You’re sitting in the doctor’s office, or maybe you just logged into your patient portal at 11:00 PM. You click the PDF, and there it is—a wall of acronyms and numbers that looks like a stock market ticker for your veins. The complete blood count chart is easily the most common blood test on the planet, yet most of us just glance at the "high" or "low" flags and start spiraling on Google.
It's overwhelming. Honestly, it's designed to be read by machines and pathologists, not necessarily by someone just looking for why they've been feeling sluggish lately.
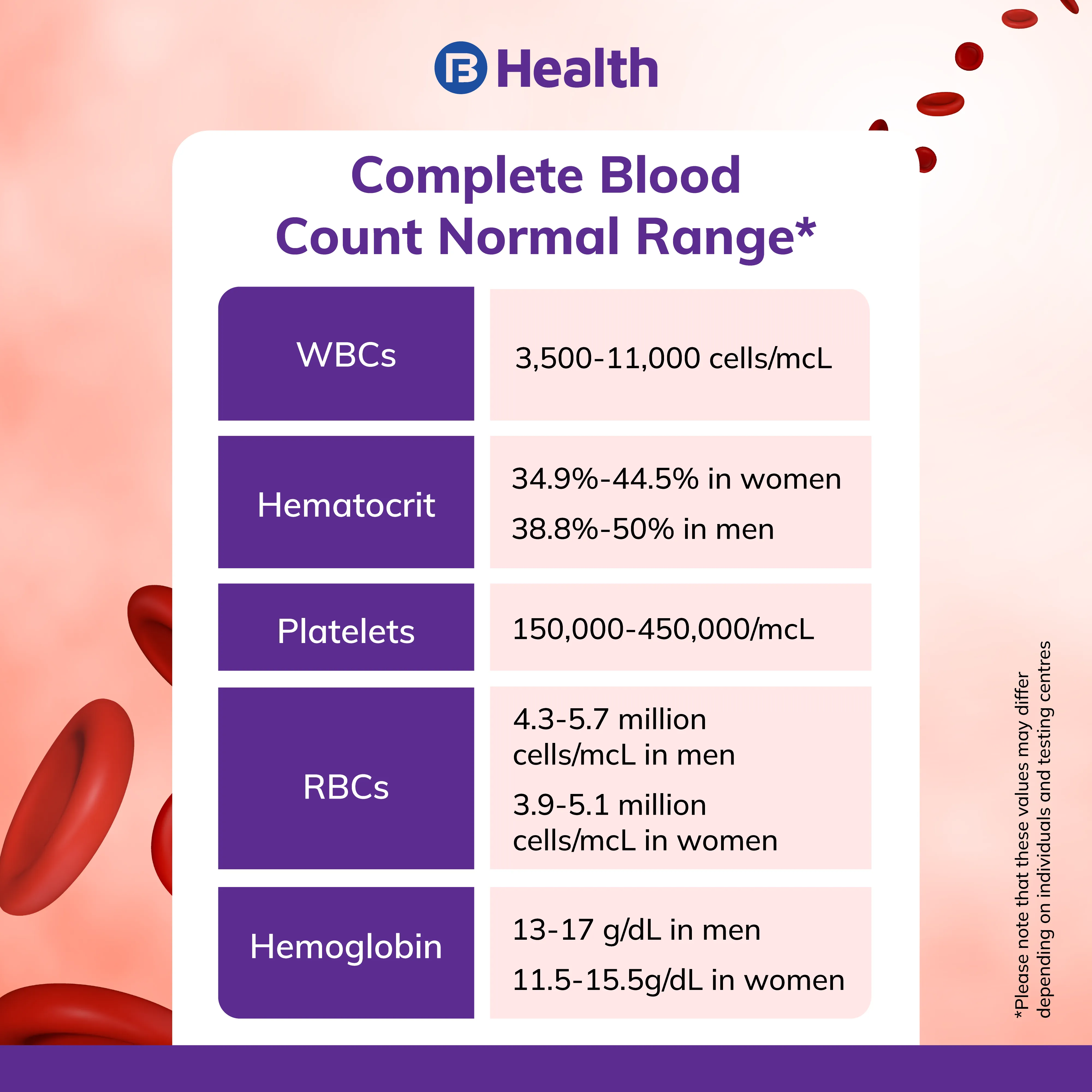
A CBC isn't just one test. It’s a snapshot of your immune system, your oxygen transport, and your clotting ability. It’s a liquid biopsy of your bone marrow’s performance. But here’s the thing: those "normal" ranges you see on the side? They aren't universal laws. They are averages based on the specific population that lab usually tests. Your "normal" might be someone else's "red flag."
