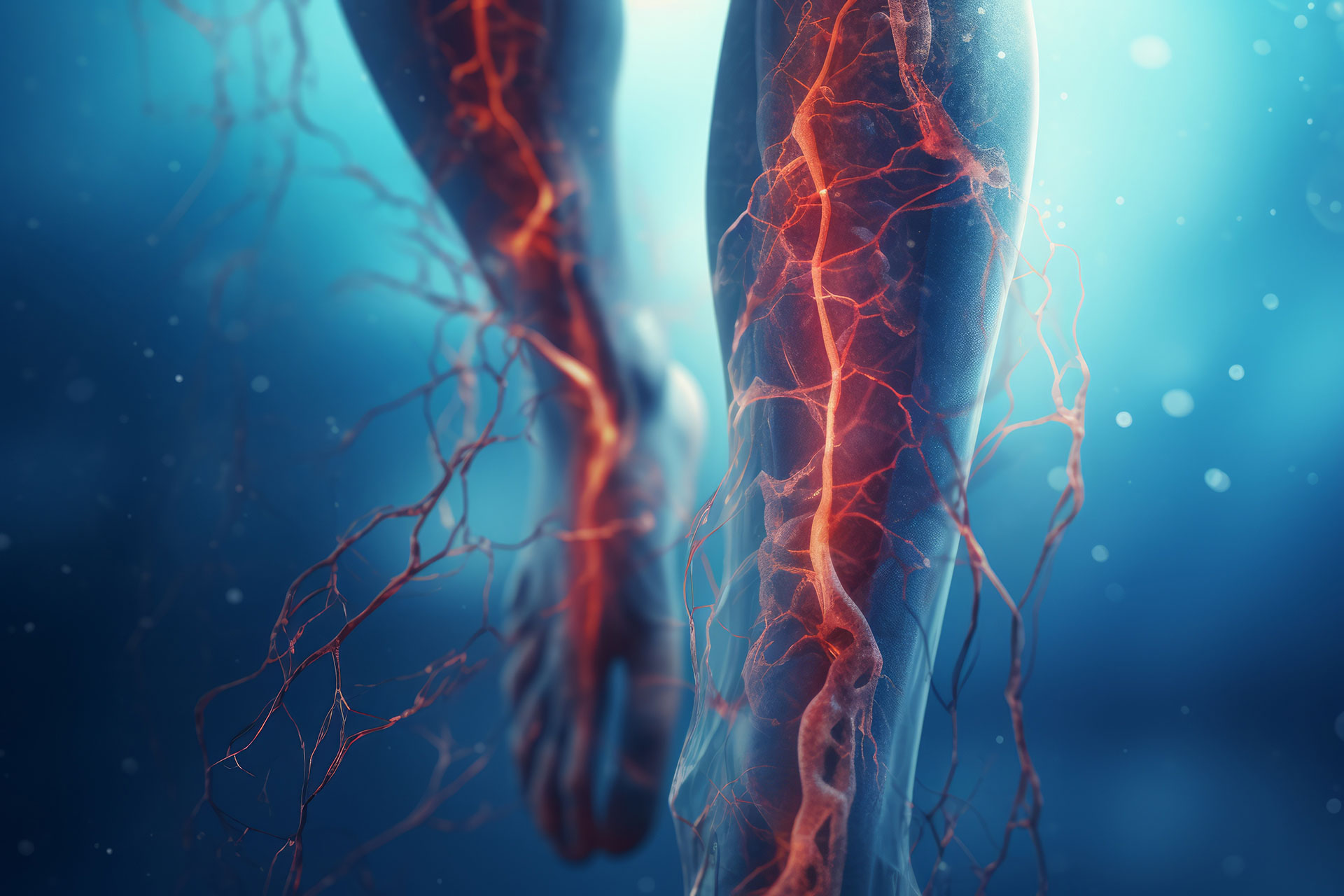
Leg pain is weird. One day you're fine, and the next, your calves feel like they're filled with lead weights after a simple walk to the mailbox. Most people just blame "getting older" or maybe a tough workout. They ignore the swelling. They ignore those tiny, spider-like purple webs creeping up their ankles. Honestly, that's exactly how serious vascular issues fly under the radar until they become genuine emergencies.
If you are looking into Vascular Care of Greenville, you aren't just looking for a clinic; you're likely trying to figure out why your circulatory system is acting like a clogged kitchen pipe. In South Carolina, we see a lot of this. It’s the heat, the diet, the sedentary desk jobs—it all adds up. But here is the thing: vascular health isn't just about "bad veins." It is a complex highway system of arteries and veins that keeps your heart from working itself to death.
The Real Difference Between Arteries and Veins
People mix these up constantly.
Arteries are the high-pressure hoses. They carry oxygen-rich blood away from your heart to your toes. When they get blocked (Peripheral Artery Disease, or PAD), it’s a plumbing nightmare that can lead to things no one wants to talk about, like ulcers or even amputation. On the flip side, veins are the return trip. They have the hard job of fighting gravity to get blood back up to your chest. When the little valves inside those veins fail, blood pools. That is where you get those bulging varicose veins that look like a bag of marbles under your skin.
It’s not just a cosmetic thing. It’s a pressure problem.
Why Vascular Care of Greenville Matters Right Now
Living in the Upstate means we have access to some of the best medical tech in the country, but the "wait and see" approach is still killing people. Literally. When you look at the specialized services at a place like Vascular Care of Greenville, you're seeing a focus on minimally invasive stuff. We aren't in the 1980s anymore. You don't necessarily need a massive "vein stripping" surgery that keeps you in bed for a month.
