You're sitting in the doctor's office, sleeve rolled up, watching that Velcro cuff squeeze your arm until it pulses. For decades, you probably heard the same magic number: 120/80. It was the gold standard, the holy grail of cardiovascular health. But honestly, things get a bit more nuanced once you hit your 70s. If you're wondering what is normal blood pressure for a 70-year-old male, the answer isn't a single static digit on a screen. It’s a moving target influenced by your history, your kidneys, and how dizzy you feel when you stand up too fast.
The medical community has been arguing about this for years. Some experts lean toward aggressive control, while others worry that pushing a 70-year-old’s pressure too low causes more harm than good.
The numbers you actually need to know
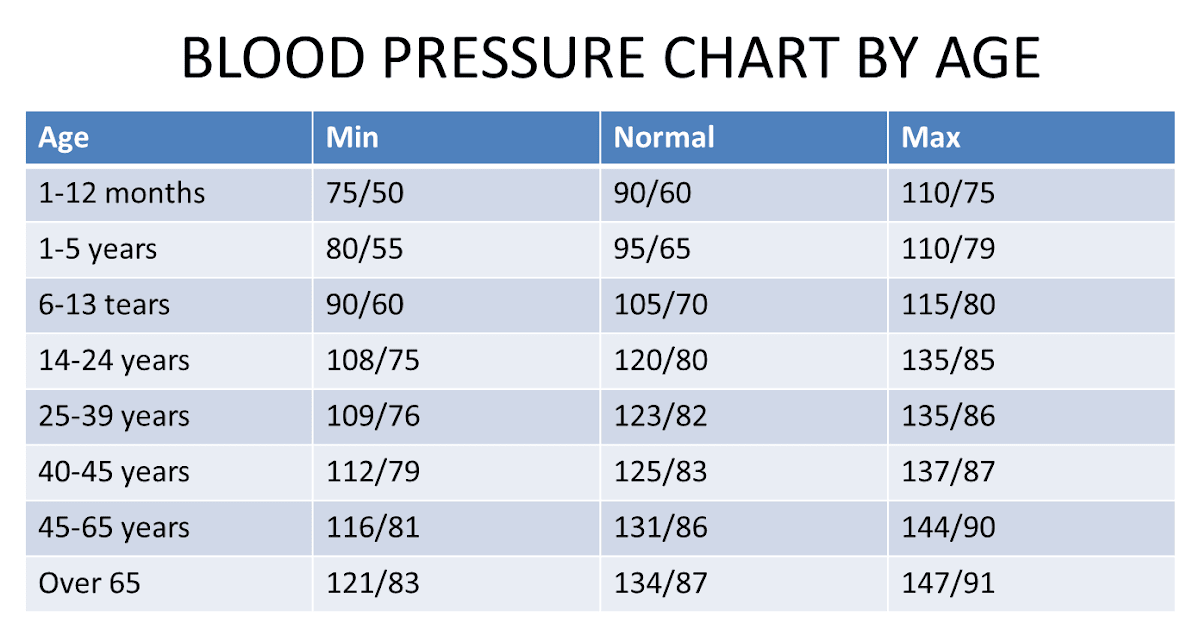
Current guidelines from the American Heart Association (AHA) and the American College of Cardiology (ACC) generally suggest that for most adults, including those over 70, "normal" is still considered less than 120/80 mmHg. But here’s the kicker. "Normal" and "Target" are two different things.
Most doctors aren't going to panic if a 72-year-old man clocks in at 130/80. In fact, many practitioners follow the SPRINT trial (Systolic Blood Pressure Intervention Trial) logic, which showed significant benefits in lowering systolic pressure to below 120 in older adults, but they balance that against the risk of falls.
If your top number—the systolic—is consistently between 130 and 139, you’re officially in Stage 1 Hypertension territory.
Does that mean you're in immediate danger? Not necessarily. But it does mean your arteries are stiffer than they used to be. That's just biology. As we age, the structural proteins in our arterial walls, like collagen and elastin, change. The vessels get less "bouncy." This leads to isolated systolic hypertension, where the top number climbs while the bottom number (diastolic) stays the same or even drops.
Why 140/90 used to be the "okay" mark
It wasn't that long ago that the JNC 8 guidelines suggested 150/90 was an acceptable target for folks over 60. The logic was simple: we didn't want seniors fainting. When blood pressure drops too low, especially in a 70-year-old male, the brain doesn't get enough perfusion. You stand up, the lights go dim, you hit the floor, and suddenly you’ve got a broken hip.
💡 You might also like: Can DayQuil Be Taken At Night: What Happens If You Skip NyQuil
The pendulum swung back toward 130/80 because the data on strokes and heart attacks was too loud to ignore.
