Honestly, the first time a doctor hands you a prescription for Warfarin (Coumadin), it feels a bit like they’re handing you a list of rules that suck the joy out of dinner. You’re told to watch your greens. You’re told to avoid certain oils. Suddenly, a spinach salad feels like a gamble. But here is the thing: food that interfere with warfarin aren't actually "forbidden." It’s a huge misconception that you have to clear out your fridge and live on white bread and processed meat just to keep your INR (International Normalized Ratio) stable.
Blood thinners are finicky.
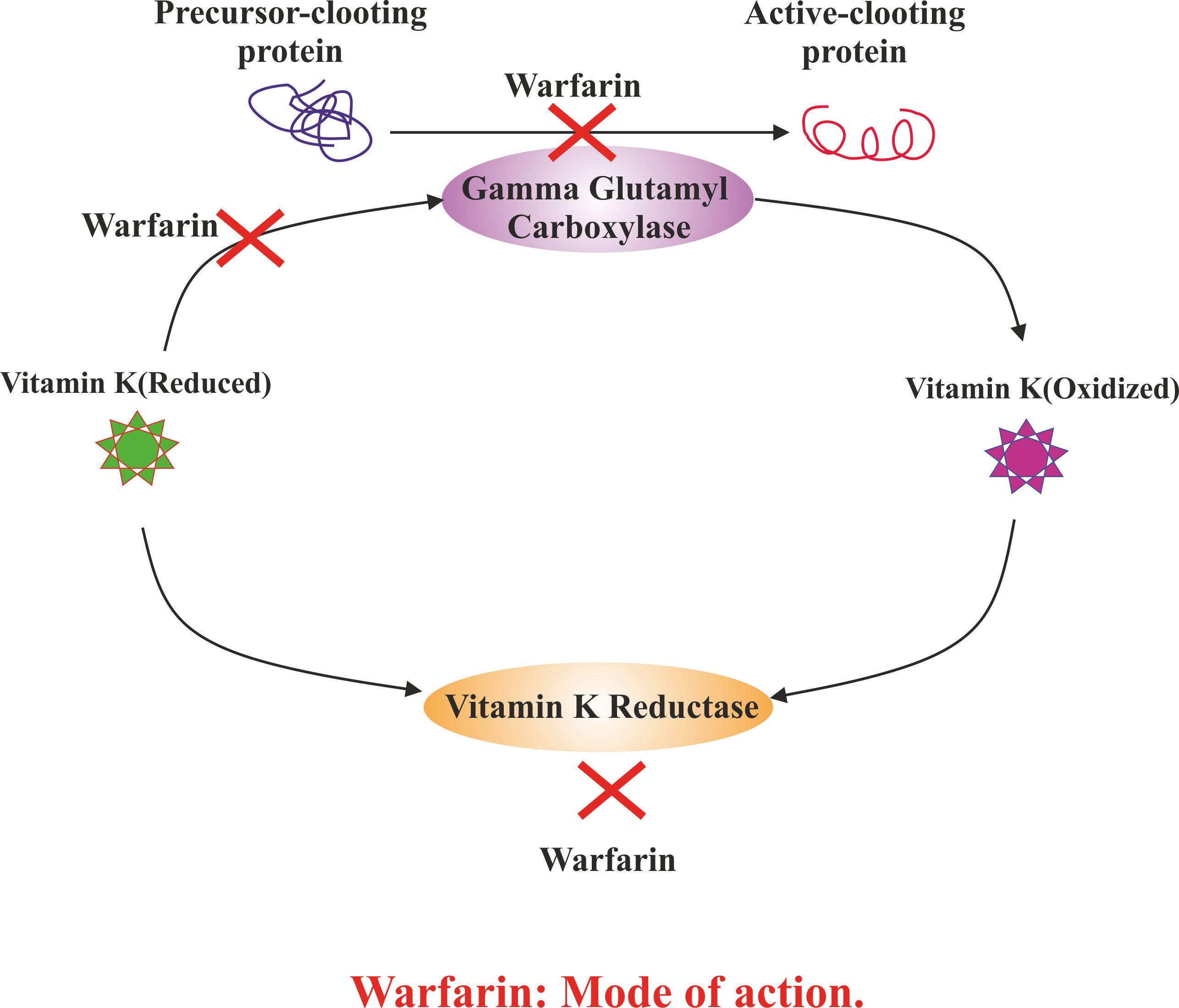
Warfarin works by inhibiting an enzyme called vitamin K epoxide reductase. Basically, it slows down your body's ability to recycle Vitamin K, which is the primary "clotting factor" in your blood. If you flood your system with Vitamin K from food, you're essentially undoing the work the medication is trying to do. It's a tug-of-war. If the food wins, your blood gets too thick, and you're at risk for a stroke or a clot. If the medicine wins by too much because you stopped eating greens entirely, your blood gets too thin, and you might start bleeding from your gums or bruising if someone just brushes against your arm.
