You’re sitting in the doctor’s office. The nurse hands you a printout with rows of numbers. One says your LDL is creeping up, and another shows your Vitamin D levels are “suboptimal.” It’s a classic combo.
Most people look at these two markers as totally separate issues, like a flat tire and a cracked windshield. But the truth is they’re basically cousins. They’re both born from the exact same precursor in your body: acetyl-CoA. In fact, your body uses cholesterol to make Vitamin D. If you don't have enough of the "raw material," or if the conversion process gets gunked up, things start going sideways.
The "Sunlight Hormone" and Your Arteries
Let’s get one thing straight. Vitamin D isn't actually a vitamin. It’s a secosteroid hormone.
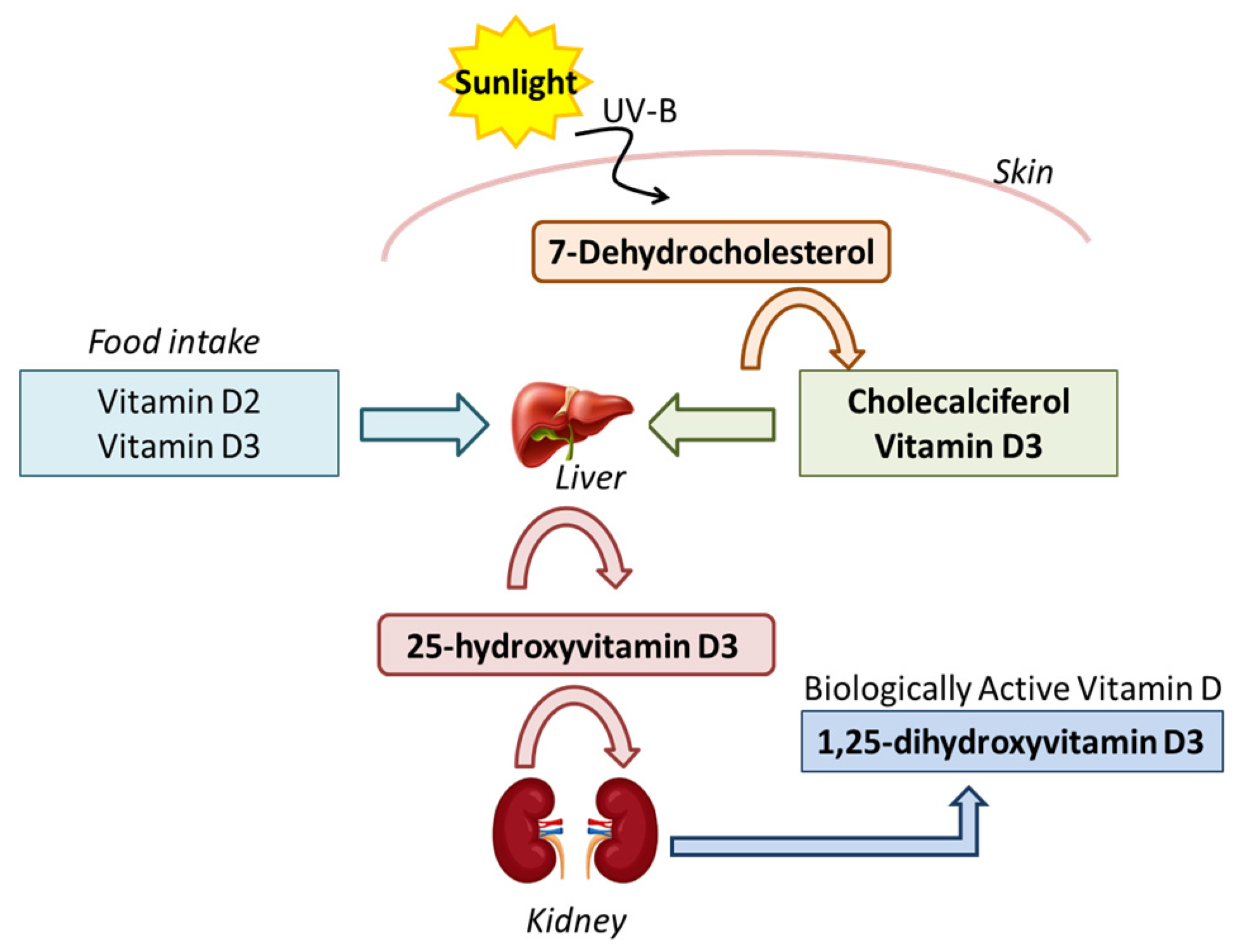
When the sun hits your skin, it reacts with a form of cholesterol called 7-dehydrocholesterol. This turns into Vitamin D3. It’s a beautiful, elegant system. But here’s where it gets weird. Recent studies, including some published in The American Journal of Clinical Nutrition, suggest that when Vitamin D levels are low, the body might actually ramp up cholesterol production as a sort of compensation mechanism. It’s like your body is screaming, "I can't make enough D, so let me hoard more of the ingredients!"
Does this mean taking a pill will magically scrub your arteries clean? Not exactly.
