You’re in the kitchen. You’ve got the fridge door open. Honestly, you have no idea why you're standing there. This happens to everyone, right? It’s the "doorway effect." But for millions of families, these tiny lapses start to feel... different. They get heavier. When we talk about warning signs of Alzheimer's, we aren't just talking about forgetting where the car keys are. We’re talking about a fundamental shift in how a brain processes the world.
It’s scary.
People often wait years to see a doctor because they’re terrified of the answer, or they just assume getting older means losing your mind. That’s a myth. Aging brings wisdom and maybe a slower recall speed, but it shouldn't steal your ability to function. Alzheimer's Disease International estimates that a huge portion of cases—maybe up to 75%—go undiagnosed globally. That is a staggering number of people navigating a neurological minefield without a map.
It’s not just "Senior Moments" anymore
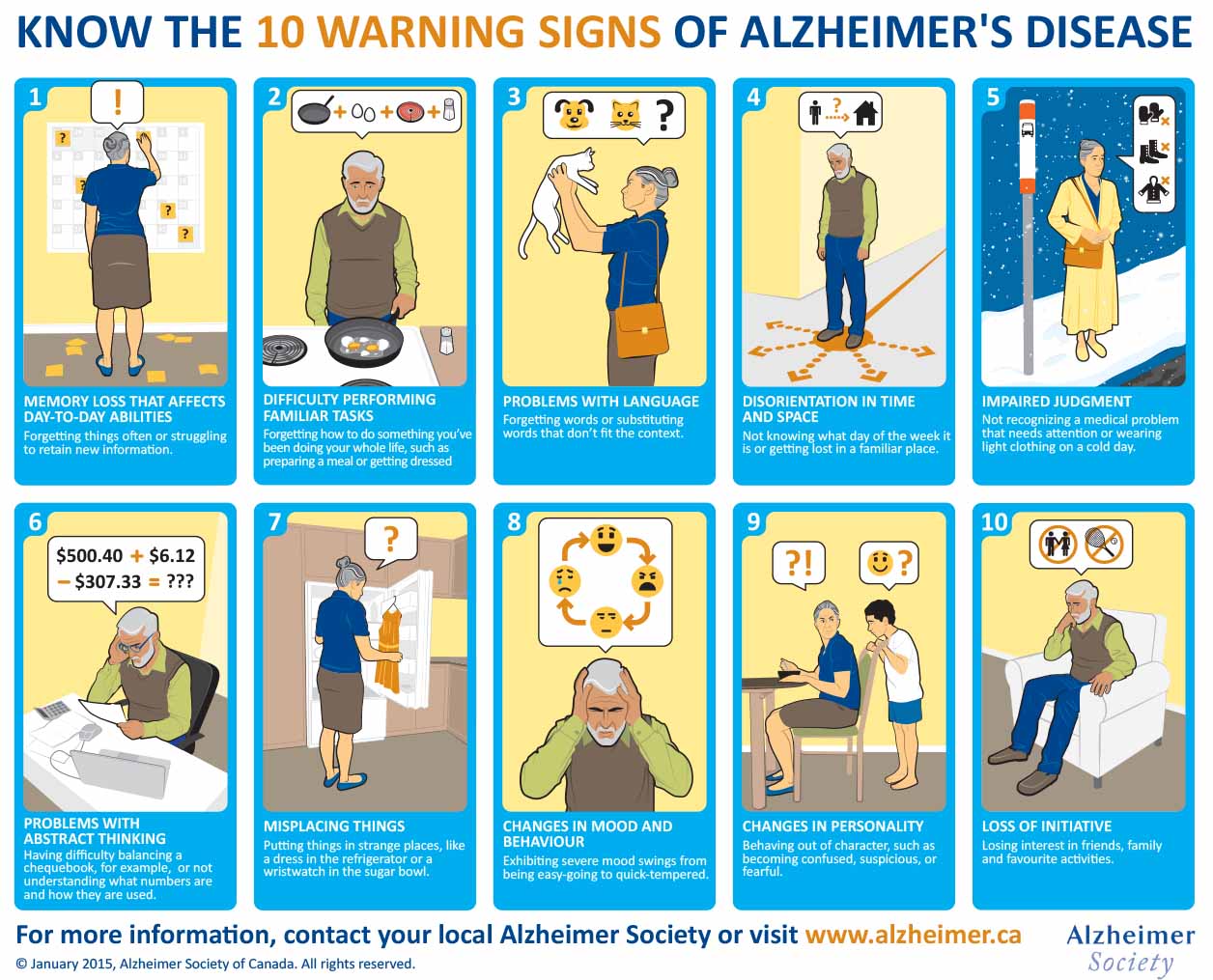
The biggest misconception is that memory loss is the only thing to watch for. If you’re looking for warning signs of Alzheimer's, you have to look at the "Executive Function." This is the CEO of your brain. It handles the bills. It follows the recipe for Sunday roast. It knows that if the light is red, you stop the car.
