You're lying on the table. The gel is cold. You’re staring at the monitor, trying to make sense of the gray and white static that’s supposed to be your insides. If you've had a hysterectomy, that screen looks different now. It's weirdly empty, but not really. Most people expect a giant "hole" where their uterus used to be, but that's just not how human anatomy works. Your body is incredibly good at filling in the gaps.
Finding clear images uterus after hysterectomy or even just a solid explanation of what a sonogram shows post-op is surprisingly hard. Most medical sites show you the "before" or the "surgical procedure," but they rarely show you the "after." When the uterus is gone, the bladder and the bowel basically just shimmy over. They take up the lease on that vacant property.
It’s a bit like moving furniture. You take out the bulky sofa, and suddenly the armchairs have more room to breathe. But for many patients, seeing an ultrasound or an MRI after surgery can be jarring. You’re looking for a landmark that isn't there anymore. Honestly, it’s a lot to process emotionally and physically.
What actually shows up on those scans?
When a radiologist looks at images uterus after hysterectomy, they aren't looking for a ghost. They’re looking at the "vaginal vault" or the "vaginal cuff." This is the top part of the vagina that has been sewn shut. On a scan, it looks like a little blind pouch.
If you still have your ovaries—which many people do—they might not be in the same spot. Without the uterus to tether them, ovaries can drift. They might hang out higher in the pelvis or tuck themselves behind the bladder. This is one reason why an ultrasound technician might spend an extra ten minutes digging around with the transducer. They’re literally hunting for your "migratory" ovaries.
The bladder is the big winner here, space-wise. Without a heavy uterus sitting right on top of it, the bladder often expands. This is why some people find they don't have to pee every five minutes anymore, though others deal with temporary bladder spasms while the organ adjusts to its new neighborhood.
🔗 Read more: In the Veins of the Drowning: The Dark Reality of Saltwater vs Freshwater
The Vaginal Cuff: The New Landmark
The "cuff" is the star of the show in post-hysterectomy imaging. If you had a total hysterectomy (cervix removed), the surgeon closed the top of the vaginal canal. On an MRI or a CT scan, this appears as a linear structure. It shouldn't be thick. If a doctor sees "cuff thickening," they start asking questions. Usually, it's just scar tissue or "granulation tissue," which is basically the body's over-eager way of healing.
Dr. Mary Jane Minkin, a clinical professor at Yale, often notes that healing takes time—way more time than the six-week checkup suggests. Internally, the remodeling of the pelvic floor can take a full year.
Why images of the uterus after hysterectomy matter for long-term health
You might think you’re done with pelvic imaging once the organ is out. Not necessarily. Doctors still use these images to monitor for things like:
- Prolapse: Without the uterine ligaments, sometimes the bladder or bowel starts to sag. Imaging catches this early.
- Adhesions: This is basically internal spiderwebs. Scar tissue can bind the bowel to the vaginal cuff. It’s common, and it’s often why people feel "twinges" or pulling sensations months later.
- Ovarian Cysts: If you kept your ovaries, they still do ovary things. They can still develop cysts that need to be watched.
- Fluid Collections: Right after surgery, a "seroma" or "hematoma" (pockets of fluid or blood) might show up on an image. Most of the time, the body reabsorbs these, but doctors like to keep an eye on them.
It’s kinda fascinating how the body recalibrates. The small bowel—the ileum—usually drops down into the space where the uterus was. In medical terms, this is called "small bowel descent." It sounds scary, but it’s actually the standard "after" photo. Your guts are just finding a comfortable place to sit.
The "Empty Space" Myth
There is no vacuum inside you. Your abdominal pressure ensures that everything stays packed tight. If you look at a cross-section MRI, you’ll see that the space is filled with loops of bowel. This is why some people feel "bloated" or notice a change in their digestion post-surgery. Your intestines are literally settling into a new configuration.
💡 You might also like: Whooping Cough Symptoms: Why It’s Way More Than Just a Bad Cold
Sometimes, people worry that their other organs will "fall out." This doesn't happen because the pelvic floor muscles are still there. Think of them like a hammock. The hammock used to hold a bowling ball (the uterus); now it's just holding some lighter gear. But if the hammock was already weak, that’s when issues like prolapse show up on imaging.
