You’re sitting in that small, sterile room. The nurse wraps a velcro cuff around your arm, pumps it up until it pinches, and then lets the air hiss out. Two numbers pop up on the screen. Maybe it’s 128/82. Or 115/75. Most of us just nod when the nurse says "looks okay" and we go about our day. But honestly, "okay" is a moving target. If you’ve been wondering what are good blood pressure numbers, the answer isn't a single static digit. It’s a range that shifted significantly a few years ago when the American Heart Association (AHA) and the American College of Cardiology (ACC) tightened the rules.
Blood pressure is basically just the force of your blood pushing against the walls of your arteries. Think of it like a garden hose. If the pressure is too high, the hose starts to fray. Eventually, it bursts or leaks. In your body, that "bursting" is a stroke or a heart attack. It’s quiet. It doesn't usually hurt. That's why they call it the silent killer.
The Reality of the Numbers
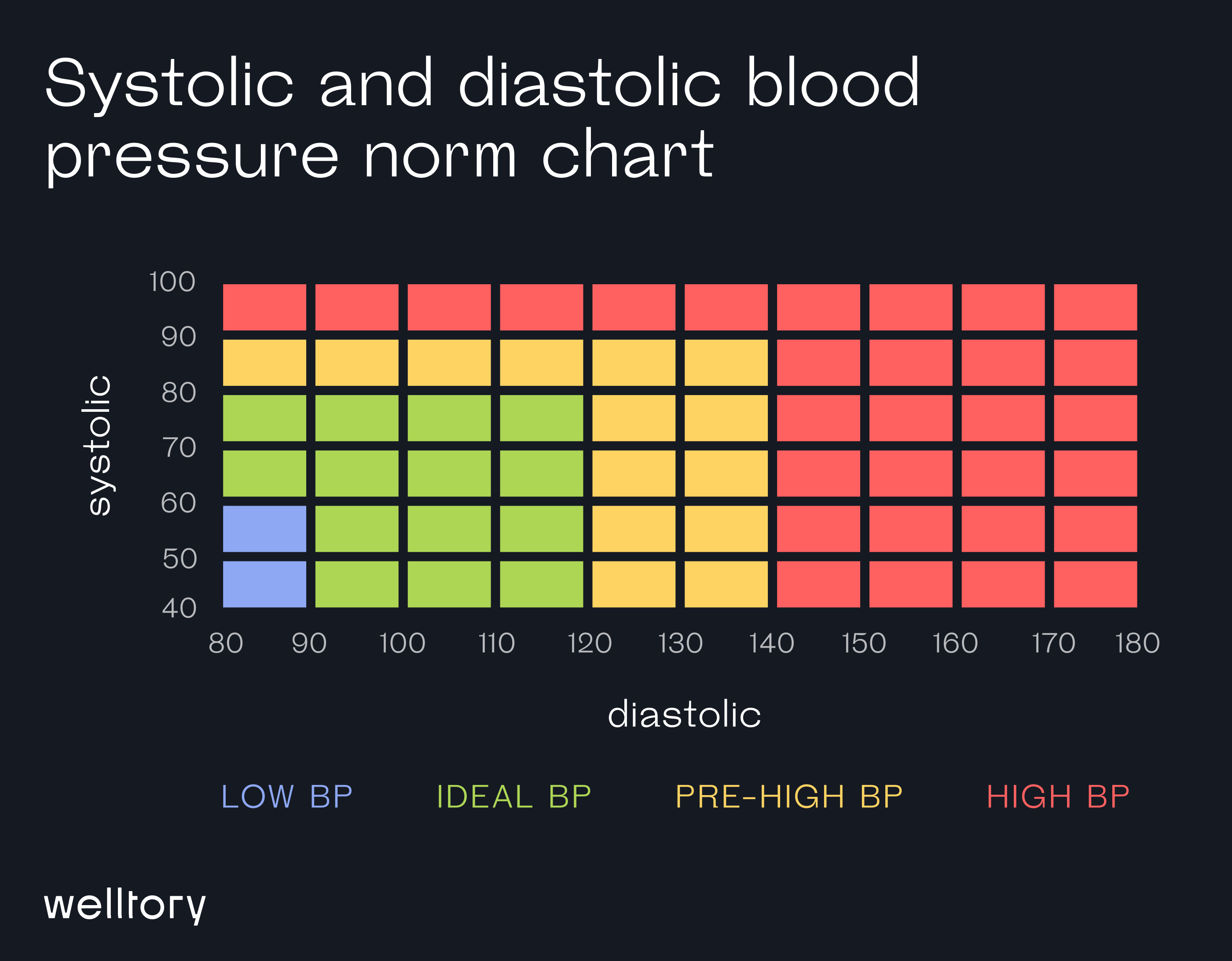
When we talk about what are good blood pressure numbers, we are looking at systolic (the top number) and diastolic (the bottom number). The top one measures pressure when your heart beats. The bottom one is the pressure when your heart rests between beats.