When someone starts struggling with a familiar task, like getting lost driving to the grocery store they’ve used for twenty years, that’s a red flag. It’s not just a "oops, took a wrong turn." It’s a spatial disorientation that feels visceral. My friend’s dad, a lifelong woodworker, suddenly couldn't figure out the sequence of steps to sand a table. He knew what a sander was. He knew what wood was. But the bridge between the two—the logic—was vanishing.
The subtle shift in mood and personality
Sometimes the very first thing to change isn't memory at all. It’s temperament. According to the Alzheimer's Association, people might become uncharacteristically confused, suspicious, depressed, fearful, or anxious.
They might get easily upset at home, at work, or with friends. Or maybe they withdraw. Imagine a woman who was the life of every party suddenly refusing to go to brunch because she can't keep up with the fast-paced chatter. It’s exhausting to try and "mask" cognitive decline. So, people stop trying. They pull away. This social withdrawal is often misdiagnosed as late-onset depression, but in reality, it’s the brain’s way of protecting itself from the overwhelm of a world it no longer fully understands.
✨ Don't miss: Ankle Stretches for Runners: What Most People Get Wrong About Mobility
Decoding the warning signs of Alzheimer's in daily life
Let’s get specific. Doctors look for patterns, not one-off events. If you forget your password once, you’re human. If you can no longer understand what a password is for, that’s a different story.
One major indicator is losing the ability to retrace steps. We all misplace things. You find your phone in the bathroom and think, "Oh right, I brought it in here when I was brushing my teeth." A person with Alzheimer's might put their phone in the freezer and have absolutely no recollection of how it got there. They lack the "mental film" to rewind their day. This often leads to accusations—they might think someone is stealing from them because they can't account for the missing items. It's heartbreaking, and it's a very common friction point for caregivers.
Language and the "Tip of the Tongue"
Finding the right word is hard for everyone. But watch for "the thingy" or "the hand-clock" instead of "watch." This is called anomia. It’s not just forgetting a name; it’s a breakdown in the linguistic filing cabinet.
A study published in the journal Brain highlighted how changes in writing and speech patterns—using simpler words, shorter sentences, or repeating the same ideas—can appear years before a clinical diagnosis. It’s subtle. It’s kind of like a fading signal on a radio station. You still hear the music, but there’s more static every day.
The Science: What’s actually happening?
We can't talk about this without mentioning plaques and tangles.
Basically, two proteins—amyloid and tau—start behaving badly. Amyloid clumps together between neurons, disrupting cell-to-cell communication. Tau, meanwhile, builds up inside the cells, eventually killing them. This usually starts in the hippocampus. That's the part of your brain responsible for forming new memories. That’s why the "new stuff" goes first. A person might remember the name of their third-grade teacher but forget what they had for breakfast twenty minutes ago.
🔗 Read more: Can DayQuil Be Taken At Night: What Happens If You Skip NyQuil
The diagnostic dilemma
Is it Alzheimer’s or something else? This is where it gets tricky.
- Vitamin B12 deficiency: Can mimic dementia symptoms perfectly.
- Thyroid issues: An underactive thyroid can cause "brain fog" and memory slips.
- Urinary Tract Infections (UTIs): In older adults, a UTI can cause sudden, intense confusion called delirium. It looks exactly like late-stage Alzheimer's, but it's treatable with antibiotics.