Distinguishing between types of surgery
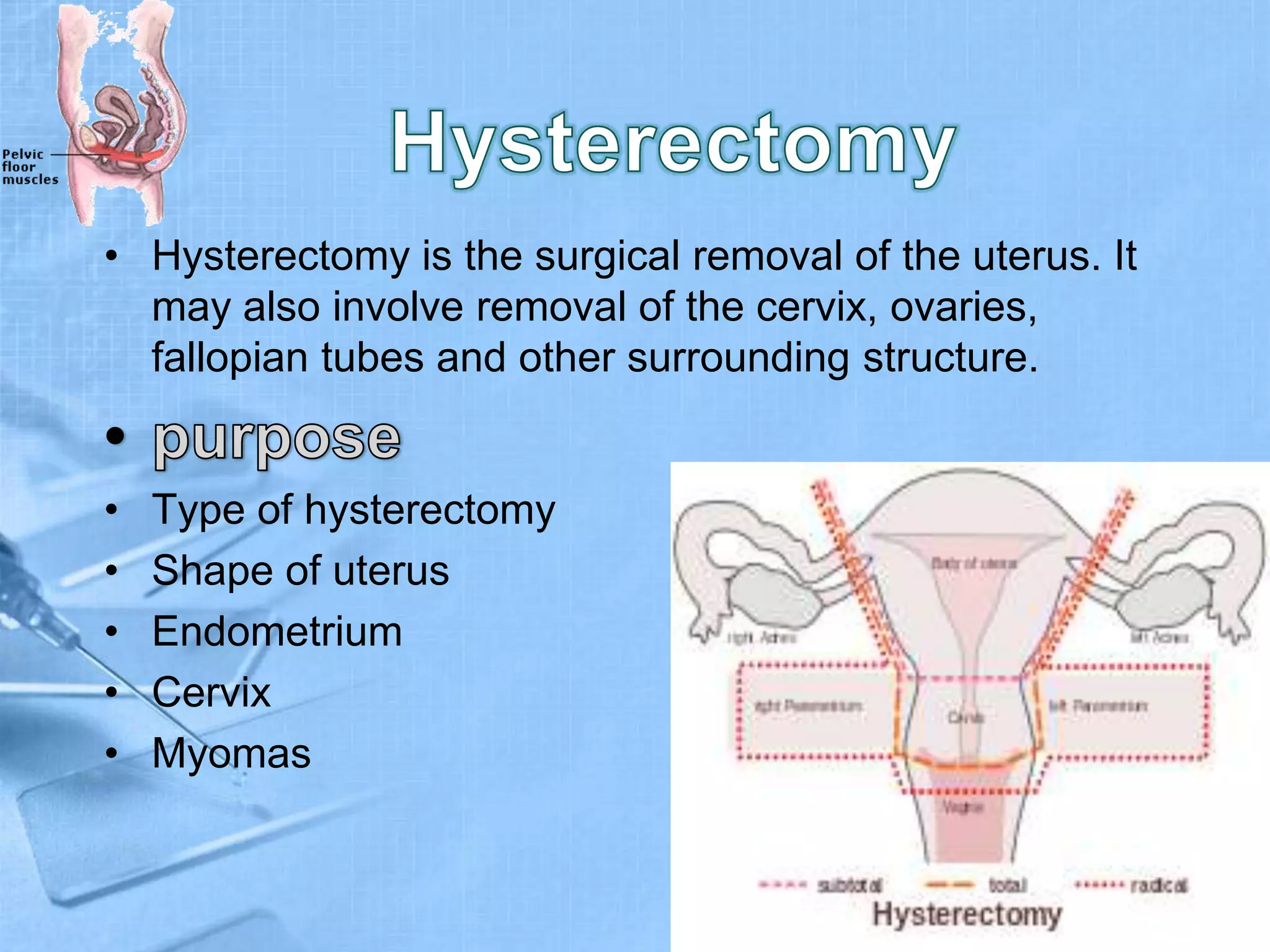
The images will look different depending on whether you had a partial or total hysterectomy.
- Supracervical (Partial): The cervix is still there. On an ultrasound, it looks like a small, nubby structure. It can actually be confusing for a technician who doesn't know your history; they might think it's a small uterus.
- Total: The cervix is gone. You’ll see the vaginal cuff.
- Radical: Usually done for cancer. This involves removing more surrounding tissue, and the "empty" space on the image will be more pronounced, often filled with more bowel loops.
How to read your own radiology report
If you’re looking at a report for images uterus after hysterectomy, you’re going to see some specific jargon. Here is the "translation" for the most common terms:
"Surgically absent uterus" – This is the most obvious one. It just means they couldn't find it because it’s gone.
"No adnexal masses" – They checked the area where your ovaries/tubes are (the adnexa) and didn't see anything weird.
"Vaginal vault unremarkable" – This is actually great news. "Unremarkable" is the favorite word of every patient. It means the top of your vagina looks healthy and healed.
"Free fluid in the pelvis" – A little bit is normal. A lot might mean inflammation or a very recent surgery.
Life after the image
Healing isn't just about what shows up on a scan. It’s about how you feel. Many women report a sense of relief when they see their "clean" scans. No more fibroids. No more adenomyosis. No more shadows that shouldn't be there.
📖 Related: Why Do Women Fake Orgasms? The Uncomfortable Truth Most People Ignore
But there’s a psychological component to seeing these images too. For some, seeing the "space" where a life-defining organ used to be can trigger a sense of loss. For others, it’s a visual confirmation of freedom from pain. Both are totally valid.
If you’re looking at your own images, remember that a snapshot in time doesn't tell the whole story. Your body is dynamic. It moves, it shifts, and it adapts.
Actionable Steps for Post-Hysterectomy Care
If you are currently navigating the "after" phase of surgery and are concerned about what’s happening inside, here is how to handle it:
- Request your CD or Portal Access: Don't just read the report. Look at the images. Ask your doctor to point out the vaginal cuff and your ovaries (if you have them). Seeing it makes it real and less scary.
- Monitor for Pelvic Pressure: If you feel a "bulge" or extreme pressure, it might not show up on a lying-down scan. Ask for a "dynamic" ultrasound or a physical exam if you suspect prolapse.
- Pelvic Floor Physical Therapy: This is the gold standard. Regardless of what the images show, your muscles need to relearn how to support your "new" internal layout.
- Keep a Symptom Journal: Images don't show pain. If you have twinges or "pulling" sensations, write down when they happen. This helps your doctor correlate your scan with your reality.
- Clarify Your History: Every time you get a scan—even for something unrelated like a kidney stone—tell the technician you’ve had a hysterectomy. It saves them time and prevents "false alarms" when they can't find your uterus.
The internal landscape changes, but it doesn't become a void. It becomes a new version of you. Understanding the anatomy of the "after" is the first step in feeling comfortable in your own skin again. If the report says everything is "unremarkable," take it as a win and keep moving forward.