Most modern procedures are "in and out."
Take Radiofrequency Ablation (RFA). It sounds like sci-fi, but basically, a doctor uses a tiny bit of heat to seal off a bum vein. Your body, being pretty smart, just reroutes the blood to healthy veins. You walk out with a band-aid. That’s it. If you’ve been putting off a consultation because you’re scared of the "knife," you’re living in the past.
💡 You might also like: Can I overdose on vitamin d? The reality of supplement toxicity
Peripheral Artery Disease: The Silent Threat
PAD is the one that keeps vascular surgeons up at night. It’s sneaky. It usually starts as claudication—that’s just a fancy word for cramping when you walk that goes away when you stop.
Dr. Joseph Zarge and other experts in the field have pointed out for years that PAD is a massive red flag for your heart. If the arteries in your legs are narrowed by plaque, what do you think the arteries in your heart look like? They're all part of the same pipe system. In Greenville, we have a high incidence of diabetes and hypertension, which are like rocket fuel for PAD.
If your feet are always cold, or if a small scratch on your toe won't heal after two weeks, you need to stop reading this and call a specialist. Seriously.
The Deep Vein Thrombosis (DVT) Scare
We’ve all heard the horror stories about blood clots after long flights. DVT is a clot in the deep veins, usually the leg. The danger isn't just the clot itself; it's the chance that a piece breaks off and travels to your lungs. That’s a Pulmonary Embolism. It can happen fast.
Vascular Care of Greenville focuses heavily on screening for these. They use duplex ultrasound—non-invasive, doesn't hurt, just some cold jelly and a probe—to see exactly how the blood is flowing. If you have sudden swelling in just one leg, that is a "go to the ER" situation, not a "make an appointment for next Tuesday" situation.
What a Typical Visit Actually Looks Like
Honestly, your first visit to a vascular specialist is pretty boring, which is a good thing.
- The Physical: They’ll check your pulses. Not just your wrist, but your ankles and behind your knees. If they can't find a pulse in your foot, that's a data point.
- The Ultrasound: This is the gold standard. You'll lay on a table while a technician looks at the "weather map" of your blood flow. Blue is one way, red is the other.
- The ABI Test: The Ankle-Brachial Index. They compare the blood pressure in your arm to the pressure in your ankle. It’s a simple math equation. If the ratio is off, you’ve got a blockage.
It’s not intimidating. It’s just diagnostic.
📖 Related: What Does DM Mean in a Cough Syrup: The Truth About Dextromethorphan
Misconceptions About Varicose Veins
"It's just for vanity."
Wrong.
While many people want them gone because they look "gross" in shorts at Unity Park, the underlying cause is often Chronic Venous Insufficiency (CVI). If left alone, the skin around your ankles can turn dark, leathery, and eventually crack open into a venous ulcer. Those are incredibly hard to heal. Treating the "ugly" vein now is actually preventative medicine for a much nastier problem down the road.
Also, insurance usually covers it.
If you have symptoms—aching, heaviness, swelling—most insurance providers, including Medicare, recognize that this isn't "cosmetic." It's a functional medical issue.
The Greenville Lifestyle Factor
We love our food here. Barbecue, biscuits, the whole nine yards. But the high-sodium, high-fat lifestyle is a direct assault on your vascular lining (the endothelium). When you combine that with the humidity that makes your legs swell anyway, it’s a perfect storm.
Vascular specialists in the Upstate aren't just there to do surgery. They’re there to manage your "statin" medications, help you with smoking cessation (smoking is the absolute worst thing you can do for your arteries), and monitor your progress.
👉 See also: Creatine Explained: What Most People Get Wrong About the World's Most Popular Supplement
A Note on Aneurysms
Abdominal Aortic Aneurysms (AAA) are the "silent killers" of the vascular world. It's a bulge in the main pipe leaving your heart. Most people have zero symptoms until it ruptures.
Current guidelines suggest that if you are a male between 65 and 75 and have ever smoked, you should get a one-time ultrasound screening for AAA. It takes ten minutes. It could literally save your life. Greenville clinics have seen a massive uptick in these screenings because they’re so effective at catching problems before they become catastrophes.
How to Take Action
You don't need to be a marathon runner to have healthy veins, but you do need to be proactive.
Start moving. Even if it's just a 10-minute walk around the block. The calf muscle acts as a "second heart." When it contracts, it squeezes the veins and pushes blood back up to your torso. If you sit all day, that blood just sits there too.
Compression is your friend. If you work on your feet at one of the hospitals or manufacturing plants in Greenville, buy some graded compression socks. They aren't your grandma’s stockings anymore; they make them in cool athletic styles now.
Watch the salt. Sodium makes you retain water, which increases the volume of your blood and puts more pressure on those vein valves.
Get a screening. If you have a family history of stroke, heart attack, or "bad legs," go see a professional.
Vascular Care of Greenville and similar specialized centers are designed to handle everything from minor spider veins to complex arterial reconstructions. The goal is always the same: keep the blood moving. Because when the blood stops, the trouble starts.
Don't wait for the pain to become unbearable. If your legs feel heavy at the end of the day, or if you're seeing changes in your skin color, that is your body's way of sending a distress signal. Listen to it. Schedule an ultrasound, talk to a specialist about your ABI scores, and get a baseline of where your circulatory health stands. It is much easier to clear a small clog now than to replace a whole pipe later.