You’re sitting in that crinkly paper-covered chair at the doctor's office, and the cuff starts squeezing your arm. It gets tight. Almost uncomfortable. Then, you hear the psshhhh of the air escaping. The nurse mutters "122 over 82" and scribbles it down. But what does that actually signify for your life? Honestly, most people just nod and figure if the doctor isn't panicked, they shouldn't be either. But knowing what systolic and diastolic mean is basically like having the password to your own cardiovascular health.
Blood pressure isn't just a static number. It’s a dynamic measurement of the force your blood exerts against your artery walls. Think of your heart as a high-performance pump and your arteries as the pipes. If the pressure in those pipes is too high for too long, things start to leak, burst, or clog.
The Top Number: Why Systolic Is the Big Squeeze
The first number in the pair is the systolic pressure. It’s the higher of the two. Why? Because it represents the maximum pressure your heart generates when it beats.
When your left ventricle contracts, it pushes blood out into the aorta. This is the "work" phase of the cardiac cycle. If you were to touch your pulse right now, that little "thump" you feel is the systolic pressure wave. It's the peak. Medical experts, like those at the American Heart Association (AHA), keep a close eye on this number because it’s often a better predictor of risk for stroke and heart disease as we age. Our arteries tend to stiffen up over the decades, and that stiffness shows up first in the systolic reading.
If your systolic is high, your heart is working overtime. It’s like trying to force water through a garden hose that someone is stepping on. Eventually, the pump wears out.
The Bottom Number: Diastolic and the Quiet Rest
Then there’s the second number. The diastolic. This is the pressure in your arteries when your heart is resting between beats.
It’s easy to think of this as the "lesser" number, but it’s vital. This is when your heart muscle actually gets its own blood supply through the coronary arteries. If the diastolic pressure is too high, it means even when your heart is trying to relax, the pipes are still under significant stress.
🔗 Read more: Creatine Explained: What Most People Get Wrong About the World's Most Popular Supplement
Imagine a balloon. If you blow it up, the pressure is high. If you let some air out but keep the nozzle pinched, there's still tension in the rubber. That’s your diastolic pressure. It never drops to zero. If it did, your blood would stop moving entirely, which is obviously a bad Saturday for everyone involved.
Why the Gap Between Them Matters
You might hear doctors talk about "pulse pressure." This is just the math of subtracting your diastolic from your systolic.
If your reading is 120/80, your pulse pressure is 40. A very wide gap—say, 190/70—can indicate that your heart is working extremely hard or that your valves aren't closing properly. On the flip side, a very narrow gap can sometimes mean your heart isn't pumping enough blood. It’s all about the rhythm and the resistance.
What’s "Normal" Anyway?
For years, the gold standard was 120/80 mmHg. (The "mmHg" stands for millimeters of mercury, a carryover from the days when we actually used liquid mercury in glass tubes to measure pressure).
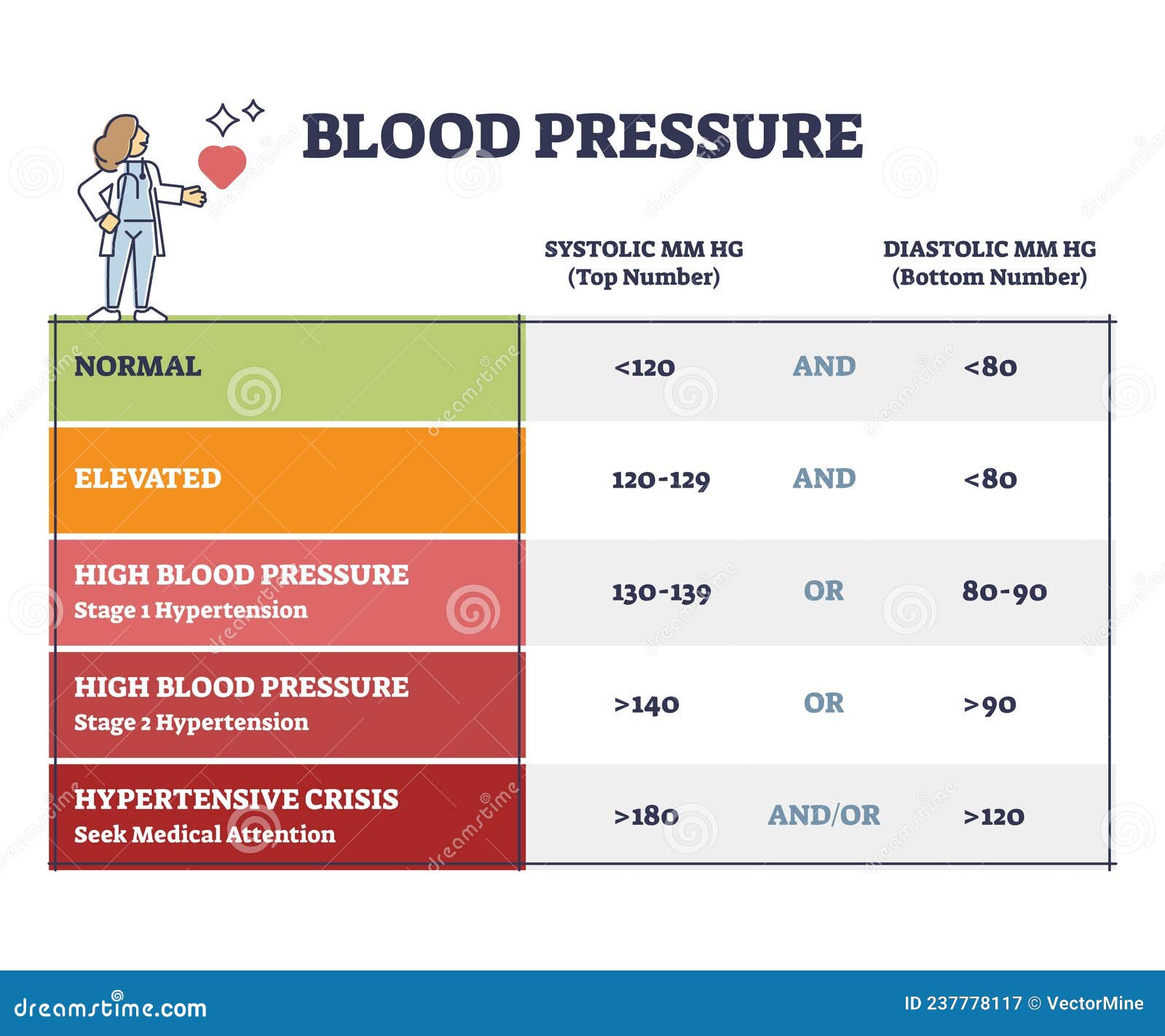
But in 2017, the American College of Cardiology and the AHA tightened the screws. They redefined high blood pressure. Now, "Elevated" starts at 120 systolic, and "Stage 1 Hypertension" kicks in at 130/80. This was controversial. Some critics felt it "medicalized" millions of healthy people overnight. However, the data from the SPRINT trial (Systolic Blood Pressure Intervention Trial) suggested that bringing pressure down lower than previously thought significantly reduced the risk of death and heart failure.