The relationship between vitamin d and cholesterol is messy. In some trials, like the large-scale VITAL study, researchers didn't see a massive drop in heart attacks just from supplementation. However, observational data tells a different story. People with higher Vitamin D levels consistently tend to have better lipid profiles. They have more of the "good" HDL and less of the "bad" triglycerides.
Why Your Statin Might Be Making You D-Deficient
If you’re on a statin, you need to pay attention. Statins work by blocking HMG-CoA reductase. That’s the enzyme responsible for making cholesterol.
Since your body needs that specific cholesterol pathway to synthesize Vitamin D from the sun, some researchers, like those featured in Dermato-Endocrinology, have raised concerns that aggressive statin use might inadvertently lower your Vitamin D levels. It’s a pharmacological catch-22. You’re lowering the "bad" stuff, but you might be accidentally throttling your hormone production.
It’s About Inflammation, Not Just Numbers
Honestly, we focus way too much on the total cholesterol number. What actually matters is how much inflammation is in your system. Vitamin D is a massive anti-inflammatory regulator.
When your D levels are tanked, your immune system gets twitchy. It starts attacking things it shouldn't. This leads to oxidative stress, which turns "normal" LDL cholesterol into "oxidized" LDL. That’s the real villain. Oxidized LDL is what actually gets stuck in your artery walls and forms plaque.
Think of it like this:
- Cholesterol is the wood.
- Inflammation is the match.
- Vitamin D is the fire extinguisher.
Without the extinguisher, that wood is a lot more dangerous.
👉 See also: Small White Bumps Inside Nose: What’s Actually Going On?
The Magnesium Connection Nobody Mentions
You can swallow 10,000 IU of Vitamin D every day and it won't do a lick of good if you’re low on magnesium. This is a huge mistake people make. All the enzymes that metabolize Vitamin D require magnesium as a cofactor.
If you're stressed, drinking too much coffee, or not eating enough leafy greens, you're likely magnesium-deficient. In that case, the Vitamin D just sits in your blood, unused, while your cholesterol remains stubborn. It’s all connected. You can’t pull one string without moving the whole web.
Is Supplementation a Silver Bullet?
I’d love to tell you it’s as simple as popping a gummy. It isn't.
Some meta-analyses have shown that high-dose Vitamin D supplementation actually increased LDL levels slightly in certain populations. Why? Because Vitamin D increases calcium absorption. If that calcium isn't directed to your bones (usually because you’re low on Vitamin K2), it can end up in your soft tissues and potentially mess with lipid metabolism.
You have to be careful. More isn't always better. The "sweet spot" for most people is a blood level between 40 and 60 ng/mL. Anything higher doesn't seem to provide extra heart benefits and might even cause issues with calcium signaling in the heart muscle.
Genetics and the VDR Gene
Sometimes, you do everything right and the numbers still won't budge. This is where the Vitamin D Receptor (VDR) gene comes in.
Some people have polymorphisms—basically "glitches"—in their VDR gene that make them less efficient at using the Vitamin D they have. These people might need much higher doses to see any change in their cholesterol or blood pressure. If you’ve been supplementing and your blood levels won't rise, your genetics might be the culprit.
Practical Steps to Balance Your Levels
Stop looking at these as separate problems. Start treating your metabolic health as a single ecosystem.
- Get a full panel, not just a "total cholesterol" check. Ask for NMR LipoProfile to see the particle size of your LDL. Small, dense particles are the ones linked to low Vitamin D and high risk.
- Test your 25(OH)D levels. Don't guess. You want to know exactly where you are before you start megadosing.
- Prioritize Vitamin K2 (MK-7). If you take Vitamin D to help your heart and cholesterol, you MUST take K2. K2 acts like a traffic cop, making sure the calcium Vitamin D absorbs goes into your bones and not your arteries.
- Eat the precursors. Wild-caught salmon, sardines, and egg yolks from pastured chickens. These contain both the healthy fats your body needs for cholesterol synthesis and the Vitamin D itself.
- Sunlight is superior. Supplements are a backup. 15 minutes of midday sun on your torso provides more usable Vitamin D than most pills, and it doesn't have the same risk of toxicity because the body has built-in "shut off" mechanisms for sun-produced D.
The Bottom Line on Vitamin D and Cholesterol
The link between vitamin d and cholesterol is a two-way street. Low Vitamin D can lead to higher cholesterol and increased inflammation, while low cholesterol (often caused by medication or extreme diets) can lead to a Vitamin D deficiency.
If you’re worried about your heart, don't just chase the cholesterol number down to zero. Focus on getting your Vitamin D into the optimal range, managing inflammation with magnesium and K2, and moving your body. Your lipids will usually follow suit once the underlying hormonal environment is fixed.
To take action today, check your latest blood work. If your Vitamin D is under 30 ng/mL and your triglycerides are over 150 mg/dL, talk to a functional medicine practitioner about a targeted protocol involving D3, K2, and Magnesium glycinate. Monitor your levels every three months to find your specific "set point."