It happens fast. One minute a nurse is checking an IV line, and the next, she’s pinned against a wall or ducking a flying kidney dish. You’d think hospitals would be the safest places on earth, right? Places of healing and all that. But the reality is getting ugly. Violence against healthcare workers has shifted from a "rare occurrence" to a daily expectation for people in scrubs. Honestly, it’s a mess. If you talk to any veteran ER nurse, they probably have a story about a bruise, a bite, or a death threat that they just "shrugged off" because they had ten other patients waiting.
This isn't just about "difficult patients" or someone being cranky because the hospital cafeteria ran out of turkey sandwiches. We are talking about systematic, escalating physical and verbal assaults. According to the U.S. Bureau of Labor Statistics, healthcare workers are five times more likely to experience workplace violence than employees in any other private industry. That is a staggering gap. It’s not just a "part of the job," though for decades, the culture of medicine basically told doctors and nurses to suck it up.
The Reality of Violence Against Healthcare Workers in 2026
The numbers don't lie, but they also don't tell the whole story. While OSHA and the American Hospital Association track these incidents, most experts agree the data is massively underreported. Why? Because filling out a 10-page incident report after a 12-hour shift feels like a punishment. Nurses are tired. Doctors are burnt out.
Take a look at the psychiatric wards and emergency departments. These are the flashpoints. In these high-stress environments, a mix of substance abuse, untreated mental health crises, and sheer desperation creates a powder keg. A study published in The Journal of Emergency Nursing highlighted that a vast majority of emergency nurses have been victims of physical or verbal abuse in the last year alone. It’s a silent epidemic. People are leaving the profession in droves, not because they don't love medicine, but because they’re tired of being punched in the face for $35 an hour.
Why is this happening now?
It’s easy to blame the pandemic, but that’s a bit of a cop-out. The seeds were sown long before 2020. We have a mental health system that is, frankly, broken. When patients can't get long-term psychiatric care, they end up in the ER. The ER isn't designed for long-term psych holds. It’s loud, bright, and chaotic—basically the worst possible environment for someone in a sensory-overloaded crisis.
🔗 Read more: X Ray on Hand: What Your Doctor is Actually Looking For
Then there’s the "customer service" aspect of modern medicine. When hospitals started being rated like hotels on TripAdvisor, the power dynamic shifted. Patients (and their families) sometimes feel entitled to immediate results, and when the wait time hits six hours, frustration turns into aggression. You've probably seen it. A family member screaming at a receptionist because a physician is tied up in a trauma code. It's a pressure cooker.
The Types of Abuse Nobody Wants to Discuss
We usually think of violence as a punch or a kick. Those are easy to categorize. But violence against healthcare workers includes a lot of "gray area" behavior that erodes a person's soul over time.
- Verbal Harassment: This is the constant drone of insults, racial slurs, and sexual comments. It’s constant.
- Stalking: With the internet making it easy to find anyone, some patients track down their providers on social media. It’s terrifying.
- Lateral Violence: This is the "nurse eating their young" phenomenon. It’s bullying within the ranks, often exacerbated by the high-stress environment of external violence.
- Physical Assault: Spitting, biting, scratching, and the use of improvised weapons like pens or chairs.
Think about the "silent" victims here. It's not just the person who got hit. It’s the other patients who hear the screaming and feel less safe. It’s the new nursing student who decides on day three that they’d rather work in tech. We are losing talent because we can't guarantee basic physical safety.