For a long time, the "gold standard" was 120/80 mmHg. If you were under that, you were golden. But things changed in 2017. Now, the medical community is much more aggressive.
A "normal" reading is officially anything less than 120/80 mmHg. If your top number is between 120 and 129, and your bottom number is still less than 80, you are now in the "Elevated" category. You don't have hypertension yet, but you're on the porch. Doctors get worried here because data from the SPRINT trial (Systolic Blood Pressure Intervention Trial) showed that lower is almost always better for long-term survival.
Once you hit 130/80, you’ve officially entered Stage 1 Hypertension. Many people are shocked by this. They feel great. They run marathons. They eat kale. But 130/80 is the new line in the sand.
Why 130 is the New 140
It feels like moving the goalposts, doesn't it? It kinda is.
The reason experts lowered the threshold for "good" numbers is that they realized damage starts much earlier than we thought. Even slightly elevated pressure begins to stiffen the arteries. This leads to left ventricular hypertrophy—where the heart muscle gets thick and stiff because it’s working too hard. It’s like a bodybuilder who gets too big to move effectively.
💡 You might also like: That Weird Feeling in Knee No Pain: What Your Body Is Actually Trying to Tell You
Dr. Paul Whelton, who chaired the committee that wrote the 2017 guidelines, points out that the risk of cardiovascular disease doubles at 130/80 compared to someone at 120/80. That’s a massive jump for a ten-point difference.
Breaking Down the Stages
- Normal: Under 120/80. This is the dream.
- Elevated: 120–129 top, and under 80 bottom.
- Hypertension Stage 1: 130–139 top, or 80–89 bottom.
- Hypertension Stage 2: 140 or higher top, or 90 or higher bottom.
- Hypertensive Crisis: Over 180 top and/or over 120 bottom. If you see this on your home monitor, wait five minutes and test again. If it’s still that high, call 911. Seriously.
Notice I said "or" in those stages. If your top number is 118 but your bottom number is 84, you have Stage 1 Hypertension. The higher number always determines the category.
The "White Coat" Problem and Home Monitoring
Have you ever noticed your heart racing the second you walk into a doctor’s office? It's real. White Coat Hypertension affects up to 30% of patients. Your numbers look like a disaster at the clinic, but they’re perfectly fine when you’re sitting on your couch watching Netflix.
This is why a single reading is basically useless. To truly know what are good blood pressure numbers for you, you need a trend.
The gold standard for diagnosis is now Ambulatory Blood Pressure Monitoring (ABPM) or at-home monitoring. You should get a validated cuff—the ones that go on your upper arm, not the wrist ones, which are notoriously finicky—and check yourself at the same time every day.
How to actually take your blood pressure
Most people do it wrong. They sit down, legs crossed, talking to their spouse, and hit the "start" button. That can add 10 to 15 points to your reading.
Here is how you get an honest number.