Why the Red Blood Cell Section Matters More Than You Think
Most people skip straight to the hemoglobin. I get it. It’s the big one. Hemoglobin is the protein that actually hauls oxygen from your lungs to your toes. If it's low, you're looking at anemia. But if you look closer at your complete blood count chart, there are these weird little markers called MCV, MCH, and RDW.
MCV stands for Mean Corpuscular Volume. Basically, it’s the size of your red cells. If your hemoglobin is low and your MCV is also low, your cells are tiny. This usually screams iron deficiency. But if your MCV is high? Your cells are oversized. That often points to a Vitamin B12 or folate issue. It’s like a detective story where the size of the footprints tells you who the culprit is.
Then there’s the RDW (Red Cell Distribution Width). This measures the variation in size. If all your cells are the same size, RDW is low. If you have a mix of tiny new cells and big old ones, RDW goes up. A high RDW is often the very first sign of a developing nutritional deficiency, even before your hemoglobin drops into the "anemic" range. It's the early warning system most people ignore because it doesn't always have a scary red flag next to it.
Hematocrit is another one that trips people up. It’s just the percentage of your blood that is made of red cells. If you’re dehydrated, your hematocrit might look high because there’s less fluid (plasma) to dilute the cells. You aren't suddenly a super-athlete with extra blood; you just need a glass of water.
The White Blood Cell Mystery: It's Not Just About Infection
White Blood Cells (WBCs) are your internal security team. A total WBC count is helpful, sure, but the "differential" is where the real data lives. This breaks the total count down into five specific types of cells: Neutrophils, Lymphocytes, Monocytes, Eosinophils, and Basophils.
Neutrophils are the first responders. They go after bacteria. If they are high (neutrophilia), your body is likely fighting an active bacterial infection or dealing with significant physical stress.
Lymphocytes are the specialized agents. They handle viruses and create antibodies. Interestingly, according to Dr. Bernie Horowitz and many hematologists, a low lymphocyte count can sometimes be a marker of chronic stress or certain autoimmune issues, not just an acute "flu."
- Eosinophils: These guys usually rise during allergic reactions or if you have a parasite.
- Monocytes: These are the "garbage collectors." They show up to clean up debris after an injury or during chronic inflammation.
- Basophils: These are the rarest. If these are high, it’s often a sign of a more complex inflammatory response or, rarely, a bone marrow issue.
If you see a "Left Shift" mentioned in your lab notes, don't panic. It’s just medical jargon. It means your bone marrow is pumping out immature neutrophils (called bands) because it's trying to fight an infection so hard it can't wait for the cells to fully grow up.
Platelets and the "Invisible" Clotting Factor
Platelets are the smallest things on your complete blood count chart, but they’re the reason you don't bleed out from a papercut. The range is huge—usually 150,000 to 450,000 per microliter.
If your count is 145,000, your doctor might not even mention it. Why? Because platelet counts are notoriously jumpy. Intense exercise, certain medications, or even how the blood was drawn can cause a slight dip. However, if they drop significantly (thrombocytopenia), you might notice easy bruising or those tiny purple spots on your skin called petechiae.
