You’re sitting in that small, sterile exam room. The cuff squeezes your arm tight—maybe a little too tight—and then comes the hiss of escaping air. The nurse mutters two numbers and scribbles them down. If you see those numbers creeping toward the top of a blood pressure chart high range, your heart might skip a beat. Honestly, it’s stressful. But what do those numbers actually mean for your Friday night plans or your long-term health? It’s not just about "high" or "low." It’s about the pressure your blood exerts against your artery walls every single time your heart beats.
Most people think a single high reading means they’re in trouble. It doesn’t.
Blood pressure is fluid. It changes when you’re annoyed at traffic, when you’ve had too much coffee, or even if you really have to pee. To actually understand if you’re looking at a blood pressure chart high situation that requires medical intervention, you need to look at the trends. The American Heart Association (AHA) and the American College of Cardiology (ACC) updated their guidelines a few years back, and it sent a lot of people into a tailspin because suddenly, "normal" became a much smaller target.
Decoding the Blood Pressure Chart High Categories
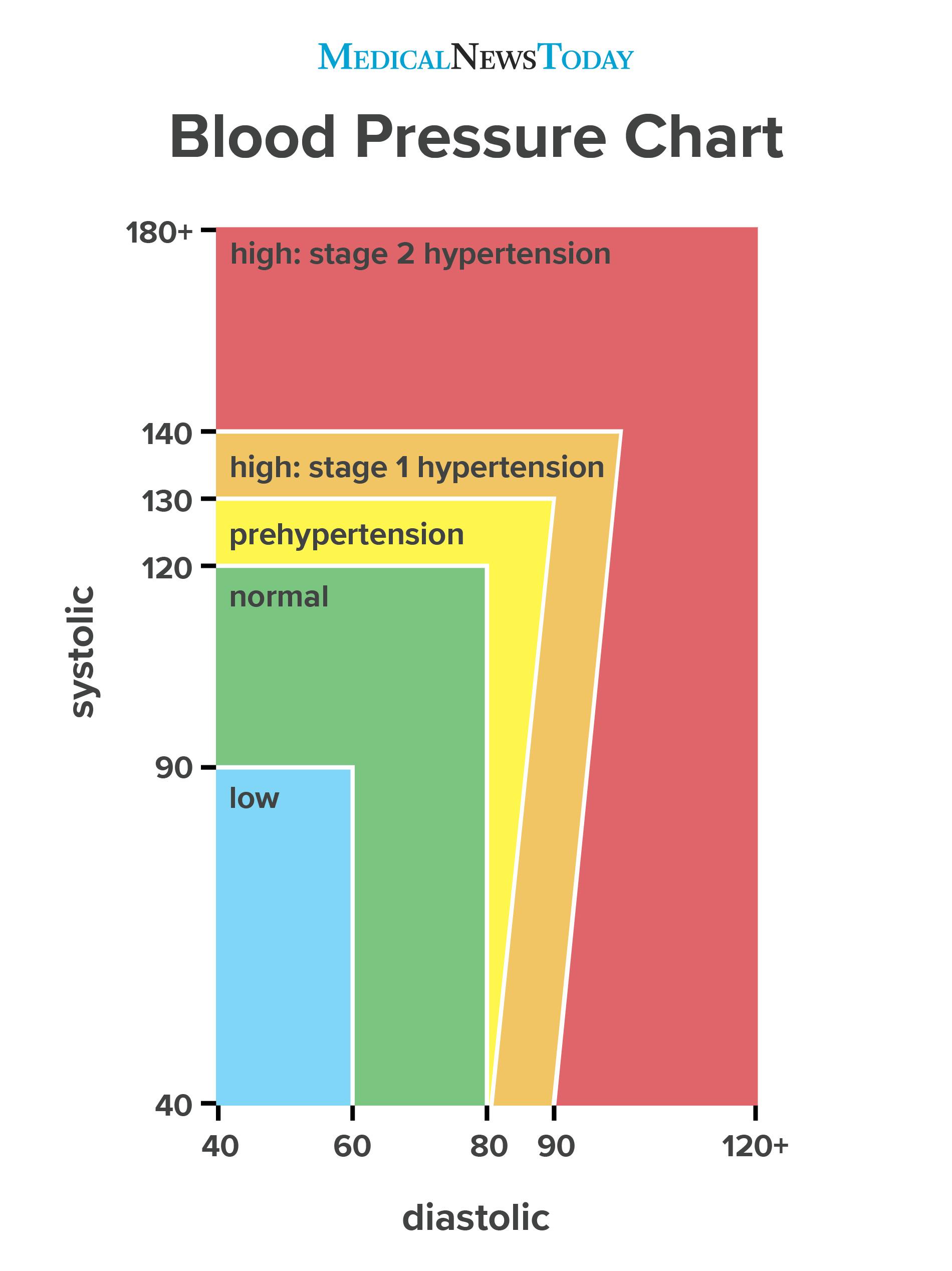
If your systolic number (the top one) is consistently over 130, or your diastolic (the bottom one) is over 80, you’ve officially entered the territory of Stage 1 Hypertension. It sounds scary.
For decades, the cutoff was 140/90. Then, a massive study called the SPRINT trial (Systolic Blood Pressure Intervention Trial) changed everything. Researchers looked at over 9,000 adults and found that bringing that top number down to 120 significantly reduced the risk of heart attacks and strokes. That's why the goalposts moved.
The Elevated Zone
This is the "yellow light" of heart health. Your top number is between 120 and 129, but your bottom number is still under 80. You aren't "sick" yet. But you’re drifting. If you don't change how you're eating or moving, you’re almost certainly headed for a diagnosis of hypertension within a few years. It’s a wake-up call, basically.
