You’re sitting there, you look down, and your heart skips a beat. It’s dark. Like, midnight dark. Maybe even a little bit shiny. It is one of those moments where your brain immediately goes to the worst-case scenario. Honestly, it’s a terrifying sight if you aren't expecting it. But before you start spiraling into a WebMD-induced panic attack, let’s get real about what is actually happening inside your gut.
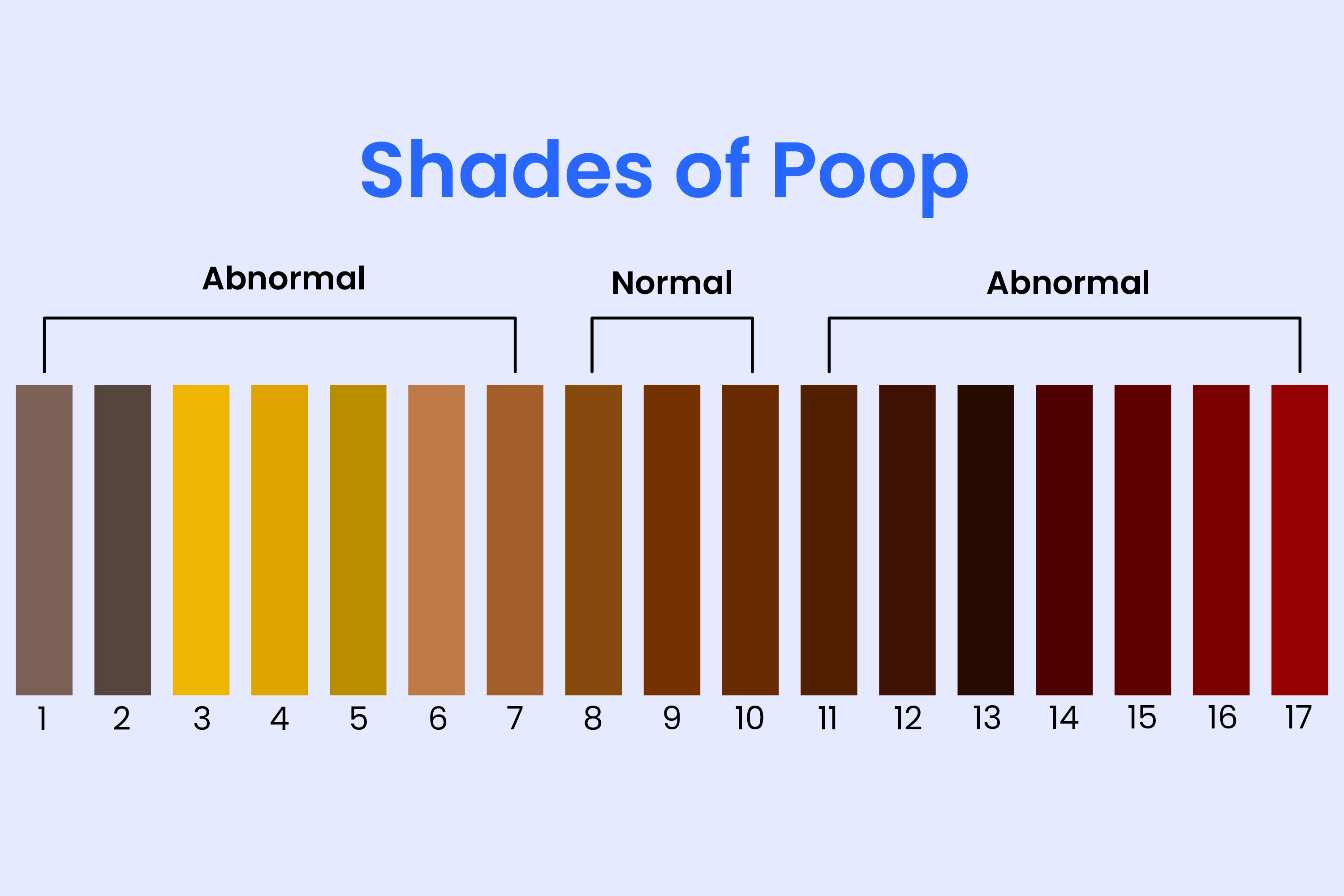
The truth is, what does it mean when your poop is black can range from "I ate too many Oreos" to "I need an emergency room right now." There is very little middle ground. Your stool is basically a daily report card for your digestive system. Usually, it’s a boring shade of brown thanks to bile and broken-down red blood cells. When that color shifts to black, the chemistry of your "output" has changed significantly.