Legislation and the "SAVE Act"
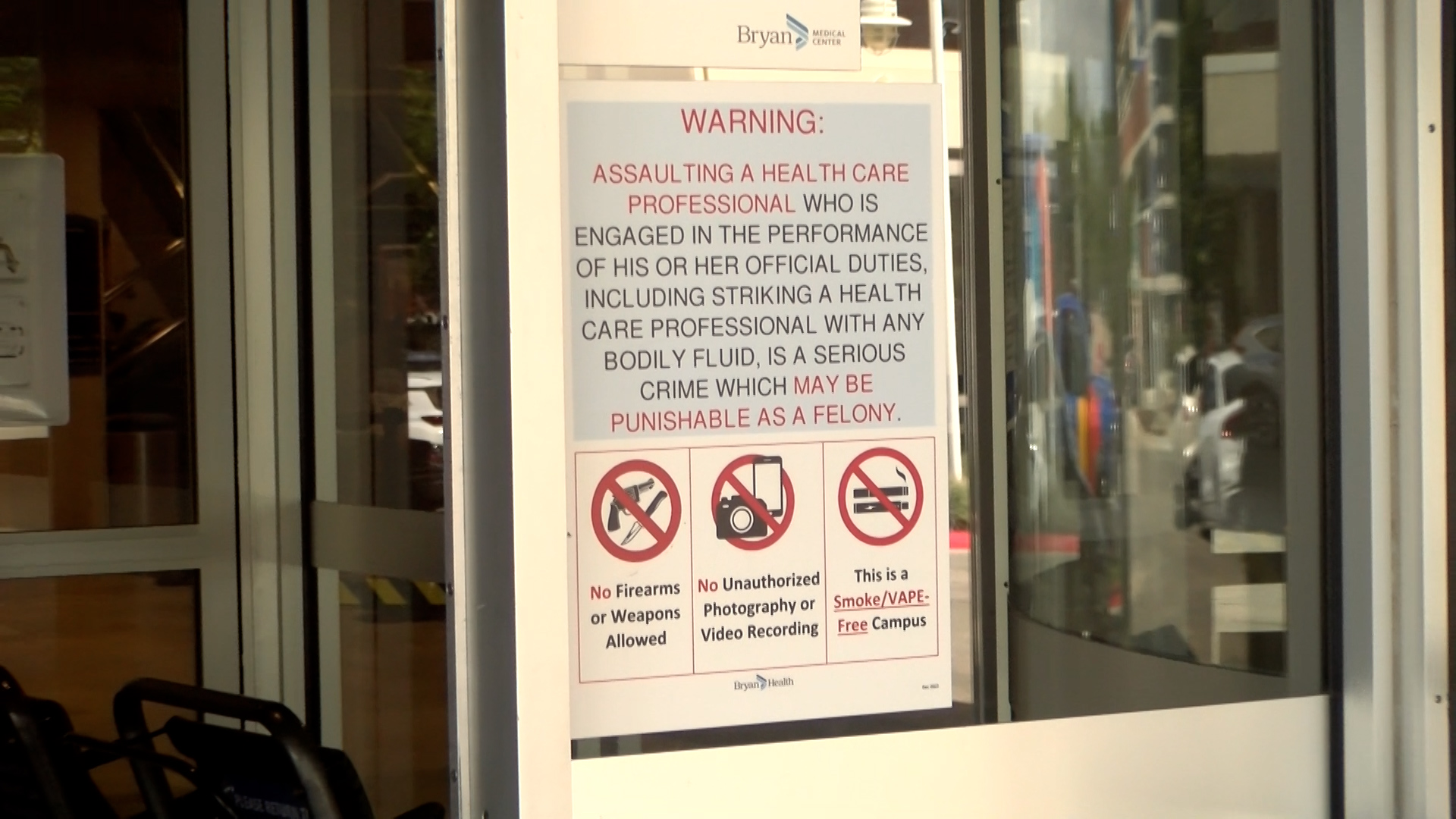
There is some movement on the legal front, though many argue it's too little, too late. The Safety from Violence for Healthcare Employees (SAVE) Act is a big one. It's modeled after protections for airline employees. You know how it’s a federal crime to mess with a flight attendant? The SAVE Act wants to bring that same level of "don't even think about it" to the hospital floor.
💡 You might also like: Does Ginger Ale Help With Upset Stomach? Why Your Soda Habit Might Be Making Things Worse
- Federal criminal penalties for assaulting hospital workers.
- Grants for hospitals to beef up security, like panic buttons and metal detectors.
- Requirements for better de-escalation training.