📖 Related: Does Birth Control Pill Expire? What You Need to Know Before Taking an Old Pack
Empty your bladder first. Sit in a chair with your back supported. Keep your feet flat on the floor. Don’t cross your legs. Your arm should be resting on a table at heart level. Stay silent. Don't check your phone. Sit there for five minutes before you even touch the machine. Take two or three readings a minute apart and average them.
The Nuance: Age and Individual Health
Is 120/80 right for everyone? Not necessarily.
Medicine is rarely one-size-fits-all. If you’re 85 years old, a doctor might be perfectly happy with you sitting at 135/85. Why? Because if they push your pressure too low with meds, you might get dizzy, fall, and break a hip. The risk of the treatment becomes higher than the risk of the pressure.
Then there’s the "J-curve" phenomenon. There is some evidence that pushing diastolic pressure (the bottom number) too low—below 60 or 70—might actually reduce blood flow to the heart muscle itself. It's a delicate balance.
If you have diabetes or chronic kidney disease, the stakes are higher. High pressure shreds the delicate filters in your kidneys. For these patients, getting back to those "good" numbers isn't just a suggestion; it’s a life-extending necessity.
What Actually Works to Lower the Numbers?
If you find out your numbers aren't in the "good" zone, don't panic. You aren't immediately destined for a lifetime of pills. Lifestyle changes are surprisingly powerful.
The DASH diet (Dietary Approaches to Stop Hypertension) is the most studied intervention here. It’s heavy on fruits, veggies, and low-fat dairy. But the real kicker is sodium. Most of us eat an insane amount of salt. We’re talking 3,400mg a day when we should be under 1,500mg.
👉 See also: X Ray on Hand: What Your Doctor is Actually Looking For
Cutting back on salt can drop your systolic pressure by 5 to 6 points. That’s as much as some low-dose medications.
And then there's exercise. You don't have to become a gym rat. Brisk walking for 150 minutes a week—about 20 minutes a day—can drop your numbers significantly. Weight loss is also huge. For every kilogram (about 2.2 lbs) of weight you lose, you can expect your blood pressure to drop by about 1 mmHg. Lose 20 pounds, and you might just move yourself from Stage 1 back to Elevated or even Normal.
Misconceptions That Can Be Dangerous
A lot of people think they can "feel" when their blood pressure is high. They’ll say, "I have a headache, my pressure must be up."
Usually, that’s not true.
Unless you are in a hypertensive crisis (180/120+), you generally won't feel a thing. That’s the danger. You could be walking around with 150/95 for five years, feeling like a million bucks, while your arteries are slowly scarring.
Another myth: "It’s just stress."
Stress definitely spikes your pressure. If a tiger jumps out at you, your pressure should go up. That's your body working correctly. But if your pressure is 145/90 when you’re "stressed" at the office every day, that's still hypertension. Chronic stress keeps your vessels constricted, and eventually, they stay that way.
Actionable Steps for Better Numbers
Knowing the numbers is only half the battle. You have to manage them. If you’re outside the "good" range, here is the roadmap:
- Verify the data. Buy a reputable home monitor (brands like Omron or Withings are often clinically validated). Track your numbers for two weeks, twice a day—once in the morning and once in the evening.
- Audit your salt. Don't just stop shaking the salt wand. Look at labels. Bread, deli meats, and canned soups are salt bombs.
- Potassium is your friend. Potassium helps your body ease the tension in your blood vessel walls and flush out excess sodium. Eat more bananas, potatoes (with the skin!), and spinach.
- Watch the booze. More than one or two drinks a day can significantly raise blood pressure over time.
- Talk to your doctor about "The Why." Is it genetics? Is it sleep apnea? (Sleep apnea is a massive, often undiagnosed cause of high blood pressure).
Understanding what are good blood pressure numbers gives you a baseline for your cardiovascular health. If you are under 120/80, keep doing what you’re doing. If you’re above that, it’s not a moral failure—it’s just a signal that your "pipes" need a little maintenance before a leak starts. Take the data to your physician and start the conversation before the silence of the "silent killer" becomes a problem you can no longer ignore.