Sometimes it’s just a stain from something you ate. Other times, it’s a sign that blood has been partially digested, turning it into a thick, tarry mess. We’re going to break down the nuances of the "black stool" phenomenon, from the harmless culprits in your pantry to the serious medical red flags that doctors look for in the clinic.
📖 Related: Cuanto es 78 kilos en libras: Why the Math Matters for Your Health
The Most Common (And Harmless) Reasons for Black Stool
Most of the time, this is a food issue. You’d be surprised how much a small amount of pigment can change things. If you’ve been hitting the "superfoods" hard or treating yourself to certain snacks, your bathroom experience might reflect that within 24 to 48 hours.
Take blueberries, for example. If you eat a massive bowl of them, or maybe a pint of blackberry cobbler, don’t be shocked when you see a deep, dark, almost purple-black stool the next morning. It’s just the natural pigments passing through. The same goes for black licorice. Real black licorice—the kind that uses extract from the Glycyrrhiza glabra plant—contains compounds that can dye your waste a very convincing shade of black.
Then there’s the "Oreo effect." It’s a real thing. If you eat a whole sleeve of those chocolate sandwich cookies (no judgment here), the dark cocoa powder used in the cookies can turn your stool pitch black. It’s alarming, but it’s just food coloring. Beets usually turn things red, but in some digestive environments, they can appear much darker, almost like old blood.
Medications and Supplements
This is the big one. If you’re taking iron supplements for anemia, your poop will be black. Period. It’s not a maybe; it’s a physiological certainty. Your body doesn’t absorb all the iron you swallow. The leftover iron oxidizes in your gut, and that oxidation process turns everything a dark, greenish-black. It’s perfectly normal, though it can sometimes cause constipation too.
Bismuth subsalicylate is another culprit. You probably know it as Pepto-Bismol. This stuff is a lifesaver for an upset stomach, but it reacts with the tiny amounts of sulfur in your saliva and digestive tract to create bismuth sulfide. Bismuth sulfide is black. It can even turn your tongue black for a few hours. If you took some pink liquid yesterday and your stool is black today, that is 100% the reason why.
When It’s Not Food: The Medical Reality of Melena
Now we have to talk about the serious side. In the medical world, black, tarry, foul-smelling stool is called melena. This isn’t just a color change; it’s a texture and odor change too.
Melena happens when there is bleeding in the upper gastrointestinal (GI) tract. We’re talking about the esophagus, the stomach, or the first part of the small intestine (the duodenum). When blood is exposed to stomach acid and digestive enzymes, the iron in the blood oxidizes. This turns the blood from bright red to a sticky, black substance that looks a lot like used motor oil or coffee grounds.
The Smell Factor
Honestly, you’ll know melena by the smell. It’s distinct. It’s a metallic, sickly-sweet, incredibly pungent odor that is vastly different from "normal" bad smells. Doctors can often diagnose an upper GI bleed just by walking into the room because the scent is so specific. If your stool is black and it smells significantly worse than usual, that’s a major red flag.
Why Would Your Gut Be Bleeding?
There are several reasons why the upper GI tract might start leaking blood. It’s rarely a "just because" situation. Usually, there is an underlying irritation or a structural issue that needs addressing.
Peptic Ulcers are the most frequent cause. These are open sores on the lining of your stomach or duodenum. They are often caused by an infection with H. pylori bacteria or by the long-term use of NSAIDs like ibuprofen (Advil, Motrin) or naproxen (Aleve). These meds are great for headaches, but they can be brutal on your stomach lining if you take them too often.
Gastritis is another one. This is just a fancy word for inflammation of the stomach lining. It can be caused by alcohol, spicy foods, or even extreme stress. If the inflammation is bad enough, the lining can start to bleed.
Esophageal Varices are more serious. These are swollen veins in the esophagus, usually found in people with advanced liver disease or cirrhosis. If these veins burst, it causes heavy bleeding. This is a medical emergency. You might also vomit blood that looks like coffee grounds in this scenario.