On the flip side, high platelets (thrombocytosis) can happen because of inflammation. Your body sees inflammation and thinks, "Hey, we might be wounded, better make more glue!" Chronic iron deficiency can also weirdly drive platelet counts up. It’s the body’s way of trying to compensate for the lack of healthy red cells.
Common Misconceptions That Mess With Your Head
I see this all the time: people see one number slightly outside the bolded "Reference Range" and assume the worst.
👉 See also: Meds for Kidney Stones: What Actually Works and What’s a Waste of Money
Lab ranges are statistical. If a lab tests 1,000 healthy people, they set the range so that 95% of them fall inside it. That means, by definition, 5% of perfectly healthy people will be "out of range."
Also, your "baseline" matters. If your WBC count has been 4.2 for the last ten years, and suddenly it's 10.5, that’s a massive jump for you, even if 10.5 is technically within the lab's "normal" limit. This is why keeping your old lab reports is so vital. You aren't looking for a single point in time; you’re looking for a trend.
Different labs also use different equipment. A CBC done at Quest Diagnostics might have slightly different "normal" cut-offs than a CBC done at a local hospital or through a finger-prick test at a wellness clinic. Comparing results between different labs is like comparing Celsius and Fahrenheit without a calculator—it just causes unnecessary stress.
Real-World Factors That Skew Your Results
Smoking can permanently raise your hemoglobin and hematocrit because your body is constantly starved for oxygen and tries to overcompensate. High altitude does the same thing. If you live in Denver, your complete blood count chart will look different than if you live in Miami.
Pregnancy is another huge variable. Blood volume expands massively during pregnancy, which often "dilutes" the red blood cells. This is called physiological anemia of pregnancy. It’s expected, yet it still scares parents-to-be every single day when they see that "Low" flag on their portal.
Even the time of day matters. Some studies, including research published in the Journal of Clinical Pathology, suggest that certain white blood cell levels fluctuate based on your circadian rhythm. Stress, recent surgery, and even a particularly grueling workout the day before the blood draw can send your neutrophils into a temporary spike.
Actionable Steps for Your Next Blood Test
Don't just look at the colors on the screen. Take these steps to actually use your data:
🔗 Read more: Does Trump Have an LVAD? What Most People Get Wrong
1. Request the "CBC with Differential"
Standard CBCs just give you the totals. The differential breaks down the white blood cells. It’s usually the same price or a negligible difference, but it provides 5x the diagnostic value.
2. Hydrate before the needle
Being dehydrated can artificially concentrate your blood. This makes your red cell count and hemoglobin look higher than they actually are. Drink sixteen ounces of water an hour before your appointment.
3. Contextualize the "Low" markers
If your hemoglobin is slightly low but your Ferritin (iron stores) and B12 are normal, it might just be your personal baseline. Ask your doctor, "Is this low for the lab, or is this low for me compared to last year?"
4. Check the RDW first
If you're feeling tired but your hemoglobin is "fine," look at the RDW. If it's creeping up toward the high end of the range (usually above 14.5% or 15%), you might be in the early stages of a deficiency that hasn't fully crashed your system yet.
5. Avoid the "Google Trap"
A single abnormal value on a CBC almost never means something catastrophic. Doctors look for patterns. They look at how the MCV interacts with the MCH. They look at the ratio of Neutrophils to Lymphocytes (the NLR ratio), which is becoming a popular way to measure systemic physiological stress.
Next time you get your results, print them out. Put them in a folder. Over the years, you’ll see the rhythm of your own biology. That’s the real power of the complete blood count chart—not just a one-time "pass/fail" grade, but a long-term map of your health.
If you see something that genuinely concerns you, like a WBC count that has doubled since your last check or a platelet count that has plummeted without explanation, don't wait. Call the office and ask for a "nurse callback" to explain the clinical significance. Most of the time, there’s a simple explanation involving a recent cold or a lifestyle shift you didn't even think was relevant.