The Vitamin K Tug-of-War
Most people think they should just stop eating Vitamin K. That's a mistake.
Doctors and registered dietitians, like those at the Mayo Clinic, actually suggest that the goal isn't "low Vitamin K," it’s "consistent Vitamin K." If you eat a cup of kale every Tuesday, keep eating a cup of kale every Tuesday. Your doctor will adjust your Warfarin dose to match that baseline. The trouble starts when you go on a "health kick" and start drinking green smoothies every morning after a month of eating mostly pasta. Your INR will crater.
The heavy hitters are the leafy greens. We're talking about kale, spinach, Brussels sprouts, and collard greens. These are packed with Vitamin K1 (phylloquinone). Just a half-cup of cooked kale contains over 500 micrograms of Vitamin K, which is way over the daily recommended value for someone on anticoagulants.
But it’s not just the obvious greens.
💡 You might also like: Resistance Bands Workout: Why Your Gym Memberships Are Feeling Extra Expensive Lately
Did you know that certain oils are high in Vitamin K? Soybean oil and canola oil can sneak into your diet through salad dressings and fried foods. If you suddenly switch from an olive oil-based diet to one heavy in soybean oil, you might see a shift in your blood thickness. It’s subtle, but it matters.
Beyond the Greens: The Surprising Culprits
There are food that interfere with warfarin that have nothing to do with Vitamin K. This is where it gets tricky.
Take grapefruit, for example. It’s famous for messing with statins, but it can also impact how your liver processes Warfarin. Cranberry juice is another one that gets a lot of press. For years, the medical community warned that cranberry juice could "potentiate" Warfarin, meaning it makes the drug stronger and increases your bleeding risk. The data is actually a bit mixed—some studies show a significant interaction while others don't—but most hematologists still suggest limiting cranberry juice to no more than eight ounces a day.
Then there’s alcohol.
A glass of wine with dinner usually isn't a crisis. However, binge drinking is a disaster for someone on Warfarin. Heavy alcohol consumption can stress the liver, which is the organ responsible for both metabolizing your medication and producing clotting factors. If your liver is busy dealing with a six-pack of beer, it’s not managing your blood chemistry correctly.
- Garlic and Ginger: In huge, supplemental amounts, these can have a mild anti-platelet effect. Eating a clove in your pasta? Fine. Taking a high-potency garlic pill? Talk to your doctor.
- Green Tea: It contains Vitamin K, but you’d have to drink a massive amount to really swing the needle. Still, if you’re a gallon-a-day iced tea drinker, it’s worth mentioning during your next blood draw.
- Charbroiled Foods: Interestingly, some research suggests that eating a lot of charred or grilled meat can decrease the effectiveness of Warfarin. It’s about the chemicals created during the charring process, not the meat itself.
Why "Consistency" is a Scary Word for Foodies
I've talked to patients who feel like they're under house arrest with their diet. They're terrified to eat a Caesar salad.