Mallory-Weiss Tears happen when you’ve been vomiting or coughing violently. The pressure causes a small tear in the lining where the esophagus meets the stomach. It bleeds, you digest the blood, and—you guessed it—black poop.
Sorting Through the Symptoms
How do you tell the difference between "I ate blueberries" and "I have a stomach ulcer"? You have to look at the big picture.
If you feel fine, have no pain, and just happened to notice the color, it’s likely dietary. But if the black stool is accompanied by other symptoms, you need to pay attention. Are you feeling dizzy or lightheaded? That could mean you’re losing enough blood to drop your blood pressure. Are you unusually pale? Do you have a gnawing pain in your upper abdomen that gets better or worse when you eat?
Texture Matters
- Dietary Black Stool: Usually maintains a normal, firm consistency. It’s just "painted" black.
- Melena (Blood): Usually sticky, tarry, and "tacky." It’s hard to wipe away. It’s often loose or looks like paste.
The Role of Testing and Diagnosis
If you go to a doctor because you're worried about what does it mean when your poop is black, they aren't just going to take your word for it. They’ll perform a fecal occult blood test (FOBT). This is a quick test where they put a smear of the stool on a special card and add a chemical trigger. If it turns blue, there’s blood in it. Simple as that.
If that test is positive, the next step is usually an endoscopy. A gastroenterologist—basically a plumber for humans—will slide a thin tube with a camera down your throat while you’re sedated. They can see exactly where the bleeding is coming from and often fix it right then and there by cauterizing the wound or clipping a vessel.
Don't Ignore the "Other" Dark Colors
Sometimes people mistake deep green for black. If you’ve been eating a lot of kale, spinach, or taking chlorophyll supplements, your stool might be a "forest green" so dark it looks black in the dim light of a bathroom. A quick trick? Take a bit of the stool on some toilet paper and look at it under bright light. If it has a green tint, it’s just bile moving too fast through your system or a surplus of veggies.
Immediate Action Steps
If you are seeing black stool right now, here is exactly what you should do. No fluff, just the steps.
First, think back over the last 48 hours. Did you take Pepto-Bismol? Did you eat a lot of dark chocolate, blueberries, or beets? Did you start a new iron supplement or a multivitamin? If the answer is yes, stop taking that substance for two days. If the color returns to brown, you have your answer. You're fine.
📖 Related: Butt Plugs and Better Sex: What Most People Get Wrong About Anal Play
Second, check your vitals if you can. If you feel "heart-rolly," dizzy when you stand up, or short of breath, stop reading this and call a doctor. An internal bleed isn't something you can "walk off." It can lead to anemia or shock very quickly.
Third, look at your medication cabinet. If you are on blood thinners like warfarin (Coumadin), clopidogrel (Plavix), or even a daily baby aspirin, you are at a much higher risk for GI bleeding. Even a small irritation can bleed significantly because your blood can’t clot as easily.
When to See a Doctor
- The black stool lasts for more than two days after you've stopped eating "suspect" foods.
- The stool is sticky and tarry like road asphalt.
- You have persistent abdominal pain or cramping.
- You feel weak, fatigued, or faint.
- You are also vomiting (especially if the vomit looks like coffee grounds).
Internal bleeding is sneaky. It doesn't always hurt. You might just feel "off" for a few days before you realize you’re losing blood. It’s always better to get a "false alarm" at the doctor's office than to ignore a slow-bleed ulcer that could eventually perforate your stomach wall.
Final Practical Insights
Basically, don't let a dark stool ruin your week, but don't ignore it either. If you’re a heavy NSAID user—someone who pops ibuprofen every time their back aches—take this as a sign to be careful. Those drugs are amazing for inflammation but they are notorious for thinning the stomach lining.
Switching to acetaminophen (Tylenol) for a while can give your stomach a break. Also, if you do have an ulcer, modern medicine is incredible. A few weeks of a proton pump inhibitor (PPI) like omeprazole can shut down acid production long enough for your body to heal itself completely.
The bottom line? Watch your diet, know your meds, and listen to your gut—literally. If something feels wrong and looks "tarry," get it checked out. Most of the time it’s just the blueberries, but your health is worth the five-minute test at the clinic.