Some critics argue that criminalizing patients with mental illnesses isn't the answer. And they have a point. If someone is in a florid psychosis, a federal law isn't exactly a deterrent. However, for the "visitor" who decides to deck a nurse because they’re annoyed by the visiting hours, the law provides a much-needed stick.
What Most People Get Wrong About Hospital Security
You see a security guard at the front desk and think, "Okay, we’re covered." Not really. Most hospital security guards are unarmed and, in many cases, are instructed not to engage physically unless absolutely necessary to prevent a death. They are often "observe and report" staff.
The real "security" often falls on the "lift team" or the male nurses who get paged to "Room 4" whenever a patient gets rowdy. This is an unfair burden. It turns caregivers into bouncers.
Hospitals are starting to experiment with more "hard" security measures. Think canine units in the lobby or permanent police substations inside the building. It’s a sad state of affairs when a place of healing starts looking like a correctional facility, but for many workers, it’s the only way they feel they can get through a shift.
📖 Related: Horizon Treadmill 7.0 AT: What Most People Get Wrong
The Psychological Toll: Moral Injury
We need to talk about Moral Injury. This isn't just "stress." Moral injury happens when a healthcare worker is forced to endure or witness acts that transgress their deeply held moral beliefs. Being forced to care for an abusive patient while you’re bleeding or shaking from an assault is a specialized kind of trauma. It leads to PTSD, substance abuse, and, tragically, high rates of suicide within the medical community.
How to Actually Fix This (Moving Beyond Awareness)
"Awareness" is a buzzword that usually means doing nothing while feeling good about it. We are past awareness. We need structural change. This means hospitals have to stop treating violence as an "occupational hazard."
Concrete Steps for Facilities
- Mandatory Reporting: No more "did you fill out the form?" Make reporting automatic and supported by management.
- Zero-Tolerance Policies with Teeth: If a visitor is abusive, they are removed. Period. No "customer service" apologies from the C-suite.
- Environmental Design: Use "Crime Prevention Through Environmental Design" (CPTED). This means better lighting, fewer blind spots, and furniture that can’t be easily thrown.
- Staffing Levels: Violence goes up when staffing goes down. When a nurse has eight patients, they can't monitor the one who is getting agitated. Proper staffing is a safety feature.
Advice for Healthcare Workers
If you are in the trenches, you've got to protect yourself because, frankly, the system might not.
- Trust your gut. if a room feels "off," don't go in alone. Wait for a colleague.
- Learn De-escalation. Organizations like the Crisis Prevention Institute (CPI) offer training that actually works. It’s about body language, tone, and knowing when to back out.
- Document everything. Even the "small" stuff. If a patient threatens to find you in the parking lot, that goes in the chart and an incident report.
- Demand debriefing. After a violent event, the team needs to talk. Not a "what did you do wrong" meeting, but a "how are we doing" meeting.
What You Can Do as a Patient or Family Member
It sounds simple: be kind. But it's more than that. It's about recognizing that the person in the scrub top is a human being with a family and a nervous system. If you see someone being abusive to a healthcare worker, don't just film it—report it to security. Advocate for your loved ones, but remember that the nurse isn't the one who decided the MRI machine is broken or that the doctor is stuck in surgery.
The healthcare system is leaning on the altruism of its workers to keep the lights on. But altruism doesn't stop a bullet or a fist. We are at a breaking point where the very people we need to save us are the ones who need saving.
Actionable Next Steps for Healthcare Leaders:
- Audit your current incident reporting system: If it takes more than 5 minutes to report an assault, your staff won't do it. Simplify the tech.
- Implement "Code Grey" (or equivalent) response teams: Ensure these teams are trained in trauma-informed care and physical intervention that prioritizes the safety of both staff and patients.
- Publicly support your staff: Display clear signage stating that violence and verbal abuse will lead to removal and prosecution. Back this up when it happens, even if the aggressor is a "VIP" or a donor.
- Invest in mental health support specifically for workplace trauma: General EAP programs are often insufficient for the specific trauma of being assaulted at work.