📖 Related: Core Fitness Adjustable Dumbbell Weight Set: Why These Specific Weights Are Still Topping the Charts
Let's be real: nobody eats the exact same amount of Vitamin K every day. Life doesn't work like that. You go to a wedding, you eat the asparagus. You go on vacation, you eat differently. The key is to avoid "massive" swings. If your usual diet is a 2 on the Vitamin K scale, don't jump to a 10 for three days straight.
Check your multivitamin, too. Many "One-a-Day" style vitamins contain 25 to 80 micrograms of Vitamin K. If you start or stop a vitamin, your INR will move. This is why pharmacists always ask if you've changed any supplements. Even herbal teas like St. John’s Wort can speed up the breakdown of Warfarin in your body, making the dose you're taking less effective.
Navigating the "Hidden" Risks
It's not just what you eat; it's how your body reacts to it.
If you get a stomach bug and have diarrhea for two days, you’re likely not absorbing your medication or your food properly. Furthermore, the bacteria in your gut actually produce some Vitamin K (Vitamin K2). When you take antibiotics, you kill those bacteria. This is why many people find their INR skyrockets when they’re on a course of amoxicillin or ciprofloxacin. It's a double whammy: you're eating less because you're sick, and your gut bacteria aren't helping you out anymore.
Common foods that interfere with warfarin (The "Watch List"):
- Kale and Spinach: High K.
- Natty/Fermented Soy: Extremely high K2.
- Mango: Some reports suggest it can increase the effect of Warfarin (bleeding risk).
- Avocado: High amounts might decrease Warfarin's effectiveness.
- Sushi: Specifically the seaweed (Nori) wraps, which are dense with Vitamin K.
The complexity of these interactions is why the "Warfarin Clinic" exists. It’s a literal balancing act.
👉 See also: Why Doing Leg Lifts on a Pull Up Bar is Harder Than You Think
Real-World Management Strategies
If you love your veggies, keep them. Seriously.
The healthiest people on Warfarin are often those who eat a high-vegetable diet but do so consistently. Their dose is simply higher to compensate. If you're a "Veggie King," your dose might be 7.5mg, whereas a "Meat and Potatoes" person might only need 2.5mg. Both are equally safe as long as the INR stays in that 2.0 to 3.0 "sweet spot."
- Track your "Big Greens": You don't need a spreadsheet, but just keep a mental note. If you had a big pile of spinach today, maybe skip the broccoli tomorrow.
- Watch the supplements: Don't start CoQ10, Vitamin E, or Fish Oil without checking in. Fish oil can have a mild thinning effect, which adds to the Warfarin.
- Be honest with your nurse: If you spent a week in Mexico eating guacamole and drinking margaritas, tell the person doing your blood draw. They’d rather know why your numbers are off than play a guessing game with your dosage.
- Read labels for "Soybean Oil": It's in everything from mayonnaise to crackers. If you're changing brands, take a quick peek.
The Actionable Path Forward
Managing food that interfere with warfarin isn't about deprivation; it's about awareness. You shouldn't be afraid of your dinner plate.
Immediate Steps to Take:
- Audit your supplements: Look at your multivitamin and any herbal pills. Note the Vitamin K content and tell your doctor the exact dosage.
- Establish a "Baseline" salad intake: Decide how many servings of greens you actually enjoy in a week and try to stick to that number.
- Watch for "The Big Three" symptoms: If you notice nosebleeds, dark/tarry stools, or bruises that appear for no reason, call your clinic immediately. This means the interaction between your diet and medicine has tipped the scales too far.
- Keep a "Warning" card: Always carry a card in your wallet stating you are on Warfarin. In an emergency, doctors need to know your blood won't clot normally, regardless of what you ate for lunch.
Stick to a routine that makes you happy. Your medication should fit your life, not the other way around. Talk to your pharmacist about any new foods you're worried about, but generally, if you keep things moderate and steady, you’ll be just fine.
Stay consistent, stay monitored, and keep eating your dinner.