Hypertension Stage 1
Here, you’re looking at 130-139 over 80-89. Most doctors won't immediately reach for the prescription pad here unless you have other risk factors like diabetes or kidney disease. They’ll talk to you about salt. They’ll talk to you about walking.
Hypertension Stage 2
When the blood pressure chart high readings hit 140/90 or higher, the conversation changes. This is where the risk of "silent" damage to your organs starts to climb. Your arteries are becoming less like flexible rubber hoses and more like stiff pipes. Stiff pipes break.
📖 Related: Blackhead Removal Tools: What You’re Probably Doing Wrong and How to Fix It
The Hypertensive Crisis
If your monitor reads 180/120 or higher, stop reading this and call a doctor. Seriously. If you have chest pain, shortness of breath, or numbness alongside these numbers, it’s an emergency. This is the "red zone" where the pressure is so high it can cause immediate organ failure or a stroke.
Why "White Coat Syndrome" Is Ruining Your Data
Ever noticed your heart racing the second you walk into a clinic? That’s white coat syndrome. Studies suggest up to 30% of people diagnosed with high blood pressure based on office readings actually have normal pressure at home.
This is why home monitoring is a game changer.
When you check your pressure at home, you're in your natural habitat. You’re on the couch, not sitting on a crinkly paper sheet in a cold room. To get an accurate read on a blood pressure chart high trend, you need to follow the "rule of twos." Check it twice a day—once in the morning before meds or food, and once in the evening. Do this for a week. That average is worth ten times more than a single reading at the doctor’s office.
The Salt Myth and the Potassium Reality
Everyone blames the salt shaker. While it’s true that sodium makes you retain water—which increases blood volume and therefore pressure—it’s only half the story.
Most of us aren't getting enough potassium.
Potassium acts as a natural foil to sodium. It helps your kidneys flush out the salt and eases the tension in your blood vessel walls. If you’re staring at a blood pressure chart high reading, don't just put down the salt; pick up a banana, some spinach, or a baked potato. The DASH diet (Dietary Approaches to Stop Hypertension) isn't just some fad; it’s one of the most clinically proven ways to drop your numbers without drugs. It emphasizes magnesium, calcium, and potassium. It’s basically just eating like a human before processed food existed.
👉 See also: 2025 Radioactive Shrimp Recall: What Really Happened With Your Frozen Seafood
The Hidden Culprits: Sleep and Stress
You can eat all the kale in the world, but if you aren't sleeping, your blood pressure will stay high. Sleep apnea is a massive, often undiagnosed cause of hypertension. If you snore or wake up feeling like you haven't slept, your oxygen levels might be dropping at night. When that happens, your brain panics and sends a surge of adrenaline through your system to wake you up so you can breathe. That spike in adrenaline keeps your blood pressure elevated even during the day.
Stress is the other big one.
We aren't built for chronic stress. We're built for "a tiger is chasing me" stress, which is supposed to end quickly. Modern life is just one long, slow-motion tiger chase. Cortisol and adrenaline stay high, and your blood vessels stay constricted. Finding a way to "turn off" that sympathetic nervous system response is just as important as your morning jog.
Real Talk About Medication
There’s a weird stigma about blood pressure meds. People feel like they "failed" if they have to take a pill.
Think of it differently.
Sometimes your genetics just won’t cooperate. You can be a vegan marathon runner and still have a blood pressure chart high situation because your family tree decided your arteries should be a bit more stubborn. Medications like ACE inhibitors, beta-blockers, or diuretics aren't a "defeat." They are tools to prevent your brain from bleeding or your kidneys from quitting.
Actionable Steps to Lower Your Numbers Starting Today
If you’ve seen a high reading recently, don't panic, but don't ignore it either.
✨ Don't miss: Barras de proteina sin azucar: Lo que las etiquetas no te dicen y cómo elegirlas de verdad
First, get a validated home monitor. Look for one that’s been tested by the British and Irish Hypertension Society or a similar body. Wrist monitors are famously finicky; go for the bicep cuff. It’s more annoying to put on, but the data is actually usable.
Second, watch your "hidden" sodium. It’s not the salt you sprinkle on your eggs. It’s the salt in bread, canned soup, and salad dressings. Manufacturers use it as a preservative and a flavor carrier. Read the labels. If a serving has more than 400mg of sodium, maybe put it back.
Third, move for 30 minutes. You don't need to join a CrossFit gym. A brisk walk where you can still talk but would rather not is enough. Exercise makes your heart stronger. A stronger heart can pump more blood with less effort, which decreases the force on your arteries.
Fourth, check your waistline. This isn't about vanity. Visceral fat—the stuff around your organs—secretes inflammatory chemicals that directly mess with your blood pressure. Even losing five or ten pounds can result in a measurable drop in your systolic pressure.
Finally, limit the booze. It’s a bummer, I know. But more than one or two drinks a day can cause your blood pressure to climb over time. Alcohol also interferes with the effectiveness of many blood pressure medications.
Keeping an eye on a blood pressure chart high isn't about living in fear. It’s about maintenance. You wouldn't ignore the "Check Engine" light in your car for three years, right? Your body is giving you the same kind of signal. Pay attention to it now, and you won't have to deal with a breakdown later.
Consistent monitoring is the only way to know where you stand. If you haven't checked yours in a month, do it today. Sit quietly for five minutes first. Don't cross your legs. Keep your arm at heart level. If the number is high, take a breath, wait a few minutes, and try again. One data point is a fluke; a week of data is a map to your future health.