The "White Coat" and "Masked" Paradox
Ever notice your heart racing the moment you walk into a clinic? That’s White Coat Hypertension. Your blood pressure spikes because you're stressed by the environment.
💡 You might also like: Blackhead Removal Tools: What You’re Probably Doing Wrong and How to Fix It
Then there’s the sneakier version: Masked Hypertension. This is when your pressure looks great at the doctor's office but skyrockets when you're dealing with a deadline at work or an argument at home. This is why many cardiologists, like Dr. Eric Topol, advocate for home monitoring. One single reading in a cold office every six months tells you almost nothing about your average daily pressure.
You've gotta look at the trends.
The Stealthy Damage of High Readings
High blood pressure is called the "silent killer" for a reason. You usually can't feel it. You don't get a "pressure headache" until it's dangerously high—usually over 180/120, which is a hypertensive crisis.
What happens if you ignore what systolic and diastolic mean? The constant pounding damages the smooth inner lining of your arteries. This allows plaque to build up more easily. It’s a vicious cycle. The more plaque, the narrower the artery. The narrower the artery, the higher the pressure.
- Your Brain: High pressure can cause tiny vessels to burst (hemorrhagic stroke) or lead to vascular dementia.
- Your Kidneys: These are basically bundles of delicate blood vessels. High pressure shreds them over time, leading to kidney failure.
- Your Eyes: Retinopathy is common when the tiny vessels in the back of the eye can't take the heat.
Real World Factors That Mess With the Numbers
Salt is the obvious villain. It makes your body hold onto water. More water in the pipes equals more pressure. But it’s not just the salt shaker. Processed foods are the real culprits.
Stress is another. When you’re stressed, your body dumps cortisol and adrenaline. These hormones constrict your blood vessels and make your heart beat faster. If you’re chronically stressed, your "pipes" never get a chance to widen back out.
📖 Related: 2025 Radioactive Shrimp Recall: What Really Happened With Your Frozen Seafood
And let’s talk about sleep apnea. If you snore and stop breathing at night, your oxygen levels drop. Your brain panics and sends a massive surge of adrenaline to wake you up. This causes your blood pressure to spike wildly in the middle of the night—the time when it’s supposed to be at its lowest.
Practical Steps to Manage Your Numbers
Knowing the numbers is step one. Changing them is step two.
- Get a decent home monitor. Look for one that goes on your upper arm, not your wrist. Wrist monitors are notoriously finicky and often inaccurate if your arm isn't at the exact right level. Omron and Withings make some of the most reliable consumer models.
- The "Rule of 5." Sit quietly for five minutes before taking a reading. No talking. No scrolling on your phone. Feet flat on the floor. Back supported. If you just ran up the stairs or finished a coffee, your reading will be junk.
- The DASH Diet. This isn't just a buzzword. The Dietary Approaches to Stop Hypertension is backed by decades of NIH research. It’s heavy on potassium (potassium helps your body flush out sodium and relaxes blood vessel walls).
- Watch the "Dip." Your blood pressure should naturally drop by 10-20% at night. If it doesn't, that’s often a sign of underlying issues like the aforementioned sleep apnea or high salt intake.
Taking Action Today
Don't wait for your next annual physical to care about this. If you haven't checked your blood pressure in a year, go to a local pharmacy and use the machine, or better yet, buy a home cuff.
Keep a log for one week. Take your pressure once in the morning and once in the evening. This gives your doctor a "moving picture" rather than a "snapshot." If you see your systolic consistently creeping over 130 or your diastolic over 80, it’s time to have a real conversation about lifestyle tweaks or medication.
Understanding what systolic and diastolic mean isn't about memorizing medical jargon. It’s about recognizing the internal weather of your body. When you know the pressure is rising, you can take cover before the storm hits.
Start by checking your labels for sodium content today. Even reducing your intake by 1,000mg a day can significantly drop your systolic numbers within weeks. Your heart is doing the heavy lifting 24/7; the least you can do is give it a slightly easier job.