Still, your "normal" depends on your "frailty." A marathon-running 70-year-old has a different physiological profile than a 70-year-old dealing with type 2 diabetes and stage 3 kidney disease. For the latter, a doctor might be perfectly happy with 135/85 because pushing it lower might stress the kidneys too much.
The "White Coat" factor is real
You can't talk about what is normal blood pressure for a 70-year-old male without mentioning the stress of the clinic. Many men in this age bracket experience a massive spike the moment they see a stethoscope.
You’ve got to track this stuff at home.
One reading at 2:00 PM after you struggled to find a parking spot and walked up three flights of stairs means nothing. You need the "rested" average. Sit in a chair. Feet flat. Back supported. No talking. No scrolling on your phone. Wait five minutes. Then take the reading. If your home average is 125/78, but the doctor's office says 145/90, you likely have white coat hypertension.
What happens when the gap widens?
You might notice your numbers look something like 145/70. This is called a wide pulse pressure.
📖 Related: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
Pulse pressure is the difference between the top and bottom numbers. In this case, $145 - 70 = 75$. A pulse pressure greater than 60 is often a "red flag" for cardiovascular aging. It suggests the large artery—the aorta—has lost its elasticity. It’s stiff. When the heart pumps, the stiff aorta can't expand to buffer the pressure, so the systolic number shoots up. When the heart rests, the aorta doesn't recoil properly, so the diastolic pressure drops.
This is very common in men in their 70s. It’s also a predictor of future heart issues, sometimes more so than the individual numbers themselves.
The role of lifestyle (it’s not just salt)
Everyone blames the salt shaker. Sure, sodium matters. But at 70, potassium might matter more.
As we age, our kidneys become less efficient at flushing out salt. Increasing potassium-rich foods—potatoes, bananas, spinach—helps the body excrete sodium and eases the tension in the blood vessel walls.
Then there's the alcohol factor. You might have enjoyed a couple of scotches or beers every night for forty years. But the way a 70-year-old body processes ethanol is different than a 40-year-old body. Alcohol can cause "rebound" hypertension, where your pressure spikes as the liver clears the toxins.
And don't overlook sleep apnea. If you're snoring loudly and waking up tired, your blood pressure will never be "normal" because your body is under a state of oxygen-deprived panic all night long.
👉 See also: That Time a Doctor With Measles Treating Kids Sparked a Massive Health Crisis
Medication: Is it inevitable?
Not always. But look, if you’re hitting 145/90 consistently, lifestyle changes might only get you so far.
Modern medications like ACE inhibitors, ARBs, or low-dose diuretics (water pills) are incredibly effective. The goal isn't to "over-medicate." It's to prevent a stroke that could change your life in thirty seconds.
The conversation you have with your doctor should be about "quality of life" targets. If a medication makes you feel like a zombie or causes "orthostatic hypotension" (that head-rush when standing), the dose is wrong.
Actionable steps for the 70-year-old male
Don't just take a pill and hope for the best. Take control of the data.
- Buy a validated home monitor. Look for the "AAMI" or "ESH" validation seal. Wrist cuffs are generally garbage for 70-year-olds because arterial stiffness makes them inaccurate. Stick to the upper arm cuff.
- Log your readings for two weeks. Take one in the morning and one in the evening. Ignore the outliers. Look for the trend.
- Check your "standing" pressure. Take your blood pressure sitting down, then stand up and take it again after one minute. If the top number drops by more than 20 points, you are at a high risk for falls. Tell your doctor immediately.
- Monitor your "DASH" intake. The Dietary Approaches to Stop Hypertension isn't a fad; it’s one of the most studied diets in medical history. It focuses on magnesium, calcium, and potassium.
- Assess your magnesium. Many men in their 70s are slightly deficient in magnesium, which acts as a natural calcium channel blocker to help relax blood vessels.
Finding your specific "Normal"
Ultimately, what is normal blood pressure for a 70-year-old male is the pressure at which your brain stays sharp, your kidneys stay functional, and your heart isn't working overtime. For most, that means aiming for a target of less than 130/80, but accepting a bit of wiggle room if you are prone to dizziness or other side effects.
If you're currently seeing numbers consistently above 140/90, it's time to tweak the protocol. Whether that's cutting back on processed meats, increasing your daily walk by ten minutes, or adjusting a prescription, the goal is longevity with functionality. Keeping the pipes clear and the pressure steady is the best way to ensure your 70s and 80s are spent on the golf course or with grandkids, rather than in a recovery ward.
Focus on the average, watch for the "dizzy" spells, and keep a paper log. Your doctor will thank you, and your heart will, too.