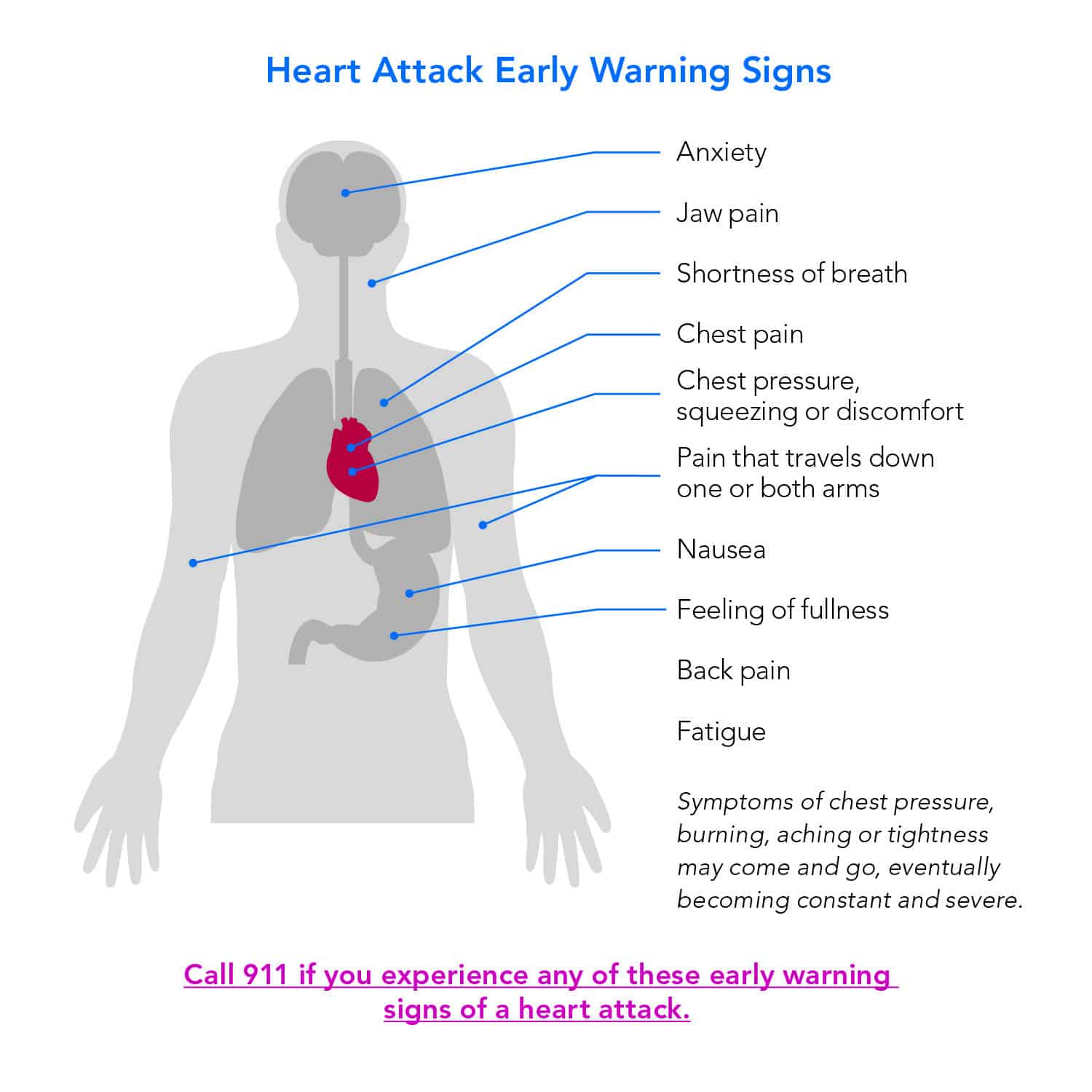
For many women, the first sign of a heart attack is actually:
- Shortness of breath without any chest pain at all.
- Nausea or a feeling of lightheadedness.
- A weird, nagging pain in the lower jaw or neck.
- Pressure in the upper back that feels like a pulled muscle.
If you’re a woman and you suddenly feel "off" in a way you can't explain—accompanied by a cold sweat or sudden anxiety—don't ignore it. Dr. Nieca Goldberg, a cardiologist and spokesperson for the AHA, has spent years pointing out that women’s symptoms are frequently dismissed as "anxiety" or "stress." Don't let a doctor tell you it's just stress if your gut tells you otherwise.