- Normal Pressure Hydrocephalus: A buildup of fluid in the brain that causes walking issues, incontinence, and memory loss.
This is why "self-diagnosing" via the internet is dangerous. You need a neurologist. You need blood work. You might even need a PET scan to see if those amyloid plaques are actually there. The Mayo Clinic emphasizes that a thorough workup is the only way to rule out reversible causes. Honestly, if it is a B12 deficiency, you'd want to know that immediately because it's fixable.
Why the "Early" part of early detection matters
There is no cure yet. Let’s be real about that. But there are treatments like Lecanemab (Leqembi) and Donanemab, which are monoclonal antibodies designed to clear amyloid from the brain. These aren't magic bullets. They don't bring back dead neurons. But they can slow the decline in people who are in the very early stages.
If you wait until the warning signs of Alzheimer's are screaming, these medications usually aren't an option.
Early detection also gives a person "Agency." It allows them to participate in their own legal and financial planning. They can say, "This is how I want my life to look," before they lose the capacity to make those choices. It's about dignity.
Beyond Memory: Vision and Spatial Awareness
This one surprises people. Alzheimer’s can mess with your eyes, but not in the way a cataract does. It’s the brain’s interpretation of what the eyes see.
💡 You might also like: Nuts Are Keto Friendly (Usually), But These 3 Mistakes Will Kick You Out Of Ketosis
Some people have trouble reading, judging distance, or determining color/contrast. This makes driving incredibly dangerous. They might see a shadow on the floor and think it's a hole. They might reach for a glass of water and completely miss it because their depth perception is shot. If your loved one is suddenly bumping into furniture or seems hesitant to walk over different flooring surfaces (like moving from carpet to tile), it might not be a balance issue. It might be a brain-vision disconnect.
The "Sun-Downing" Phenomenon
You’ll hear caregivers talk about this. As the sun goes down, the confusion ramps up. The person might become restless, agitated, or even aggressive. Scientists aren't 100% sure why it happens, though it likely involves the disruption of the body’s internal clock (circadian rhythm). It’s like their brain’s "battery" is drained, and they no longer have the cognitive energy to keep it together.
Navigating the Conversation
How do you tell someone you think they have it? You don't. At least, not like that.
Instead of saying, "You're forgetting everything, you might have Alzheimer's," try focusing on the "Check-up." You could say, "I’ve noticed you've been a little more stressed and forgetful lately, and I'm worried about you. Let’s go get some blood work done to make sure everything is balanced."
Make it about health, not about "losing your mind."
Keep in mind that anosognosia is a real thing. It’s a physiological condition where the brain is so damaged it cannot recognize its own impairment. They aren't being stubborn or "in denial." They literally cannot see the problem because the part of the brain that performs self-reflection is broken.
Actionable Next Steps for Families
If you are seeing these warning signs of Alzheimer's, don't panic, but do act. Time is the one thing you can't get back in neurology.
- Document the "Oddities": Keep a private log. Note the date, the time, and exactly what happened. "Mom couldn't remember how to use the microwave at 4 PM" is much more helpful to a doctor than "She's been acting weird."
- Schedule a "Long" Appointment: A standard 15-minute physical isn't enough. Ask for a cognitive screening specifically.
- Check the Meds: Look at their current prescriptions. Some medications (like certain sleep aids or bladder control drugs) have "anticholinergic" effects that can cloud the mind.
- Blood Panels: Ensure the doctor checks B12, folate, and thyroid levels (TSH).
- Look into Clinical Trials: Sites like Antidote or the Alzheimer’s Association TrialMatch can connect you with research that offers access to the newest therapies often years before they hit the general market.
- Assess the Environment: Simplify the home. Remove trip hazards. Improve lighting. If vision is becoming an issue, high-contrast tape on the edge of stairs can prevent a fall.
The path ahead isn't easy, but knowing what you're looking at is the first step toward managing it. Whether it's Alzheimer's or a treatable deficiency, clarity is always better than the "not knowing." Keep an eye on the patterns. Trust your gut. If something feels off, it usually is.