The "Silent" Warning
Can you have a heart attack and not even know it? Absolutely. It’s called a Silent Myocardial Infarction (SMI).
📖 Related: Trump Says Don't Take Tylenol: Why This Medical Advice Is Stirring Controversy
In these cases, the what is the first sign of a heart attack question becomes even more haunting because there might not be a "sign" in the traditional sense. A study published in the journal Circulation found that nearly half of all heart attacks may be silent.
People realize it weeks or months later when an EKG shows scarring on the heart muscle. They might recall a day when they felt a bit "flu-like" or had a lingering bout of indigestion. That was the heart attack. If you have diabetes, you are at a much higher risk for these silent events because high blood sugar can damage the nerves that carry pain signals from the heart.
Physical Cues You Can't Ignore
Beyond the chest, your body starts throwing out "referred pain." Your heart is struggling, and it’s sending out distress signals that travel along the same nerve pathways as your arms and jaw.
The Left Arm Myth
Everyone thinks it has to be the left arm. While the left arm is common, the pain can actually radiate to either arm. Or both. It usually feels like a heavy, numb sensation or a tingly ache that travels down to the wrist.
Cold Sweats and "Impending Doom"
There is a specific symptom that paramedics look for: the "gray" look. When the heart struggles, the sympathetic nervous system goes into overdrive. You might break out in a cold, clammy sweat even if the room is freezing.
Many survivors also describe a profound sense of "impending doom." It sounds poetic, but it’s a physiological response. Your body knows something is fundamentally wrong before your conscious mind can process it. It’s a primal "get help now" signal.
👉 See also: Why a boil in groin area female issues are more than just a pimple
What to Do When the Signal Hits
If you suspect that you or someone near you is experiencing what is the first sign of a heart attack, you have a very narrow window to act.
- Call 911 immediately. Do not drive yourself to the hospital. If you black out behind the wheel, you’re a danger to everyone. Paramedics can start treatment—like performing an EKG and administering oxygen—the second they arrive.
- Chew an aspirin. Unless you are allergic, chewing (not swallowing whole) a full-strength 325mg aspirin can help break up the blood clot that is likely causing the blockage. Chewing it gets it into your bloodstream faster.
- Sit down and stay calm. Deep breaths. Don't try to "walk it off." Any physical exertion puts more strain on the heart muscle that is already gasping for air.
Risk Factors vs. Reality
We like to think heart attacks only happen to "unhealthy" people. We picture the 70-year-old smoker. But the reality is more nuanced. Genetics play a massive role. You can be a marathon runner with a perfect diet and still have a blockage if your family history is working against you.
High blood pressure (the "silent killer") and high cholesterol are the primary drivers. If you haven't had a blood panel in over a year, you’re flying blind. You won't feel high blood pressure until it's already doing damage.
Actionable Steps for Right Now
Knowing the signs is half the battle, but preparation is the other half.
- Check your family tree. Did your father or brother have a heart event before 55? Did your mother or sister have one before 65? If yes, your "baseline" risk is higher, and you should be more aggressive with screenings.
- Get a Calcium Score test. If you're over 40 and have intermediate risk, this specialized CT scan can literally see the buildup of plaque in your coronary arteries before it causes a heart attack. It’s often not covered by insurance, but it usually costs around $100 and provides a definitive look at your "clogged pipe" status.
- Download a pulse-tracking app or use a smartwatch. While not a diagnostic tool for a heart attack, noticing a sudden, unexplained spike in your resting heart rate or the onset of atrial fibrillation (Afib) can be the early warning you need to see a cardiologist.
- Carry a "Heart Card." Keep a small note in your wallet listing your current medications, any allergies (especially to aspirin or blood thinners), and an emergency contact. When you're in the middle of a cardiac event, you won't be able to remember the name of that one pill you take for your thyroid.
The most important thing to remember is that it is always better to be sent home from the ER with a "it's just gas" diagnosis than to stay home with a heart attack. Doctors won't laugh at you. They’d much rather see you for a false alarm than an autopsy.
Pay attention to the pressure. Listen to the fatigue. Trust that weird feeling of doom. Your heart is the only one you've got—don't wait for the movie-style collapse to start taking it seriously.